Acute pericoronitis
Acute pericoronitis is easily diagnosed with a superficial examination and X-ray examination.
1. Catarrhal form. With this form of acute pericoronitis, patients experience:
- Pain in the area of the erupting figure eight during chewing;
- Slightly enlarged and painful submandibular lymph nodes;
- The erupting wisdom tooth is completely or partially covered with a swollen and hyperemic hood - an overhanging area of the gum;
- When pressing on the hood, pain is felt, but there is no purulent discharge.
With this form of the disease, the patient's general condition remains satisfactory, and the body temperature does not increase. If therapeutic measures are taken in time, recovery occurs very quickly.
2. Purulent form. In the purulent form of acute pericoronitis, the patient’s condition worsens significantly, and the following symptoms appear:
- Increased body temperature to 37.5°C;
- Constant severe pain in the area of the third molar, which becomes unbearable when chewing;
- Severe swelling and redness of the gums;
- Pain when swallowing;
- Pain sensations spread to the temporal region, radiating to the ear;
- You may have difficulty opening your mouth;
- Swelling of the cheek appears;
- When you press on the hood hanging over the erupting tooth, pus is released and a sharp pain appears.
Chronic pericoronitis
A chronic process develops if patients do not go to the dentist when acute pericoronitis occurs and try to fight the disease on their own, temporarily muffling its symptoms. Due to constant trauma to the hood during eating, brushing teeth, and with repeated exacerbations of pericoronitis, pus accumulates, and the pathological process spreads to the bone tissue around the tooth, spreading along the root. As a result, bone resorption occurs, which can be seen on an x-ray. Patients experience the following symptoms:
- Constant pain or discomfort in the tooth area.
- Difficulty chewing.
- Bad breath.
- The surface of the mucous membrane of the hood has ulcerations.
- Scarring may appear along the edge of the hood.
- When pressing on the hood, serous or purulent exudate is released.
- Enlarged and painful submandibular lymph nodes.
- The wisdom tooth, and sometimes the tooth adjacent to it, becomes mobile.
Causes of pericoronitis
The disease most often results from:
- epithelial injuries due to difficult long-term tooth eruption;
- impacted (formed, but not erupted outward) teeth;
- atypically located tooth roots;
- thickening of the gum mucosa;
- accumulation of soft plaque under the hood and, accordingly, infection of tissues;
- reduction in the size of the dental arch, lack of space for teething;
The catalyst for pericoronitis of wisdom teeth is often a source of infection in the oral cavity. Very often the disease is provoked by caries, stomatitis or periodontitis. Sometimes the disease occurs against the background of ignoring the rules of personal hygiene, prolonged stress, hypovitaminosis and other conditions accompanied by decreased immunity.
Diagnostics
To diagnose pericoronitis, a specialist uses several methods:
- First of all, this is a visual examination and a detailed questioning of the patient about symptoms.
- In addition, an x-ray is required, which will show the deeper layers of soft tissue, tooth and bone.
If pericoronitis occurs in the area of a growing wisdom tooth, it is important to know its position . Additionally, the x-ray gives an idea of the periodontal tissue and the condition of the bone tissues that are located in the same area.
It is important at the diagnostic stage to distinguish between chronic forms of pericoronitis and periodontitis/pulpitis. These diseases can present with extremely similar symptoms, but have different causes and radically different treatments.
Symptoms of tooth pericoronitis
The main clinical manifestations of dental pericoronitis may be the following symptoms:
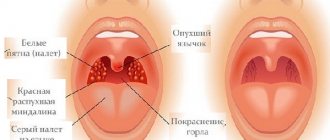
- swelling of the soft tissue of the gums in the area of the growing tooth;
- redness of soft tissues;
- pain that worsens when eating and brushing teeth;
- pain radiating to the temple, ear or eye socket (on the affected side);
- Difficulty opening the mouth and talking due to pain and swelling;
- bad breath;
- purulent discharge from under the gingival hood;
- increase in body temperature to 37.5 degrees.
If the disease has acquired a serious form, an increase in the submandibular and parotid lymph nodes (on the affected side) is observed, as well as a significant deterioration in the patient’s well-being.
Meanwhile, the most characteristic manifestations of wisdom tooth pericoronitis are:
- swelling of the gums;
- redness of the gums;
- pain in the gum area.
Often, with acute pericoronitis, the swelling is so severe that the patient has difficulty speaking and it becomes difficult to open and close his mouth.
Pericoronitis - what is it?
This is an inflammation of the soft tissues of the oral cavity, namely the gums under which the tooth is cut. According to statistics, most often patients experience pericoronitis of the wisdom tooth, because the eruption of “eights” can be associated with a whole range of problems: they are not present in the primary occlusion, but they appear at a fairly mature age (from 25 to 35 years, sometimes later), when the patient’s jaw bone is already fully formed and is very dense to its structure. The same applies to the gums. It turns out that the body is simply not ready for this process.
On a note! In dentistry, the concept of “pericoronitis” refers not only to wisdom teeth, as some ordinary people believe. In fact, pathology occurs during the eruption of any teeth, during the formation of a primary and permanent bite, and during the active change of a primary bite to a permanent one (at the age of 6-7 to 12-14 years). Therefore, not only adult patients, but also young children and adolescents may encounter it.
Types of pericoronitis
Depending on the complexity and localization of inflammation, pericoronitis is divided into:
- Spicy.
The initial stage of the disease, which is characterized by pain, hyperemia and swelling of the gums. In case of acute pericoronitis of a wisdom tooth, there is no purulent discharge and the general condition of the patient does not suffer. With proper timely treatment, this type of disease disappears in 3-5 days.
- Ulcerative.
The disease develops against the background of epithelium damaged by fusospirochetes. A characteristic symptom of ulcerative pericoronitis is the appearance of a necrotic rim along the edges of the gums. Small ulcers form on the mucous membrane. When plaque is removed from the gum surface, bleeding begins.
- Purulent
Pericoronitis, as a rule, occurs in a subacute form and is manifested by severe pain. Pus is released from the source of inflammation, and the temperature rises. In the absence of timely treatment, the disease can provoke the formation of abscesses, phlegmon and periostitis.
- Posteriormolar.
The disease develops when molars erupt incorrectly. A gingival hood forms, which then becomes infected due to the active proliferation of bacteria.
Mechanism of the disease
When a tooth, be it a molar, incisor, canine or premolar, erupts, it needs to pass through various “obstacles”: the jaw bone, the periosteum, and the gum. Almost before its appearance, the crown rests on the mucous membrane, which hangs over it in a fold and forms a kind of hood. Depending on the individual characteristics of the patient and his state of health, the tooth can remain under the gum from a month to six months. Gradually, he lifts the gum and tears it, but the mucous membrane in such a situation cannot remain reliable protection for him from the external influence of bacteria, opportunistic microflora of the oral cavity, and the smallest pieces of food. All these microparticles and microorganisms can easily penetrate under it, but it is almost impossible to clean them out. Accordingly, over time, they gradually begin to accumulate under the gingival hood, rot and lead to the appearance of an inflammatory process.
Treatment of pericoronitis
Treatment by a dentist and surgeon should be aimed not only at eliminating the symptoms of the disease, but also at eliminating its causes. As a rule, for wisdom tooth pericoronitis, drug therapy and surgical intervention are used.
Drug treatment is the fight against microorganisms that caused the development of the infectious process. The doctor also prescribes medications that reduce pain and inflammation symptoms.
As a rule, the following groups of drugs are used to treat wisdom tooth pericoronitis:
- antiseptics, mouth rinses. The products reduce the microbial load and wash away bacterial and purulent particles.
- nonsteroidal anti-inflammatory drugs, for example, Ibuprofen, Ketorolac.
- antimicrobial, broad-spectrum anti-inflammatory drugs, for example, Amoxicillin, Amoxiclav, Azithromycin.
Surgical intervention for wisdom tooth pericoronitis usually involves excision (removal) of the gum hood over the wisdom tooth. This tactic is chosen in case of frequent relapses of the disease, pronounced pain syndrome, and spread of the purulent process to surrounding tissues. When an area of soft tissue is excised above the surface of the crown, plaque stops accumulating, which prevents infection and progression of the disease.
Excision of the hood takes no more than 10-15 minutes and is performed under local anesthesia.
If removing the hood and conservative treatment does not lead to an improvement in the condition, it is possible to remove the wisdom tooth. Removal is also carried out in case of incorrect tooth position or significant deviation of the “figure eight” from its physiological axis. In rare cases, not only the wisdom tooth is removed, but also part of the bone tissue. After removal, in almost 100% of cases, the patient recovers completely.
It is worth noting that many patients often insist on maintaining the “eight”. Many believe that in the future a wisdom tooth may be useful if prosthetics are needed. However, such an opinion is wrong. The wisdom tooth is located the farthest away and does not bear a significant functional load, taking only 2% of the total load on the dentition. When installing a crown, the wisdom tooth will not withstand the pressure, and the prosthesis will have to be replaced very soon.
The main method of treating pathology is surgery
How to treat the disease? In almost all clinical cases, doctors see only one effective method - surgery, namely excision of the gingival hood. However, you should not be afraid of such a measure, because in most cases, it brings a positive result, opens access to the growing tooth and helps it finally break out and take its intended place in the row.
Important! Indications for excision of the gingival hood in case of pericoronaritis are: the integrity and healthy condition of the crown and roots of the erupting unit, as well as its correct location in the jawbone. Those. The erupting unit should not be impacted or dystopic, should not disturb the bite and interfere with adjacent teeth.
During the procedure, the specialist uses anesthesia, so you will not feel any pain. Next, the dentist will treat the affected mucosa with antiseptics and remove the soft tissue hanging over the tooth using ordinary surgical scissors or a laser. Afterwards, it will clean the resulting area from the remains of accumulated food, plaque and bacterial deposits.
Rinse
Special rinses will help relieve pain and swelling at home. However, such treatment is symptomatic. If inflammation progresses, in no case should you limit yourself to rinsing only.
The treatment for inflammation recommended by dentists is ASEPTA Active mouth rinse. This unique two-component product with a combination of “chlorhexidine + benzydamine” has an antimicrobial, anti-inflammatory effect and provides an immediate analgesic effect.
To eliminate inflammation and relieve discomfort during wisdom tooth pericoronitis, it is possible to use such medicinal herbs as:
- chamomile;
- sage;
- calendula.
Supportive therapy methods
Medicines, antibiotics and antiseptics
All these drugs are prescribed after the surgical stage and contribute to the rapid rehabilitation of the patient, allowing recovery to be achieved within 7-10 days. Here, depending on your medical history, the doctor may prescribe treating the affected mucosa with antiseptics like Chlorhexidine or Miramistin, taking antimicrobial drugs (Amoxiclav, Hemomycin, Tsiprolet, Metronidazole - the drug and course of administration are prescribed doctor), painkillers (Nurofen, Ibuprofen), the use of ointments and gels (Cholisal, Asepta, Metrogyl Denta).
On a note! Very often, the gums become inflamed due to the fact that a large amount of food has accumulated under it and has begun to rot. Therefore, try to cleanse with a regular brush - perhaps the problem can be solved without surgical intervention.
Folk remedies
Here, decoctions of chamomile and sage, as well as calendula, are very helpful in coping with postoperative consequences, removing swelling and disinfecting the wound. Soda-salt solutions and rinses are well suited for this purpose. But such methods of traditional medicine as applying pieces of lard to damaged mucous membranes, rinsing with tea leaves, and disinfecting with garlic should be abandoned.
Such methods, at best, will delay the healing period; at worst, they will lead to complications (burns, re-infection, injury to sensitive mucous membranes).
If all the doctor’s recommendations are strictly followed, tissue healing usually takes no more than 2-3 weeks.
Possible consequences
Pericoronitis of the wisdom tooth in the lower jaw is a rather dangerous disease, ignoring which can lead to very unpleasant consequences.
Possible complications of the disease may be:
- abscesses, phlegmon of the vestibule of the mouth, buccal area;
- periostitis;
- osteomyelitis of the jaw;
- periodontitis;
- ulcerative stomatitis;
- actinomycosis;
- paradental cysts.
In addition, if wisdom tooth pericoronitis affects the lymph nodes, if inflammation develops, the lymphatic system may become a victim of infection.
And, of course, without proper treatment, the disease can become chronic and periodically “harass” the patient with unpleasant symptoms. Inflammation can spread to neighboring healthy teeth. Therefore, in order to avoid complications, treatment of the disease should be carried out as early as possible.
Complications of pericoronitis
Complications of pericoronitis develop in the absence of proper treatment, when patients try to self-medicate:
- Retromolar periostitis - a purulent infection spreads to the periosteum, where an abscess forms. The patient experiences increased pain in the area of the teething tooth, general weakness appears, body temperature rises to 38.5°C, chewing food becomes almost impossible. Periostitis can cause the development of osteomyelitis and phlegmon.
- Purulent osteomyelitis is an acute purulent-necrotic inflammation of the jaw bone tissue. It develops rapidly, and after improper treatment it can turn into a chronic purulent form.
- Non-purulent osteomyelitis of the jaw bone is a chronic inflammatory process in which foci of osteosclerosis are formed in the bone tissue - changes in its structure and density. Changed areas under the influence of the inflammatory process may undergo necrosis.
- Perimaxillary phlegmon is a diffuse purulent inflammation that develops in the connective tissue; phlegmon is characterized by further spread into the cellular spaces.
- Purulent lymphadenitis - purulent inflammation develops in the submandibular lymph nodes.
If treatment for pericoronitis was started as soon as possible after its occurrence, the prognosis is favorable - cure occurs quickly and without complications.
Prevention of pericoronitis is simple - you need to regularly undergo a preventive examination of the oral cavity; an experienced doctor will notice the manifestations of not only pericoronitis, but also any dental disease at an early stage.
Prevention
As you know, it is easier to prevent a disease than to treat it. The main disease prevention measures are:
- annual dental examinations;
- timely diagnosis and treatment of impacted molars;
- maintaining oral hygiene;
- timely treatment of caries, gingivitis, periodontitis and other dental diseases;
- Regular (once every six months) professional teeth cleaning in a dental clinic.
Remember: pericoronitis without proper treatment can cause very serious complications. Therefore, if you suspect inflammation, do not delay your visit to the dentist. The doctor will help you cope with unpleasant sensations in a matter of days and prevent the development of the disease.
Surgery with laser
The procedure performed using a laser is more preferable, because will help achieve the following advantages:
- avoid further complications,
- prevent tissue infection,
- quickly cope with the rehabilitation period,
- restore the condition of the mucous membrane due to accelerated tissue regeneration,
- reduce pain after surgery,
- will eliminate the need to additionally treat the affected area with iodoform turundas and stop bleeding (laser beams will have a cauterizing and anti-inflammatory effect).
The only thing you need to remember when preparing for such a procedure is contraindications. Laser treatment is not suitable for people with cancer problems.
Clinical researches
Repeated clinical studies have proven that the two-component mouth rinse ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component rinses - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The role of hygiene products in the treatment of periodontal diseases (S.B. Ulitovsky Honored Doctor of the Russian Federation, Honored Dentist StAR Prof., Doctor of Medical Sciences, Department of Preventive Dentistry of Pavlov Pavlov State Medical University, St. Petersburg) S.B. Ulitovsky - Honored Doctor of the Russian Federation, Honored Dentist of StAR, Prof., Doctor of Medical Sciences; E.S. Alekseeva - associate professor, candidate of medical sciences; A.A. Vasyanina - associate professor, candidate of medical sciences; V.A. Grigoriev - Associate Professor, Ph.D.
- The use of drugs from the Asepta line in the complex treatment of inflammatory periodontal diseases (N.V. Berezina E.N. Silantyeva S.M. Krivonos, Kazan State Medical Academy. Kazan.) N.V. BEREZINA, E.N. SILANTIEVA, S.M. KRIVONOS Kazan State Medical Academy
When does the gingival hood need to be removed along with the tooth?
Medical intervention is not always limited to just excision of the gingival hood. Sometimes even removing the inflamed mucosa will not help solve the patient’s problem - then doctors resort to removing the tooth itself.
Why such drastic measures may be necessary:
- excision of the hood was carried out, but tissue inflammation does not stop and even continues to progress,
- there is not enough space in the row for the tooth that is about to erupt,
- the tooth is impacted or dystopic: this most often happens with eights, then their preservation can threaten the normal functionality of neighboring units and significantly undermine their health,
- a gingival hood grows again above the tooth: this type of anomaly occurs in 3-7% of all clinical cases,
- the tooth under the excised gum is affected by deep caries or pulpitis and is destroyed, and its treatment is impractical.
In all of these cases, a removal procedure is carried out. First, the doctor administers an anesthetic, then carefully dissects the gum, extracts the tooth with special forceps, treats and sutures the resulting wound.
Pericoronitis during pregnancy
During the period of bearing a child, women begin to undergo hormonal changes in the body, this is a risk factor for the occurrence of the disease. Symptomatic manifestations and diagnostic procedures do not have any features or differences from other categories of the population.
Since surgical interventions during pregnancy can cause great stress to a woman, some doctors recommend removal of wisdom teeth at the planning stage. Although, dental interventions are not contraindicated for pregnant women.
Excision of the hood, tooth extraction, laser therapy can be carried out after 16 weeks after conception; before and after 33 weeks, only conservative treatment can be used. It includes rinsing the mouth or taking tablets from the group of painkillers, anti-inflammatory, and decongestants. However, their prescribing should be done exclusively by the attending physician, as all medications should not have a negative effect on the development of the unborn baby.
Tooth extraction for pericoronitis
One of the treatment options for pericoronitis is the removal of the problematic wisdom tooth. This decision is made only after x-ray diagnostics.
Removing the figure eight is indicated in the following cases:
- the crown cannot fully erupt due to the jaw being too narrow;
- the tooth is located horizontally or grows into the cheek;
- the third molar puts pressure on neighboring teeth, deforming the entire dentition;
- secondary development of pericoronitis.
Tooth extraction is carried out immediately after cutting the gums. The tooth is removed using surgical forceps, after which the wound is sutured.
How to relieve pain when wisdom teeth erupt?
At the first symptoms of pericoronitis, it is recommended:
- rinse the mouth with a solution of soda, salt or furatsilin;
- wipe the gums with a decoction of chamomile, St. John's wort or calendula (room temperature);
- lubricate the site of inflammation with iodine or Metrogyl Denta ointment;
- take a painkiller tablet (Analgin, Solpadein, Ketanov, etc.).
However, consult a dental surgeon as soon as possible. Treatment of pericoronitis should be started immediately, otherwise the risk of developing phlegmon (diffuse purulent inflammation) increases. A list of competent specialists is on our website.
Pain during pericoronitis
A person feels like the gums in the back of the mouth are very sore. At first, there will be a slight itching on the gums. After some time, the gums begin to swell.
As the infection spreads, you may begin to experience pain in your mouth. It will become impossible to open your mouth normally without pain.
When a wisdom tooth in the upper part of the jaw comes into contact with a wisdom tooth in the lower part of the jaw, pain will also occur.
What can you do about pericoronitis?
How is pericoronitis removed? There are several things that can be done.
Mouthwash. The easiest (and cheapest) is to rinse around the affected gum with hot salt water. The heat opens the blood capillaries and helps your own immune system fight off the infection.
Physical effect - the solution vigorously flushes out the accumulation of bacteria from under the gums. And bacteria don't like salt. But you should do this every hour every day for 2-3 days.
A more effective solution is mouthwash, which releases oxygen; oxygen is harmful to bacteria. This works better than rinsing with hot salt water. An electric toothbrush also helps.
Douching the cavity. If you have a small plastic syringe, you can use a stream of hot salt water or oxygen to release the mouthwash directly under the gum.