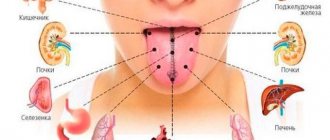
At home, you can conduct a quick health diagnosis yourself. All that is necessary for this is to examine the tongue with a mirror. A change in its color and shape will tell you a lot about the functioning of internal organs. This simple method should not be neglected. With its help, you can prevent the development of dangerous pathologies in time. Some of them are indicated by a rough tongue.
Tongue is an indicator of health
It is recommended to examine the tongue in the morning, on an empty stomach. In a healthy person, its color is pale pink, and the taste buds are easily distinguishable. Normally, it has a faint whitish coating that can be easily removed with a toothbrush or a special scraper. The complete absence of such cover should be no less alarming than its excessive amount.
Any changes that occur in the oral cavity should attract a person’s attention. They may indicate the formation of pathological processes in the body. A decrease in the amount or complete cessation of saliva production leads to the development of severe dry mouth. A rough tongue will immediately signal this to a person, since due to a lack of moisture on its surface, difficulties will arise when swallowing and chewing food.
Dry tongue can occur with severe nervous excitement or stress. From a physiological point of view, this is a normal situation. As soon as the person calms down, saliva production returns to normal. If there have been no emotional upheavals, and dryness has been observed for a long time, you should look for other causes of a rough tongue. An experienced doctor will help in this situation.
The causes of dry tongue may be the following:
- dehydration and intoxication;
- heart pathologies;
- tongue burn;
- disorders of the gastrointestinal tract;
- glossitis;
- chronic tonsillitis;
- liver pathologies;
- stagnation of food;
- blood diseases;
- HIV;
- kidney problems;
- long-term use of antibiotics;
- inflammation of the salivary glands, as well as their malignant and benign tumors;
- diabetes;
- infectious lesions.
Despite the impressive list of pathologies that cause roughness and dryness of the tongue, diseases of the gastrointestinal tract, pulmonary system, and infections are most often diagnosed. Only a doctor can make a correct diagnosis after a thorough diagnosis. He will prescribe treatment that will help defeat the underlying disease. After this, the rough tongue will definitely return to normal.
Xerostomia: causes
As a rule, the causes of xerostomia are “hidden” not in the salivary glands themselves, but in a disease of any system of the body or a general infectious disease. This condition is mainly caused by:
- Infectious diseases: tonsillitis, tuberculosis, HIV, tonsillitis, mumps (aka “mumps”, an infectious disease of the parotid salivary glands).
- Hypertension or severe iron deficiency anemia.
- Rheumatoid arthritis, as well as some diseases of the endocrine system: thyrotoxicosis (occurs when the thyroid gland is damaged), diabetes mellitus (develops when the function of the pancreas is impaired), sialadenitis (inflammation of the salivary glands themselves).
- Head or neck injuries, constant mouth breathing due to injury to the nose or the formation of polyps in the sinuses.
- Long-term use of certain groups of medications, dehydration with prolonged fever or vomiting.
- Bad habits: drinking alcohol, smoking, drug use.
The functions of the salivary glands are not necessarily impaired in all of these diseases and conditions, but if a person has xerostomia, they will be considered as possible causes.
Pathologies of the digestive tract
Reflexes that can influence the motor and secretory functions of the stomach and intestines are produced by tongue receptors. The opposite effect also occurs. That is, internal organs influence the appearance of pathological reflexes on the surface of the tongue. For example, its rough root and white coating will tell the doctor that the patient suffers from gastritis with low acidity. Pain and burning sensations in the esophagus, heartburn can complement the clinical picture.
A rough tongue covered with a gray coating may indicate the development of an intestinal ulcer. An additional factor indicating this pathology is heartburn and a burning sensation in the mouth.
Colitis, in addition to roughness, is characterized by an increase in the size of the tongue; teeth marks may even remain along its edges. With duodenitis and biliary dyskinesia, the thickness of the plaque increases significantly. A slight roughness of the tongue rarely causes discomfort. But a dense coating can negatively affect the sense of taste, reducing the sensitivity of the papillae.
Glossitis - symptoms and treatment
Folded or scrotal tongue. The term “scrotal tongue” comes from the external similarity of the affected tongue to the skin of the scrotum (from the Latin scrotum - scrotum). With this form of glossitis, a deep central groove runs along the back of the tongue with adjacent cracks and folds, which can be located longitudinally or randomly. The tongue is slightly enlarged [5]. Due to atrophy of the filiform papillae, it may look “smoothed out”, but this does not affect the taste sensation [16].
Diamond-shaped or median glossitis. This is a chronic disease of the mucous membrane of the tongue with partial or complete absence of filiform papillae closer to the posterior third of the tongue. The lesion has a diamond shape, a dense texture and a red varnished color. Usually it has clear contours and does not protrude above the mucous membrane. The lesion does not cause pain, but some patients perceive it as an aesthetic defect.
Other forms of rhomboid glossitis are less common - with tuberous outgrowths and papillomatous growths. The patient then feels the presence of a foreign body on the tongue [5][16].
Desquamative or “geographical” language. With this form of glossitis, the keratinization of the tongue is partially disrupted with signs of desquamation of the epithelium - desquamation (Latin desquamo - remove scales). The papillae of a significant part of the surface of the back of the tongue are changed. The lesions take on the appearance of red spots with a diameter of 0.5 cm and desquamated whitish epithelium along the edges. The spots can merge with each other and create a pattern similar to a geographical map.
Patients often complain of pain and burning when eating food or drinks that irritate the oral mucosa, and some of them note a short-term loss of taste.
There are two forms of desquamative glossitis: migrating and fixed [16].
The fixed form is more common with moderate damage to the stomach by the bacterium Helicobacter pylori. The disease is usually accompanied by persistent atrophy and smoothness of the filiform papillae of the tongue. The size and location of the lesions does not change.
The migratory form occurs when the stomach is heavily colonized with H. pylori. Foci of desquamation are up to 2 cm in diameter, their location is constantly changing.
Also, with desquamative glossitis, the tongue may increase in volume due to inflammation of the fungiform papillae, which are located at its root. They reach 0.8 cm in diameter and are covered with a white or light gray dense coating [14].
Black "hairy" tongue. This is a rare lesion in which the keratinized epithelium of the filiform papillae located in the posterior and middle third of the dorsum of the tongue does not slough off. Because of this, the papillae acquire a brown or black color, become stiffer, grow up to 2-3 cm, and are covered with a coating ranging from green and light brown to black [16].
The tongue takes on an unaesthetic appearance, patients complain of the sensation of a foreign body in the mouth and the appearance of a gag reflex [4].
Diseases of the gastrointestinal tract. A sign of damage to the gastrointestinal tract is a grayish-white coating on the back surface of the back of the tongue. There are no pain or any other subjective sensations.
Another manifestation of gastrointestinal tract damage is swelling of the tongue with tooth marks on its lateral surfaces without visible relief disturbances. At the same time, patients may be bothered by constant biting and burning when eating hot and spicy foods. The fungiform papillae located at the root of the tongue may also enlarge. They become bright red and rise above the surrounding tissue. The listed symptoms may accompany gastritis, gastric and duodenal ulcers[5].
With hepatitis A, areas of desquamation appear on the back of the tongue. Due to atrophy of the filiform papillae, the tongue becomes smooth and red. Patients often complain that the taste of sweet and bitter foods has become less pronounced [5].
Liver cirrhosis is manifested by swelling of the sublingual veins, atrophy of the oral mucosa and deepening of the natural folds of the tongue.
Lesions of the pancreas. In acute pancreatitis, the tongue becomes covered with a yellow-white coating, and the filiform papillae increase in size. Patients are often concerned about its dryness and disturbances in taste sensitivity.
In chronic pancreatitis, a secondary deficiency of B vitamins occurs, which is manifested by pain in the tongue and protruding bright red fungiform papillae. The tongue increases in size, becomes smooth and shiny.
Cardiovascular pathology. With hypertension, blisters with bloody contents are often present on the tongue, the so-called “vesical” symptom. They can suddenly appear and burst on their own, damaging the epithelium.
Diseases of the endocrine system. With diabetes, the body is dehydrated, so dryness appears, and the vessels of the tongue become overfilled with blood. A burning sensation occurs and long-healing ulcers form. Very often, symptomatic candidiasis is found on the tongue, especially if the patient does not regulate blood glucose levels.
Insufficient function of the thyroid gland, or hypothyroidism, leads to enlargement of the entire tongue or part of it and swelling, which does not form a dimple when pressed. Due to high cholesterol levels, the tongue is slightly yellowish in color.
Diseases of the blood and hematopoietic organs. With iron deficiency anemia, there is a need to eat unusual substances, such as chalk, clay, as well as a burning sensation and pain in the tongue. It is often pale in color and slightly increased in size.
With Addison-Beermer anemia, which occurs due to impaired absorption of vitamin B12, the filiform muscles weaken. The tongue becomes smooth and as if “polished”. This condition was called “Gunter's glossitis.” Painful red inflammatory streaks and spots appear. The tongue or just its tip turns bright red, and a tingling and burning sensation occurs [5].
Acute leukemia is manifested by ulcers of irregular shapes without clear boundaries with a necrotic coating on the tongue, without rims of hyperemia (overflow of blood vessels) along the edges. Pinpoint and small blood spots and hematomas may also appear on the mucous membrane of the tongue. One of the main symptoms of this condition is heavy bleeding.
Chronic leukemia occurs much less frequently than acute leukemia and lasts longer. Characteristic ulcers and leukemic infiltrates (fluid accumulation) appear on the tongue. At the acute and chronic stages of leukemia, they lead to the formation of ulcerative-necrotic lesions, which are difficult to treat.
Agranulocytosis is characterized by a significant decrease in the blood of granulocytes - a type of leukocyte, “protective” blood cells. The disease manifests itself as non-demarcated ulcers on the tongue and, unlike acute leukemia, an inflammatory reaction around them. Due to decreased immunity and the resulting increased susceptibility of the body to fungal diseases, candidiasis may develop.
Changes in the tongue due to hypo- and avitaminosis:
- hypovitaminosis A - dryness of the mucous membrane of the tongue and a tendency to increased keratinization of the skin (hyperkeratosis);
- hypovitaminosis C - swelling of the tongue with teeth marks on it; ulcerative necrotic lesions, usually covering a significant surface area of the tongue mucosa;
- hypovitaminosis PP causes a disease called “pellagra”, in which peeling of the surface layers of the epithelium occurs and a burning sensation of the tongue, it becomes smooth, shiny and crimson - the so-called “cardinal tongue”;
- hypovitaminosis B1 is characterized by pain in the tongue and the appearance of blisters;
- hypovitaminosis B2 is manifested by burning of the tongue, atrophy of the papillae and angular cheilitis - cracks in the corners of the mouth [4].
When infected with herpes simplex virus type 1 (HSV-1), patients complain of burning pain in the tongue. Upon examination, a deep crack is visible along its midline with several branches. In their depths there are painful blistering rashes, which over time burst with the formation of erosions.
Burning mouth syndrome. In the area of the tongue there is a feeling of a burn, paroxysmal burning pain, which intensifies with overwork and stress.
Galvanism. Patients experience a metallic taste in the mouth and rawness. Upon external examination, the tongue is swollen, its vessels are filled with blood, “bald spots” of the papillae and bright red erosions appear on its sides [5].
Diseases of the pulmonary system
A white, rough tongue occurs in patients at an early stage of the development of diseases of this organ. Inflammation in the bronchi is indicated by a thick and dry plaque located at its tip. If it begins to thicken and acquire a yellow tint, this will tell the doctor that the pathology is progressing. Additionally, the patient will experience other symptoms. For example, weakness, unpleasant odor and dry mouth.
Characteristic changes in the condition of the tongue are observed in pathologies such as scarlet fever. First, an extensive yellow or gray-white coating forms. It thickens every day. The fungiform papillae are clearly visible under the plaque. They are distinguished by a rich red color and are surrounded by a white border. After a week, the plaque disappears, and the tongue changes color to crimson.
Oral mucosa: what to pay attention to
Regular dental examinations are an important part of the prevention of not only dental and periodontal diseases, but also pathologies of the oral mucosa. They make it possible to detect cancer, leukoplakia, stomatitis and other dangerous diseases in the early stages.
Inspection algorithm
The American Dental Association recommends that your oral examination include the following steps:
- a thorough visual examination of the lips, buccal mucosa, gums, anterior part of the tongue, floor of the mouth and palate;
- examination of the throat (pharynx), including tonsils, root of the tongue;
- palpation of the jaw and neck to detect nodes, tumors, any abnormalities or abnormalities.
This procedure allows you to timely identify foci of pathological processes in the oral mucosa (OM), including erosion, ulcers, compactions, and also assess the condition of the lymph nodes.
Russian specialists adhere to a similar inspection algorithm. He suggests that the dentist should pay attention to any visible abnormalities in the structure of the face, nose, cheeks or chin. Pathological changes, taking into account their localization, are recorded using special codes. Thus, ulcerations of the mucous membranes, wounds, tissue erosions, cracks, enlarged lymph nodes and any other lesions are necessarily noted.
Oral diseases
The most common symptoms of stomatitis encountered in dental practice. Acute herpetic stomatitis accounts for 85% of all diseases of the oral mucosa; chronic recurrent aphthous stomatitis is also common [1].
Aphthous stomatitis is considered a diagnostic feature of aphthous stomatitis - oval ulcerations on the oral mucosa with clear edges, with a diameter of 3-12 mm or more, surrounded by a halo of hyperemia. Herpetic stomatitis is characterized by blistering rashes not only on the surface of the mucous membrane, but also on the lips and skin around the mouth.
Data from multicenter studies in different countries of the world also indicate a high level of prevalence of other oral diseases: leukoplakia, candidiasis, lichen planus.
Leukoplakia is characterized by the presence of foci of keratosis in the form of whitish thickenings on the oral mucosa and the red border of the lips. With candidiasis, spots of white plaque with a cheesy consistency form on the mucous membrane, which are easily scraped off with a spatula. With secondary bacterial infection and erosion, the plaque may acquire a brownish tint.
The most common sign of oral lichen planus is also gray-white spots. They appear on the inner surfaces of the cheeks, tongue and gums. Due to the similarity of these manifestations with the symptoms of other diseases, in particular leukoplakia, visual diagnosis can be difficult.
Unfortunately, in recent years the number of cases of oral cancer has been increasing. The World Dental Federation attributes this to widespread smoking and alcohol consumption. Therefore, early diagnosis of cancer of the oral mucosa is becoming increasingly important. It is precisely this that makes it possible to identify precancerous and cancerous states of cells at stages when treatment can be anatomically gentle.
Experts advise paying attention to the following signs, which may be symptoms of oral cancer:
- long-term non-healing wound or irritation;
- red or white spots;
- sensation of pain, numbness, sensitive areas in the mouth or on the surface of the lips;
- tumors, thickening, roughness, erosion and other changes;
- difficulty chewing, swallowing, speaking, or moving the tongue or jaw.
The number of visits to dentists by Russians is approximately 15 million per year [2]. This figure is higher than any other medical specialty. Therefore, the doctor’s compliance with the external examination algorithm, thoroughness and accuracy during its implementation are the key to the success of early detection of many dangerous diseases of the oral cavity.
List of sources
[1] Zarkumova A.E. Structure of morbidity of the oral mucosa // Bulletin of KazNMU. 2021. No. 3. URL: https://cyberleninka.ru/article/n/struktura-zabolevaemosti-slizistoy-obolochki-polosti-rta (date of access: 05/22/2020).
[2] Astakhov P. Chief dentist of the Ministry of Health: mortality in the dentist’s chair is below 0.001% // RT, June 7, 2021. URL: https://russian.rt.com/russia/news/397438-glavnyi-stomatolog-minzdrav-smertnost (access date: 05/22/2020).
Infectious and other diseases
There are many pathogenic fungi and bacteria in the oral cavity. Their growth is inhibited by the body's immune system. As soon as its operation fails, the infection begins its attack.
In humans, a rough tongue and a white coating on the tonsils may indicate the development of follicular or catarrhal tonsillitis. The disease is accompanied by a sore throat and fever. The causative agents of the disease are streptococci and staphylococci.
The culprit of oral thrush is the fungus Candida. A very dense white coating appears on the surface of the tongue. If you try to remove it, the mucous membrane underneath will begin to bleed. The development of this chronic pathology is observed in patients with HIV infection.
Dry tongue is accompanied by disruption of the thyroid gland. Symptoms such as sweating, loss of appetite, diarrhea, irritability and anxiety are observed.
Diabetes mellitus is characterized by the development of thirst, the patient’s tongue becomes rough and dry.
If dense white plaque is concentrated on its sides and tip, this may indicate the development of hidden renal failure. This is a very serious problem that can cause death. Therefore, if you notice such formations on your tongue, you should immediately consult a doctor.
Causes of rough surface and plaque
You should be wary in the following cases:
- plaque has appeared that cannot be removed after brushing your teeth;
- the tongue has become unusually rough;
- began to crack;
- increased;
- papillae become inflamed;
- geometric patterns appeared.
A symptom such as roughness is almost always accompanied by the appearance of a rash or plaque. These are symptoms of various diseases - from gastrointestinal lesions to diabetes.
Roughness is almost always accompanied by the appearance of a rash or plaque.
A small layer of white plaque in the morning upon waking is normal. It should completely disappear by lunchtime. This is simply an accumulation of particles of dead epithelial cells, food debris and mucin protein, which is found in saliva. Bacteria are also involved in its appearance. There are a lot of them in the oral cavity. At the same time, plaque is easily removed during brushing.
Oral hygiene can be an excellent preventive measure. It is useful to clean the surface of the tongue with a special scraper or brush. To consolidate the effect, you need to use mouthwash. This removes dangerous bacteria, food residues and other substances. The surface becomes clean, smooth and healthy.
If your tongue is rough with a white coating that cannot be removed by regular cleaning, or you feel discomfort, then you should consult a doctor. It will be necessary to undergo a comprehensive examination to identify the cause.
Let's consider the main reasons for the appearance of this pathology:
- Dehydration (the tongue becomes rough and dry), intoxication (in case of intestinal infections and poisoning), liver problems.
- Cracks can warn of disruptions in the endocrine system or diabetes.
- Lack or excess of nutrients.
- Stagnation of food. In this case, the unevenness is accompanied by cyanosis or pallor. This condition requires immediate medical attention.
- Disorders of the stomach, duodenum, and gallbladder. If gastritis develops, areas of peeling appear. There is also a bitter taste in the mouth.
- An uneven surface combined with swelling can warn of problems with the spleen, kidneys or heart.
- With blood diseases, ulcers appear.
- With an “acute abdomen,” the organ becomes enlarged, turns red, and becomes covered with a gray coating.
- With HIV, hairy leukoplakia can develop. With it, small villi appear on the tongue.
- When burned, the tongue also becomes rough.
Cracks can warn of disruptions in the endocrine system or diabetes.
Let's look at some pathological conditions in more detail.
Leukoplakia
Leukoplakia affects the mucous membranes. Often this is the reason why the tongue becomes rough. This pathology can be easily confused with thrush. A white coating also appears on the tongue, but it has clearly defined edges. Its surface is rough and dry. It is impossible to remove plaque with a spatula.
The reasons for the development of this pathology have not been fully identified. It is believed that the main role is played by provoking factors: thermal, physical and chemical irritation. Particularly dangerous is the influence of several agents at once. For example, irritation by galvanic current, which is formed as a result of the use of dissimilar metal prostheses. As well as mechanical damage to the mucous membrane from dental instruments. In smokers, leukoplakia can occur as a result of exposure to smoke and high temperatures.
Internal factors play an important role in the development of the disease. These are hormonal abnormalities, gastroenterological diseases, and lack of vitamin A. The danger of the disease is that it can gradually transform into cancer.
Diagnosis and treatment
The doctor can prescribe treatment only after he determines exactly why the tongue is rough. Sometimes the cause can be identified immediately and there is no need for numerous diagnostic procedures. But in some cases it may be necessary:
- complete blood count;
- bacteriological study of oral microflora;
- gastroscopy;
- Ultrasound;
- bronchoscopy;
- acid reflux test.
Once the underlying disease is identified, the doctor will be able to prescribe treatment for the patient. The tongue will return to normal as soon as the patient’s condition begins to improve. To eliminate dry mouth and reduce pain, the doctor additionally prescribes rinses with various antiseptics.
Treatment with traditional methods
There are several effective traditional medicine recipes that help alleviate the patient’s condition. It is recommended to rinse a rough tongue with infusions of the following medicinal plants:
- sage;
- chamomile;
- calendula;
- Oak bark;
- mint;
- sea buckthorn.
To prepare the infusion, pour a teaspoon of the selected ingredient into a glass of boiling water and leave for several minutes. After the liquid has cooled, it is filtered and used for rinsing. You can add a drop of iodine, aloe juice or honey to the finished infusion.
In addition, you can put a cotton pad soaked in rosehip oil, propolis tincture or a mixture of carrot and potato juices on your tongue for a few minutes. This procedure will relieve pain, moisturize, soothe and disinfect the mucous membrane. After 3-5 minutes, the cotton pad should be removed and your mouth should be rinsed with warm water.
Leukoplakia of the oral mucosa
Typically, leukoplakia is localized on the mucous membrane of the cheeks, mainly at the corners of the mouth, on the lower lip, less often on the tongue (on the back or side surface), alveolar process, and in the area of the floor of the mouth. The clinical picture of the disease is heterogeneous, and therefore it is necessary to distinguish between flat, verrucous, erosive and Tappeiner leukoplakia. The clinical picture of leukoplakia depends not only on the form of the disease and the factor that caused it, but also on the location. The course of leukoplakia from the moment of its appearance to the onset of malignancy can be divided into several stages. The process, as a rule, begins with the preleukoplakic stage, which is characterized by slight inflammation of a limited area of the mucous membrane. After this, its uniform keratinization occurs very quickly. Subsequently, as the process progresses, the lesion begins to rise above the surrounding normal mucous membrane (verrucous leukoplakia). During this period of the disease, hyperplastic changes are replaced by metaplastic changes, and therefore malignancy often occurs in this form. The erosive form has the greatest potential for malignancy. Thus, all clinical forms of leukoplakia are a stage of a single pathological process. All forms of leukoplakia have the potential to become malignant, with the highest incidence of malignancy observed when the process is localized on the tongue. Leukoplakia in some patients can exist for years and even decades without malignancy, while in others it quickly transforms into cancer. The duration of leukoplakia before its possible transformation into cancer is very individual and primarily depends on the form of leukoplakia, since its verrucous and erosive forms have the greatest potential for malignancy. Clinical symptoms by which one can judge the beginning of malignancy of leukoplakia depend on the form of the disease. Signs indicating malignancy of flat leukoplakia are sudden erosion and the appearance of compaction at the base of the leukoplakia lesion. Particularly suspicious is the occurrence of a compaction not under the entire area of keratinization, but only under one of its sides. Clinical signs of malignancy of erosive leukoplakia: the appearance of compaction at the base of the erosion, bleeding of the erosive surface when it is injured, ulceration, the formation of papillary growths on the surface of the erosion or a rapid increase in its size. However, in the early stages of malignancy, all these signs may be absent. In connection with the above, it is advisable to remove foci of verrucous and erosive leukoplakia as early as possible, followed by histological examination.
Reviews about the treatment
Patients often leave reviews about how they managed to cure a rough tongue. In some cases, therapy does not take much time. Improvement occurs quickly after using regular rinses with medicinal herbs. Lubricating the surface of the tongue with sea buckthorn oil gives good results.
In the event that dryness, plaque and roughness of the tongue are associated with the development of serious pathologies, it is not possible to manage only with antiseptic rinses. Patients often write that they have come a long way before they were given the correct diagnosis. Only after complete recovery were they able to forget about the problem of dry and rough tongue.
On the tip of the tongue
Remember the situation when you really want to say something to your interlocutor, but you can’t find the right word: it doesn’t come to your mind, but it’s as if it’s “twirling on the tip of your tongue.” This is a common example of a cognitive distortion (more precisely, a memory distortion), which for simplicity is called “on the tip of the tongue.” Read about what it is and what cognitive mechanisms are involved in the occurrence of this phenomenon in our blog.
Share
The “tip-of-the-tongue” phenomenon (in English the very euphonious and playful ‘tip-of-the-tongue’ is used) was first described by the “father of American psychology” William James in his work “Principles of Psychology”. Strictly speaking, James did not call the phenomenon he described as is customary now, but he spoke about it quite clearly - as “a name that does not correspond to its form.” Indeed, in the case when a word is on the tip of our tongue, we can describe it (sometimes even as if with excerpts from a dictionary entry), select synonyms for it that reflect the essence, but do not express it completely, or reproduce something consonant.
An excellent example of an illustration of this distortion is the story by Anton Pavlovich Chekhov “The Horse's Name.” One of his characters, trying to remember the name of a healer who knows how to charm a toothache, relies on the fact that it is somehow connected with horses. Before remembering her (spoiler for those who haven’t read: Ovsov), he goes through all possible options like Kopytin, Uzdechkin and Merinov. If we evaluate this (and any other) example from the point of view of linguistic signs (here we can rely on Ferdinand de Saussure), then we can say that the signified does not find its exact signifier in the human consciousness, even if it looms somewhere nearby.
In general, “on the tip of the tongue” reflects the imperfection of the mechanisms of human thinking and memory. In this case - lexical access. The information that is stored in a person’s semantic memory can be represented in the form of vocabulary cards (they are also used to learn new words in a foreign language): on the one hand, what the object is, that is, the signified, and on the other, the form, in which this object can exist in our vocabulary (or as a visual image, smell, sound - in general, everything that can be somehow imagined), that is, a signifier. In the mind, both sides of such a vocabulary card are linked together and are used together in the process of speech production and processing.
For example, imagine that someone mentions a hat in a conversation with you; you may think that knowing what a “hat” is is intuitive and does not require any additional thinking processes. In fact, this is not so: in order to understand what is being said, when processing the lexical shell of an object, the corresponding card in the mind must be found and turned over, even if this happens quite quickly. The same thing happens during speech production: for example, if you want to tell your interlocutor who is talking about a hat about another headdress, for example a hat. The “tip of the tongue” phenomenon shows that this process is not as automatic as we think, and that the desired card is not found and turned over immediately.
The word, of course, is known: this is evidenced either by the fact that the word is eventually remembered, or by something similar to an epiphany (or eureka effect), when someone else reminds us of this word. The fact that the word is known is also indicated by the fact that along the way we remember a lot of other (similar, but unnecessary) information: as if we were sorting through those same vocabulary cards in search of the necessary one.
Of course, like any other phenomenon of human thinking, “on the tip of the tongue” has been studied many times. The first experimental work was carried out in 1966 by Roger Brown and David McNeil from Harvard University. In their study, volunteers had to remember a specific word that was spoken to them. Scientists noticed that when participants could not remember the required word immediately, they tried to “grope” for it in other ways - for example, they named the number of syllables in it, the first letter or another word consonant with it. This work also showed that such a situation arises not because the word is unknown to the respondent, but because he cannot recognize and reproduce it at a certain moment. Brown and McNeil's work looks at "tip of the tongue" in terms of "direct access" to the word, which overlaps as the phenomenon occurs.
The opposite approach to the study of such a distortion is heuristic-metacognitive: in simple terms, in its framework, the appearance “at the tip of the tongue” is explained not by access to just one word, but in general to all the information that is associated with it - certain clues that can potentially “get” the desired form from our consciousness. The feasibility of this approach was experimentally demonstrated in 1977 by Asher Koriat and Israel Lieblich: new words in their study were more likely to be “on the tip of the tongue” of volunteers if their definitions were longer (and therefore less memorable). Recent work on the phenomenon quite often combines these two approaches, indicating that “on the tip of the tongue” is a combination of violations of direct access to both the word itself and the information that is associated with it.
Quite often this effect is observed when trying to extract a word from memory in a non-native language. Indeed, research with bilinguals shows that words from a second, less dominant language are more often found on the tip of the tongue. It is impossible to say that the word is unknown, as we have already found out, but we can confidently say that the card with it is hidden a little further simply because it is used less often.
The frequency of occurrence of the phenomenon also depends on the age of the speaker (this is mostly due to cognitive decline - memory, including semantic memory, is no longer what it used to be). “On the tip of the tongue” sometimes even accompanies one of the types of aphasia, but in any other case it is a completely harmless phenomenon. So if you ever feel stupid because you can’t pronounce the word “synchrophasotron” or “existentialism” in time, while fully understanding what is being said, then don’t be sad: the truth is still somewhere out there .