Why are Bednar's aftas called exactly that - after the surname of their first researcher? Are they something special?
Yes, they, which are quite common in dentistry, differ sharply from other symptoms and disorders. And the differences from other types of ulcers of the oral mucosa are absolute.
Firstly, this is a disease exclusively of childhood, and secondly, the localization and appearance of ulcers are typical signs specifically for Bednar's aphthae. Finally, the disease has features and course that are characteristic of them.
And it all starts with the thumb. More precisely, from his sucking. It has long been noted that Bednar's aphthae are more common in children who suck their thumbs. The favorite object of the process is the thumb.
Bednar's aphthae occur precisely in the area where this finger rests, supported from below by the tongue. This is the zone of the palate, or more precisely, the border between the hard palate and the soft palate.
The mucous membrane in this zone is not particularly thick, and if it is compressed for a long time between the palatine bones, on the one hand, and a foreign object of sufficient hardness in the mouth, on the other, it is damaged. And immediately to its entire depth (thickness).
The mechanism of injury in the formation of Bednar ulcers is comparable to that in the formation of pressure ulcers. Therefore, as with it, the depth of tissue necrosis is significant.
Thus, the “sweet finger”, with which the child does not want to interrupt communication day or night, becomes the cause of a serious illness.
Why does the disease occur?
People first started talking about this pathology 150 years ago; during this period, erosive changes in the oral mucosa, localized at the border of the soft and hard palate, were considered a disease of the poor. At that time, the causes of this disease in children were considered to be malnutrition, environmental problems, and poor oral hygiene. Over time, Bednar's aphthae began to be viewed as a consequence of traumatic injury to the oral mucosa with subsequent infection.
There are not many reasons for the appearance of aphthae in infants:
- traumatic factor during breastfeeding (in particular, the mother’s hardened nipple);
- consequence of trauma during childbirth;
- inappropriate size of pacifiers;
- frequent use of non-orthodontic pacifiers.
In older children, aphthae in the oral cavity occurs:
- in case of violation of basic rules of personal hygiene;
- against the background of an unbalanced diet, poor nutrition;
- Often the causes of the disease are hormonal imbalance and vitamin deficiency;
- some children suffer from the bad habit of biting their nails or putting foreign objects into their mouths, causing infection with them;
- in case of immune failure.
Using dirty pacifiers, toys, and the habit of putting your fingers in your mouth are common causes of ulcers on the oral mucosa.
Important! Some doctors associate the appearance of Bednar's aphthae in the mouth with congenital heart disease.
Development mechanism
How to treat aphthous stomatitis in children
Children's oral mucosa is extremely sensitive to any aggressive influence of external aggressive factors. Any mechanical irritation can become a trigger that will lead to the appearance of ulcers. Thus, the affected cells are slowly restored, as a result of which numerous erosions (aphthae) form on the mucous membrane.
It is noteworthy that with a prolonged course (no treatment), a secondary infection can join the ulcers. In this case, the bottom of the aphthae becomes covered with white fibrin, and then with a thick yellow coating. The area of the ulcerative lesion naturally increases, and the regeneration process slows down even more.
Symptoms and diagnosis
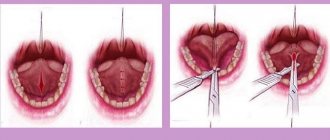
The classic manifestation of the disease (shown in the photo above) is ulcerative formations on the oral mucosa, which are “attached” to the border of the soft and hard palate. The aphthae have a characteristic oval shape and are located symmetrically in relation to each other. The affected areas are covered with a dense yellow coating.
If a child’s immune system is weakened, such formations can significantly increase in size, acquire an irregular shape, and occupy almost the entire palate. In this case, the growth of aphthae is accompanied by the appearance of a pronounced pain syndrome - the child becomes whiny, restless, and the treatment process is complicated.
Timely seeking help from a dentist will not only detect the disease, but also prevent it from becoming chronic.
The appropriate diagnosis is made by a pediatrician based on an analysis of the clinical picture of the disease; if necessary, a smear is taken from the mucous membrane (to determine the type of bacterial infection).
Important! Without fail, a specialist differentiates the disease from aphthous stomatitis, a common childhood disease in which erosions are located in the vestibule of the oral cavity.
Clinical picture
The size of AFT is from a pinhead to 5 mm in diameter, round or oval in shape. The number of aphthae depends on the form of the disease; Thus, with herpetic stomatitis (see) on the oral mucosa, with a mild course, 1-5 aphthae are observed, with moderate severity - up to 20, with severe - can reach 100. The surface of the aphthae is covered with a yellow-white coating; The duration of their development in acute stomatitis is from 5 to 10 days, in chronic stomatitis - up to 30 days. Aphthae heal without leaving scars on the mucous membrane.
When the body's defenses are weakened, aphthae can merge, forming extensive erosive surfaces.
Herpangina, or herpangina
,—a disease caused by Coxsackie viruses (see Sore throat); pink spots the size of a pinhead appear on the soft palate and arches, successively turning into papules, vesicles and rounded erosions on a hyperemic base (tsvetn. Fig. 2).
With Pospischilla aphtoid
APHTA is localized not only on the mucous membrane of the mouth, but also on the mucous membrane of the genital organs, on the skin of the face and hands.
Currently, the disease is rare; apparently represents one of the most severe forms of herpetic stomatitis.
For Behçet's syndrome
aphthae appear simultaneously on the mucous membranes of the mouth, genitals and eyes (see Behçet's disease).
Touraine's major aphthosis
the manifestations on the oral mucosa are similar to the diseases described above; however, aphthae rash occurs against the background of a very severe general condition (multiple thrombosis of the vessels of the retina, brain and its membranes, intestines) with high mortality.
Aphthae on the mucous membrane of the mouth and nose with foot and mouth disease
- see foot and mouth disease.
How to deal with the disease
The main problem in treating Bednar's aphthae is that long-term medication is required for visible improvement. In general, treatment of the disease takes place in several successive stages:
- affected areas of the mucous membrane are treated with solutions of Trypsin and Lysozyme;
- compresses are recommended for infants, and rinsing the mouth with decoctions of medicinal plants (St. John's wort, chamomile, sage) for older children.
- The resulting ulcers are lubricated with sea buckthorn oil and Solcoseryl.
- If there is pain, patients are prescribed systemic painkillers (Kamistad).
The described actions are repeated for several days in a row, after which the child is re-examined by a specialist. It is noteworthy that the duration of the course of treatment can range from several days to 2 weeks - it all depends on the characteristics of the baby’s immune system, the reaction of his body to certain drugs, and the degree of damage to the mucous membrane by aphthae.
Obviously, eliminating the traumatic factor is of no small importance. If the child continues to use dirty pacifiers, toys, or put foreign objects in his mouth, no drug treatment will lead to the expected result.
To avoid the addition of a bacterial infection, erosive lesions of the mucous membrane are treated with local antiseptics so that the cells regenerate faster - they are lubricated with keratoplastic compounds
Aphthous stomatitis: treatment, drugs
Aphthous stomatitis in adults is the same as canker sores in children - the treatment is the same, and the treatment strategy described below is suitable for patients of any age. As for the medications listed later in the article, some of them do have age restrictions, which we will also indicate.
Due to the fact that it is usually impossible to clearly identify the specific cause of aphthous stomatitis in a particular patient, treatment will be multifocal, i.e. drugs of several groups are used simultaneously. The choice of treatment strategy and medications will depend on the following 3 factors:
1) on the severity of symptoms, 2) on the frequency of relapses, 3) on identified predisposing factors.
Treatment at the first stage should be aimed at reducing pain and inflammation in the area of ulcers, and at the second and third stages - at speedy epithelization of ulcers and preventing their occurrence in the future. To facilitate the choice of the best treatment option, all patients can be divided into 3 types (according to the criteria - severity of the disease and frequency of relapses).
- Type A - in patients of this type, aphthous stomatitis occurs no more than several times during the year and is characterized by slight pain.
First of all, in such patients it is necessary to identify local predisposing factors and eliminate them (for example, overhanging edges of fillings or hygiene products with sodium lauryl sulfate). It is important to ask the patient about eating habits to evaluate a possible relationship between stomatitis outbreaks and certain foods. The patient is advised to avoid solid foods (eg, crackers, toast), all types of nuts, chocolate, eggs, acidic drinks or foods - fruit or citrus juices, tomatoes, pineapples, salty foods. You should avoid eating spicy foods, any spices, including pepper and curry, as well as alcoholic and carbonated drinks. In type A patients, local symptomatic therapy is mainly used, which includes antiseptic rinses and gel applications for pain and inflammation.
- Type B - in such patients, aphthous stomatitis develops almost monthly, and the ulcers are so painful that they force the patient to change habits (for example, brushing teeth less often due to severe pain). It remains important to identify local and general predisposing factors and, if possible, eliminate them. It is very important to teach patients of this type to feel the first signs of the imminent appearance of ulcers - burning, itching or swelling of the mucous membrane, in order to provide early local treatment even before the formation of the ulcers themselves.
- Type C - in patients of this type, ulcers are very painful, appear so often that while one lesion is healing, the next one appears almost immediately. This group also includes patients in whom local treatment in the oral cavity is completely ineffective, and improvement in their condition occurs only after the use of systemic therapy.
Possible complications and prognosis
If you seek medical help in a timely manner, drug control against Bednar's aphthae in most cases leads to a complete cure. In another situation, this pathology can develop into a chronic recurrent form; ulcers on the palate will bother the baby several times a year with the slightest traumatic injury to the oral mucosa. In addition, ulcers are the “entry gate” for any infections. Accordingly, if they are not treated in time, the child may become a “victim” of sore throat, diphtheria and many other infectious diseases.
Prevention
To prevent the appearance of Bednar's afte on the oral mucosa, it is necessary to strictly observe the rules of personal hygiene of the child, monitor the cleanliness of pacifiers and toys. Young mothers should carefully monitor the condition of the skin of the nipple (during breastfeeding) - it can become rough as a result of certain physiotherapeutic procedures and become a traumatic factor that will contribute to the formation of ulcers on the baby’s mucous membrane.
Older children should once and for all get rid of the bad habit of biting their nails and putting foreign objects into their mouths. To strengthen the immune system, you should take vitamin and mineral complexes every six months (as recommended by your doctor).
Aphthae of newborns
Aphthae of newborns (synonym: Bednar's aphthae, ulcera decubitalia palati
) - decubital ulcers, resembling aphthae in appearance, occur as a result of mechanical damage to the mucous membrane of the palate when carelessly wiping the mouth of a newborn or as a result of disruption of the integrity of the epithelium by the nipple during artificial feeding (the epithelium of the mucous membrane of the newborn’s mouth does not keratinize and is easily injured).
In newborns and infants, small, round ulcerations appear on the mucous membrane of the palate in the area of the transition of the hard palate to the soft palate, more or less symmetrically from the midline, located accordingly to the hamulus pterygoideus (printing Fig. 1).
The same ulcers, but somewhat larger in size, usually oblong in shape, in some cases also appear along the midline of the palate.
Bednar's ulcers can become the entry point for septic infection.
In advanced cases, individual ulcers merge and form a rather extensive wound surface in the form of a butterfly with a deep crater-shaped depression in the center. The surface of such an ulcer is relatively often covered with a fibrinous coating, and then the disease resembles diphtheria of the pharynx.
To clarify the diagnosis, a laboratory smear test is necessary.
Forecast
For shallow injuries, the ulcers disappear without a trace after eliminating the traumatic factor; deep lesions heal with the formation of a scar.
Treatment
Elimination of the traumatic factor. Locally - in case of deep damage, the surface of the ulcer is cleaned with enzyme solutions (trypsin, chymotrypsin, chymopsin, etc.) and covered with keratoplastics (sea buckthorn oil, rose hips, vitamin A oil solution, carotolin, etc.).
Prevention
Extremely careful and only if necessary, cleansing the newborn’s mouth from trapped amniotic fluid and discharge from the mother’s birth canal; in the future - explaining to the mother that wiping the child’s mouth is unnecessary. When artificial feeding, you should ensure that the nipple is short and its surface is smooth.
Bibliography:
Human viral diseases, ed. A. F. Bilibina, p. 302, M., 1967; Laboratory diagnosis of viral and rickettsial diseases, ed. E. Lennet and N. Schmidt, trans. from English, p. 622, M., 1974; Pashkov B.M. Lesions of the oral mucosa in skin and venereal diseases, M., 1963, bibliogr.; Rudnev G. P. Anthropozoonoses, p. 206, M., 1970, bibliogr.; Rybakov A.I. Stomatitis, M., 1964, bibliogr.; Behcet H. Über rezidivierende aphthöse durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien, Derm. Wschr., Bd 105, S. 1152, 1937; Touraine A. L'aphtose, Bull. Soc. frang. Derm. Syph., t. 48, p. 61, 1941; S with hue rm a η n H. Krankheiten der Mundschleimhaut und der Lippen, München - B., 1958.
A. newborns
— Gavrilov K.P. Peculiarities of development and pathology of children of the newborn period, p. 90, M., 1951; Tur A.F. Physiology and pathology of newborn children, p. 255, L., 1967; Shagan B.F. Fundamentals of the doctrine of a newborn child, p. 374, Frunze, 1966.
T. F. Vinogradova; A.F. Tour (ped.).