Dermatovenerologist
Khasanova
Alina Rashidovna
8 years of experience
Make an appointment
Patients often consult a doctor complaining of inflammation in the red border or mucous membrane of the lips. In most cases, a specialist diagnoses “cheilitis”. This is the name for tissue inflammation, which manifests itself in the form of redness, peeling, the appearance of purulent crusts and weeping ulcers. Any attempt to open the mouth when eating or communicating causes sharp pain associated with tissue damage. Without proper treatment, the disease persists for a long time, causing the patient a lot of physical and aesthetic inconvenience. For young people, the prognosis after clinical treatment of cheilitis is completely favorable, but older patients may encounter its complications in the form of leukoplakia and the onset of the oncological process.
Exfoliative cheilitis
Exfoliative cheilitis was described in 1900 by HW Stelwagon, the name was proposed in 1912 by I. Mikulic and G. Kümmell. This is a chronic psychosomatic disease in which only the red border (intermediate part) of the lips is affected. In the pathogenesis of the disease, a certain role belongs to genetic and psychogenic factors. The implementation of the latter is carried out through the hypothalamus and the autonomic nervous system, the changes in which, according to R.I. Zalkiev, are very significant.
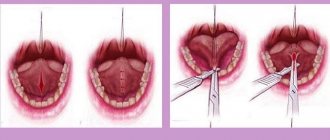
There are exudative and dry forms of exfoliative cheilitis. The histopathology of both forms is qualitatively similar, but with the exudative form the changes are more pronounced. In the epithelium of the red border of the lips (outer zone) there is parakeratosis (see), acanthosis (see), in the spinous layer and the layer of keratinizing epithelium there are large light cells. In the dermis, especially in the papillary and reticular layers, thickening of collagen fibers occurs, and a slight round cell infiltration is noted. A characteristic feature of exfoliative cheilitis is the spread of the process along the entire red border of the lips from corner to corner of the mouth, only a narrow strip of the red border bordering the skin remains unaffected. In the dry form of exfoliative cheilitis, gray or brownish-gray scales, reminiscent of mica, are formed in the affected area, tightly attached in the center and lagging along the periphery. Sometimes only the middle part of the red border of the lips is affected. The exudative form of cheilitis may be preceded by a dry form. In the exudative form of cheilitis, massive yellow or brownish-yellow crusts are first formed, after removal of which a smooth, dry, bright red, non-eroded surface is exposed. Then, a whitish sticky exudate appears on the red border of the lips and its inner zone (Klein’s zone), shrinking into crusts. Patients are bothered by a burning sensation and tightening of the lips. Due to lip sticking, patients try to keep their mouth half open. The course is long.
Diagnosis of exfoliative cheilitis is based on the characteristic localization of the process, a typical wedge, picture, and the absence of primary morphological elements. Exfoliative cheilitis should be differentiated from atopic cheilitis, contact and actinic cheilitis, lesions of the lips in pemphigus (see), lupus erythematosus (see).
When treating the exudative form, sedatives and antidepressants are prescribed, acupuncture is performed in the second (weaker) version of the inhibitory technique (see Acupuncture), ultraphonophoresis with corticosteroid ointments is used locally; in the dry form - acupuncture according to the first (stronger) version of the stimulating technique, fat-containing ointments.
The prognosis is usually favorable, spontaneous recovery is possible. No malignancy is observed. Prevention has not been developed.
Glandular cheilitis
Glandular cheilitis is characterized by the location of small salivary glands or their ducts in the outer and inner zones of the red border of the lips, their hyperplasia and hyperfunction. It can occur both primary and secondary (against the background of lip damage due to systemic lupus erythematosus, lichen planus, etc.). It usually appears in people over 30-40 years of age.
Histological examination reveals significant hypertrophy of the salivary glands, cystic expansion of their acini and ducts, and slight inflammatory infiltration.
When examined on the inner zone of the red border of the lips, and sometimes on its outer zone (usually on the lower lip), dilated mouths of the salivary glands are visible in the form of red dots, from which droplets of saliva are released in the form of dew.
The course of glandular cheilitis is torpid. When a secondary infection occurs, which is extremely rare, superficial or deep purulent glandular cheilitis develops, up to the formation of abscesses and fistulas. Occasionally, leukoplakia (see), which looks like thin rings, occurs around the dilated mouths of the salivary glands - the Puente-Acevedo form.
To identify glandular cheilitis, the patient’s lower lip should be slightly pulled back; after 20-30 seconds, droplets of saliva appear on the mucous membrane of the lip, released from the dilated mouths of the small salivary glands, which does not happen with other cheilitis.
Surgical treatment: removal or electrocoagulation of each salivary gland. Secondary glandular cheilitis disappears after resolution of the underlying disease.
The prognosis is favorable, however, irritation of the lip with saliva can contribute to the occurrence of cracks, erosions, precancerous diseases and cancer developing from the epithelium of the red border of the lip (see Lips).
2. Reasons
The etiopathogenesis of actinic cheilitis is not completely clear today, but it is obvious that the basis of this disease is a painfully aggravated reaction to the ultraviolet (the harshest and most dangerous) part of the solar spectrum. Sometimes actinic cheilitis is combined with other forms of photodermatosis.
Naturally, actinic cheilitis is characterized by a distinct seasonality: spring and summer, i.e. during periods of increased solar activity, the incidence of complaints described below increases sharply, and in the cold season, accordingly, decreases.
Visit our Dermatology page
Allergic contact cheilitis
Allergic contact cheilitis occurs as allergic contact dermatitis (see), develops as a result of sensitization of lip tissue to various chemicals. substances, for example, contained in lipstick. This cheilitis manifests itself as erythema of varying intensity, rarely - papulovesicular elements in the area of contact with the chemical, peeling of the red border of the lips, and sometimes the adjacent skin. Patients note a burning sensation on their lips.
The diagnosis of allergic contact cheilitis is established on the basis of anamnesis (contact with a chemical substance) and clinical symptoms. The diagnosis can be confirmed by skin testing with the suspected allergen. However, it should be borne in mind that there may be no parallelism in the sensitivity of the skin and the red border of the lips to sensitizing factors.
Treatment consists of eliminating the effect of the sensitizing factor and prescribing hyposensitizing agents; prednisolone ointment and emollient creams are applied topically.
The prognosis is favorable. Prevention consists of preventing re-sensitization.
Meteorological cheilitis
Meteorological cheilitis, described by A.L. Mashkilleyson (1970), is a non-allergic inflammatory disease of the lips that occurs as a result of the action of various meteorological factors (low humidity, wind, cold, insolation, dust, etc.). It is observed mainly in men who work outdoors, and is most often localized on the lower lip.
Histological examination reveals diffuse uneven hyperplasia of the epithelium of the red border of the lips, in places with slight keratinization. The stroma is infiltrated, there is thickening and homogenization of elastic fibers. The red border of the lower lip is unevenly congestively hyperemic, somewhat infiltrated, and in places tightly packed scales are formed.
The course is chronic, independent of the time of year, there is no sensitization to sunlight. In contrast to systemic lupus erythematosus (a form without clinically pronounced atrophy), meteorological cheilitis does not have a sharp border of erythema and keratinization at the periphery of the lesions, which has the appearance of a palisade, and treatment with synthetic antimalarial drugs does not produce results (for lupus erythematosus, these drugs have a positive effect).
The main thing in treatment is the elimination of external adverse influences. In addition, vitamins (B2, B6, B12), local photoprotective creams (see Photoprotective agents), and prednisolone ointment are prescribed.
Meteorological cheilitis is an optional precancer with a slight potential malignancy, but against its background obligate forms of precancer (warty precancer, limited hyperkeratosis, etc.) may arise, which significantly worsens the prognosis. Prevention consists of protecting lips from damaging meteorol. factors.
4.Treatment
Like all allergic reactions, actinic cheilitis is best treated by avoiding contact with the allergen. In this case, however, this is most often not possible.
Special vitamin complexes are prescribed (mainly groups A, B and E), and corticosteroid hormonal drugs are used according to indications to eliminate local inflammation. Sometimes antimalarial drugs are used in treatment, which also show an effect in actinic cheilitis.
Patients are strongly recommended to use special photoprotective creams and ointments.
Actinic cheilitis
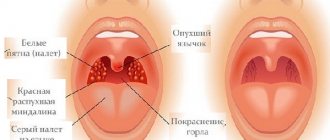
Actinic cheilitis, described in 1923 by S. Aures, develops as a result of sensitization of the red border of the lips to sunlight and can be combined with solar eczema of the face. The process occurs and intensifies in the spring-summer period; in winter, the rashes disappear without a trace. Histologically, the picture of allergic contact dermatitis is determined (see). There are two forms of actinic cheilitis - dry and exudative. In the dry form, the lower lip becomes bright red, covered with small scales, and sometimes verrucous formations appear. In the exudative form, the lip is hyperemic, swollen, small, quickly opening blisters, weeping, crusts, and bleeding painful cracks appear. Patients are bothered by burning and itching.
To establish the diagnosis of actinic cheilitis, the connection of the disease with insolation, the onset of its development in the spring, and localization on the lower lip are of primary importance.
During treatment, synthetic antimalarial and hyposensitizing agents are used, corticosteroid ointments and photoprotective creams are used topically (see Photoprotective agents).
The prognosis is aggravated by the possibility of developing obligate precancer and squamous cell carcinoma against the background of actinic cheilitis. Prevention of relapses involves protecting the lips from sun exposure.
Clinical manifestations of cheilitis
Cheilitis is divided into the following types:
- Exfoliative.
- Glandular.
- Contact allergic.
- Meteorological, or actinic.
- Atopic.
- Macrocheilitis.
- Hypovitaminosis.
Clinical manifestations of cheilitis vary depending on the type of disease.
Exfoliative cheilitis affects the red border of the lips. The first clinical symptom is peeling. The nature of the disease is not completely clear to specialists, but the authors noted a connection between cheilitis and psychological or neurological disorders: thyrotoxicosis and anxiety-depressive syndrome. Patients complain of anxiety and unreasonable worry. A connection between the disease and hyperfunction of the thyroid gland has also been revealed. Most often, the disease is diagnosed in females.
Experts distinguish two forms of the disease exfoliative cheilitis: dry and exudative. The first is not marked by an inflammatory process and is more common in young people.
The exudative form of the disease is more often observed in middle-aged and elderly people. Patients complain of inflammation, swelling, pain, inability to open their mouth wide, difficulty speaking and eating.
Peeling is found on the red border of the lips, it does not spread to the skin and mucous membrane, and the areas bordering the skin and the area of the corners of the mouth remain free.
Symptoms of exfoliative cheilitis are dry skin, burning, and scaling. The patient often bites them off or removes them with his hands, since this process is painless. A bright scarlet surface remains in place of the removed scales; no erosion is observed. After 5-7 days after removal, the scales form again.
This type of cheilitis has a long, sluggish course, with periods of remission and further exacerbations. The disease cannot be cured on its own; qualified assistance from a specialist is required. When examining a patient, the doctor notes dry lips, identifies scales that at the beginning of the process look like mica, and then are tightly fused with a red border. The edges of the red border look raised due to the presence of scales.
Granular cheilitis was first described in 1870. Its pathogenesis involves congenital or acquired proliferation of small salivary glands, which provokes their infection. There are two types of this disease:
- Primary granular cheilitis.
- Secondary granular cheilitis.
This disease affects people of both sexes, mainly after the age of 30, and it is noted that damage to the lower lip occurs in patients twice as often. Patients with chronic periodontal diseases, tartar and caries are at risk, as they contribute to infection of the dilated ducts of the salivary glands.
A direct connection has been established between the occurrence of primary granular cheilitis and the presence of a congenital anomaly in the functioning of the salivary glands. The salivary glands hypertrophy under the influence of various factors (dental pathology, periodontal disease, pathology of the dentition, gums, etc.), and the intensity of saliva production increases. According to one of the scientists' hypotheses, the appearance of the disease may be influenced by heredity.
Characteristic of secondary granular cheilitis is the fact that the resulting inflammation affects the glandular tissue. However, these are not typical cases.
Granular cheilitis has a specific clinical picture; its characteristic signs are red dots - dilated mouths of the salivary glands, from which drops of saliva are released (the “dew drops” symptom). The main complaints of patients are the presence of dryness, erosions and cracks. Dryness occurs due to the constant moistening of the lips with saliva and its evaporation. Then the skin of the lips gradually undergoes keratinization, starting from red dots and spreading further. If the disease lasts for a long time and cracks appear, this may be a harbinger of the formation of pre-cancer lesions. The resulting cracks can remain forever, as the elasticity of the skin of the lips is impaired.
A pyogenic (purulent) infection often penetrates the ducts of the salivary glands. Symptoms of granular cheilitis in purulent form are marked by swelling, pain, discharge of pus, and covering the lip area with thick crusts that are black-brown and yellowish-green in color. If the ducts of the glands are blocked, abscess formation may begin.
Contact allergic cheilitis is a clinical manifestation of a delayed type of allergic reaction to substances in contact with the lips. Often the causes of this disease are lipsticks, the plastic of dentures, and the toothpaste used. More often, female representatives suffer from contact allergic cheilitis. This disease can also develop as a result of bad habits (chewing pencils or pens) and the professional need to interact with metal objects for a long time (for example, mouthpieces of wind instruments). Patients complain of severe itching, swelling, redness of the lips and a burning sensation. After contact with an allergen, the symptoms of cheilitis become even more pronounced.
The pathological process is located in the area of the red border of the lips and rarely involves the skin around the lips. Sometimes the lesion is localized on the oral mucosa along with the main location of cheilitis. Erythema of varying intensity develops at the site of contact with the allergen. The following chain is visible: the beginning of the inflammatory process, the formation of small bubbles, the opening of small bubbles, the occurrence of cracks and erosions.
Meteorological, or actinic cheilitis, refers to inflammatory diseases of the lips. It is directly related to the influence of adverse meteorological factors on the body, these include:
- low or high humidity;
- solar radiation;
- dustiness of the air (wind, cold).
It is important how long a person is exposed to these factors, what is the structural feature of his skin.
Patients with meteorological cheilitis have some common features: delicate white skin, skin diseases (seborrheic eczema, seborrhea, diffuse neurodermatitis). The course of the disease does not depend on the time of year; it is chronic. As practice shows, this pathology most often affects men aged 20 to 60 years.
Actinic cheilitis develops due to a delayed allergic reaction to exposure to ultraviolet rays. In some cases, in addition to lesions of the lips, solar eczema of the face may be diagnosed. The disease has a seasonal course: exacerbations are observed in spring and summer, and remission in autumn and winter.
Experts distinguish two forms of actinic cheilitis:
- Dry.
- Exudative.
A symptom of the first form is dryness of the lower lip. Violations rarely affect the skin of the face and upper lip. The entire area of the red border is affected, it acquires a bright red color, and is covered with dry small scales of silvery-white color. Further erosions and abrasions may occur. Some patients may develop areas of hyperkeratosis and verrucous growths.
With the exudative form, the area of the red border swells, small bubbles, crusts, and weeping erosions form. Patients complain of burning, itching and soreness.
The clinical picture of meteorological cheilitis is characterized by dryness and the formation of scales on the lip, cracks and erosions. Patients feel tightness, dryness and notice flaking.
Atopic cheilitis is one of the manifestations of neurodermatitis or atopic dermatitis. The disease affects representatives of both sexes, most often in adolescence.
Allergic predisposition is an important pathogenetic link of this disease. Food products, medicines, household and flower dust, cosmetics, microorganisms and their toxins can act as allergens.
Patients diagnosed with atopic cheilitis complain of redness of the lips, accompanied by itching, peeling of the red border of the lips, and characteristic damage to the corners of the mouth. During remissions and subsidence of the acute process of the disease, lichenification (thickening of the skin and increased skin pattern) and peeling are noted. Cracks appear due to constant dryness and infiltration of the corners of the mouth.
Macrocheilitis is part of the Melkerson-Rossolimo-Rosenthal syndrome. Experts identify three main symptoms:
- Facial nerve paralysis.
- Macrocheilitis.
- Folded tongue.
More often, female representatives suffer from this disease. Hereditary predisposition and infectious-allergic factors are of great importance in the pathogenesis of this complex. This disease occurs with a recurrent nature and with a sudden improvement in well-being.
Patients complain of lip enlargement, itching, swelling, spreading to other areas of the face and existing for a long time. In places of swelling, the skin has a bluish-pink tint and is shiny. One or both lips, eyelids, cheeks, and other areas of the face in the area of innervation of the facial nerve are affected. Neuritis manifests itself in the form of a skewing of the face in the healthy direction, while the nasolabial fold is smoothed out.
Diagnosis of Melkerson-Rosenthal syndrome can be difficult due to not showing all the symptoms of the triad.
Hypovitaminous cheilitis develops in the case of a lack of B vitamins in the human body; deficiency of vitamin B2 is especially pronounced. The oral mucosa is dry, the patient feels a burning sensation on it, as well as on the tongue and lips. Upon examination, the doctor notes swelling and redness of the mucous membrane, fine scaly peeling and small vertical cracks on the red border of the lips, bleeding and painful. The skin of the lips is dry and red. The tongue is enlarged in size, and teeth marks are clearly visible on it.
A complication of this type of cheilitis may be the development of glossitis. With it, atrophy of the nerve papillae begins, the surface in the area of the back of the tongue can become smooth, acquire a bright scarlet color, and the process of hypertrophy of the fungiform papillae begins.
Abrasive precancrosis cheilitis Manganoti
Abrasive precancrosis cheilitis of Manganoti, described in 1933 by G. Manganotti, is an obligate precancerous disease of the lower lip, usually found in elderly men. A certain role in the occurrence of abrasive precancrosis cheilitis belongs to the influence of meteorological factors, injuries (mechanical, chemical), changes causing circulatory disorders in the lip, etc.
Histological examination reveals limited proliferation of the epithelium with symptoms of discomplexation and atypia, especially in deeply proliferating epithelial outgrowths. In the central part of the proliferation focus, an epithelial defect filled with a thick infiltrate is found. One or two superficial deep red erosions with a smooth surface appear on the red border of the lower lip, and sometimes crusts form. In approximately half of patients, erosion is located on a slightly inflamed base.
The course of the disease is chronic, erosions can heal, but then reappear in the same or another place.
Abrasive precancrosis cheilitis may be similar to pemphigus (see), herpetic erosion (see Herpes), erosive and ulcerative form of lichen planus (see Lichen planus), lupus erythematosus (see), erosive leukoplakia (see), etc. ., with which it should be differentiated.
To exclude malignancy, clinical signs may be absent; a pathohistological or cytological examination is performed.
Treatment includes sanitation of the oral cavity, oral administration of vitamin A, B vitamins, methyluracil, theonicol; Corticosteroid ointments and methyluracil ointment are used externally. If there is no effect from conservative therapy within 2 months, the lesions are excised.
Surgery usually leads to recovery. Malignancy of erosions is possible, which worsens the prognosis. Prevention consists of sanitizing the oral cavity, timely prosthetics, and eliminating mechanical and chemical injuries to the lip.
Treatment of the exudative form of exfoliative cheilitis
Local treatment of the exudative form of exfoliative cheilitis :
1) sanitation of the oral cavity, professional hygiene;
2) rational oral hygiene;
3) applications of keratoplasty, as well as solcoseryl dental adhesive paste 3-4 times a day;
4) applications of corticosteroid ointments - prednisolone or hydrocortisone - 3-4 times a day for 20 minutes;
5) blockade with a 2% solution of lidocaine or a 2% solution of trimecaine 2-3 ml as infiltration anesthesia into the lower and upper lips every other day, No. 7-10; 6) border rays of Bukki - 200 R 2 times a week, for a course of treatment 1600-3000 R. Before the session, remove the crusts, 1 course every 6 months.
General treatment:
1) sedatives and tranquilizers, until complete recovery, doses are selected individually;
2) psychotherapy - hypnosis, auto-training, electrosleep, relaxation;
3) acupuncture;
4) multivitamins with microelements - supradin, unicap-M, panhexavit, glutamevit, oligovit, etc.;
5) drugs that increase the body’s reactivity - pyrogenal according to the scheme, starting from 50 MTD, after 2 days the dose is increased to 150 MTD and then increased to 1000-1500 MTD (minimum pyrogenic doses), the course of treatment is 7-10 days;
6) gamma globulin or histaglobulin 2 ml 2 times a week, No. 5-7.
Did you like the article? Share with friends
0
Similar articles
Next articles
- Glandular cheilitis
- Contact allergic cheilitis
- Meteorological cheilitis
- Actinic cheilitis
- Atopic cheilitis
Previous articles
- Cheilitis
- Candidiasis in the oral cavity
- Herpes in the mouth
- Pemphigus in the mouth
- Lichen planus in the oral cavity
Atopic cheilitis
Atopic cheilitis is one of the symptoms of atopic dermatitis (see Neurodermatitis), often at certain stages of the disease it is its only manifestation. This lesion of the lips was previously mistakenly called eczematous, microbial, seborrheic cheilitis, eczematid, etc.
With atopic cheilitis, the red border and certainly the skin of the lips are affected, and most intensely in the area of the corners of the mouth. The part of the red border that passes directly into the mucous membrane of the lips remains unaffected; the process never spreads to the mucous membrane of the mouth. Damage to the lips begins with itching and the appearance of erythema, which has fairly clear boundaries; sometimes there is slight swelling of the skin and the red border of the lips, then licheialization of the lips occurs. The red border is infiltrated and peeling is noted. its entire surface is as if cut through by thin radial grooves and resembles a harmonic. In summer, the rashes usually disappear, but the skin in the area of the corners of the mouth remains infiltrated. which contributes to the formation of small cracks.
Atopic cheilitis is similar to foliative, actinic and allergic contact cheilitis, lupus erythematosus of the lips, with which it must be differentiated. Lupus erythematosus of the lips, in contrast to atopic cheilitis, is characterized by hyperkeratosis, snow-white glow of scales in the rays of a Wood's lamp, cicatricial atrophy, and absence of itching. In some cases, differential diagnosis of atopic cheilitis with symmetrical streptococcal and candidal infections is difficult. But with seizures, the process is localized only in the corners of the mouth and, as a rule, there is no lichenification (see Candidiasis, Pyoderma).
Treatment is aimed at eliminating the underlying disease (see Neurodermatitis). Corticosteroid ointments, pastes and ointments that have antipruritic and anti-inflammatory properties are used locally; in persistent cases, Bucca rays are used (see X-ray therapy). The prognosis is usually favorable.