What is periodontal tooth
The periodontium is a connective ligament that secures the tooth in the jaw bone. It is also common to call periodontium the tissue that fills the space between the alveolar process and the cementum of the tooth root.
Functions of periodontium
The main function of periodontal tissue is to anchor the tooth in the jaw bone. Physiological tooth mobility increases due to age-related and pathological changes. The width of the periodontium at the neck of the tooth should be 0.3–4.8 mm, at the apex – 0.25 mm, and in the middle of the root – 0.2 mm. Typically, the width of the periodontal space in incisors is greater than in chewing molars. With increased load on the tooth, the width of the periodontium increases, thereby causing slight loosening of the tooth roots.
Due to the fact that there are many nerve fibers in the periodontal fissure, when there is increased pressure on the tooth, a person feels an external influence. Thanks to this reflex, early physiological tooth mobility is almost impossible. Based on this, we can say that the fabric is also responsible for the shock-absorbing task.
Other functions of the periodontium include:
- plastic – participation in tooth growth;
- trophic – providing nutrition to the pulp;
- barrier – protecting the root from infection.
Anatomy
The histological structure of the periodontium includes the periosteum, alveolar tissue, periodontal ligament, gum and gingival sulcus.
- The periosteum is a dense tissue that is attached to the outer surface of the alveolar process.
- The alveolar process is a spongy bone penetrated by blood vessels and bone marrow.
- The periodontal ligament secures the teeth in the alveoli.
- The gums and gingival sulcus prevent pathogenic bacteria from penetrating into the periodontal gap.
A healthy periodontium is about 0.2 millimeters thick. It consists of elastic collagen fibers, between which are loose connective tissues.
The periodontium is literally permeated with blood vessels, which form the internal, middle and external plexuses and play the role of a kind of shock-absorbing pillow.
- The blood supply is successfully carried out by several longitudinal blood vessels.
- The lymphatic system is located along the small vessels.
- Innervation is carried out by two types of nerve endings - bushy and glomerular nerve endings of pulpal nerve fibers.
The structure of the periodontium
The structure of the periodontium includes collagen fibers, the beginning of which comes from the root cement, and the end from the alveolar process. Based on the location, the periodontium of a tooth can have a horizontal direction (at the apex of the interdental space) and an oblique course (at the apex of the tooth). Between the bundles of fibrous structures there are blood and lymphatic vessels. They deliver nutrients to the tooth tissue and gums.
Periodontal histology
The cellular composition of the periodontium includes:
- fibroblasts;
- macrophages;
- plasma cells;
- osteoblasts;
- osteoclasts.
Tissue histology shows that most of the periodontium is occupied by fibroblasts. It is these cells that make up the fibers of the ligament. During inflammatory processes, they participate in the regeneration of fibrous structures. In addition, histological examination of the tissue may reveal Malasse cells forming the epithelial lining of the cyst.
Periodontal fibers
The tissue fibers are composed of type 1 collagen protein. Collagen produced in fibroblasts is converted to tropocollagen. The resulting substance gives rise to fibrils, threads and bundles of periodontal tissue. Therefore, periodontal tissues have a fibrous structure. This structure gives the fibers flexible and elastic properties.
Anatomical and physiological features of periodontium
The anatomy of the periodontal ligament of the tooth indicates that the thickness of the tissue should not exceed 0.25 mm. However, this figure may change with increasing age and the presence of inflammatory and non-inflammatory gum diseases. Near the tooth germs, the thickness of the periodontium is much less - 0.1 - 0.15 mm, since the strength of the tissue is small compared to erupting teeth. Changes from the norm can be considered pathology.
The ligament itself consists of connective tissue and intercellular substance. It is in this substance that fibrous and collagen fibers are located. There are few elastic fibers in the connective tissue layers of the periodontal ligament, which allows this part of the tissue to resemble tendons. Elastic fibers are found most in the front teeth, and less in molars and premolars.
Innervation
The periodontium of the tooth is innervated by the facial arteries and the trigeminal nerve. The branches of the dental artery supply blood to the apexes of the root, and nutrition of the remaining parts of the tissue is provided by the interalveolar and gingival vessels. At the base of the periosteum, nerves, blood and lymphatic vessels enter the plexus. Through it, reflex impulses and biologically active substances pass into the pulp space.
The innervation of the periodontium may be impaired due to trigeminal neuralgia and serious facial injuries. In this case, emergency dental care is required.
PERIODONTIUM
Periodontium
(Greek peri around, about + odus, odontos tooth; syn.:
periodontal ligament, pericement
) - a connective tissue ligament that holds the root of the tooth in the dental alveolus of the jaw.
The periodontium develops simultaneously with the root of the tooth shortly before its eruption, i.e. in the postembryonic period. The development of the periodontium occurs due to the mesenchymal cells of the outer layer of the dental sac surrounding the tooth germ (see Teeth). The formed periodontium consists of bundles of collagen fibers stretched between the cementum of the tooth root and the bone walls of the dental alveoli. Bundles of P.'s collagen fibers have different arrangements. At the edges of the dental alveoli they have a mainly horizontal direction. Some of these fibers are woven into the gum, while others go around the neck of the tooth and form the so-called. circular ligament. This group also includes interdental fibers, which pass over the top of the interalveolar septum and connect adjacent teeth. In the lateral sections of the periodontal fissure, bundles of collagen fibers have a mainly oblique direction, and in the area of the apex of the tooth root they are located radially. In the spaces between the bundles of collagen fibers there are layers of loose connective tissue with individual elastic fibers, in which vessels and nerves pass. Among the bundles of P.'s collagen fibers, the so-called. oxytalan fibers, which in chemical composition occupy an intermediate position between collagen and elastic fibers.
The cervical part of the periodontal fissure is an area of accumulation of cells (fibroblasts, plasma and mast cells, osteoblasts, osteoclasts). Throughout the rest of the periodontal fissure, cells are grouped closer to the bone of the dental alveolus and to the cementum of the root. There are also small islands of epithelial cells (the so-called islands of Malasse), which are believed to represent the remains of the epithelial dental organ formed during the development of the tooth, and can serve as a source of development of the epithelial lining of dental granulomas and perihilar cysts (cystogranulomas).
Histochemical examination of the periodontium reveals a large amount of acidic glycosaminoglycans and high activity of redox enzymes in cellular elements.
Periodontal blood vessels form a rather dense network. They anastomose with the vessels of the gums and bone marrow spaces. Larger vessels are located in the recesses of the wall of the dental alveoli. In P., vascular glomeruli, as well as arteriovenous anastomoses, are described.
The periodontium contains many free bush-like nerve endings, which, apparently, are mechanoreceptors and record the degree of tension in the bundles of collagen fibers during the act of chewing. With age, P.'s fibers undergo partial destruction, especially in the cervical part, and the number of young cellular elements decreases.
Periodontium has a high regenerative ability. This allows, in case of P. injuries or complete dislocation of the tooth and rupture of the P. fibers, to implant the tooth into the dental alveolus (see Replantation). Among the pathological processes of P. there are inflammatory ones, including with the formation of dental granulomas near the roots of the brush (see Periodontitis), as well as periodontal disease (see).
Bibliography:
Gavrilov E.I. Biology of periodontal and dental pulp, M., 1969; Gemonov V.V. and Kozlovitser T.V. Fibrous structures of the periodontium, Dentistry, v. 53, no. 2, p. 9, 1974; Gemonov V.V., Giller L.I. and Kozlovitser T.V. On the issue of oxytalan fibers of the periodontium, in the book: Changes in periodontal tissues before and after prosthetics, ed. Sh. V. Bokanova and A. I. Voloshina, p. 57, M., 1972; Falin L. I. Histology and embryology of the oral cavity and teeth, M., 1963; Schumacher G.-H. u. Schmidt H. Anatomie und Biochemie der Zahne, B., 1972; Structural and chemical organization of teeth, ed. by AEW Miles, y. 1, NY - L., 1967.
BB Gemonov.
Periodontal diseases
The main disease occurring in periodontal tissue is called periodontitis. The disease is inflammatory in nature and is divided into:
- acute periodontitis: serous, purulent;
- chronic periodontitis: granulating, granulomatous and fibrous;
- aggravated periodontitis in chronic form.
With all types of disease, a cyst forms in the periosteum. Despite the fact that granulating and granulomatous periodontitis are included in the same group, they have differences in the manifestation of the disease. In the first case, the resulting cyst has a polygonal shape, and in the second – round. The sizes of the tumors also differ from each other.
Purulent periodontitis
The causes of periodontitis are different:
- gum injury;
- allergic reaction to drugs used in dental treatment;
- errors in tooth preparation and filling;
- errors in dental prosthetics.
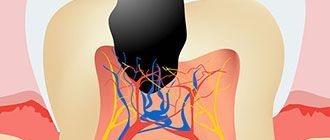
The main cause of periodontal inflammation is infection. Bacteria penetrate into periodontal tissue through caries and its complications, as well as through inflamed areas of the gums.
Periodontal infections
With untreated caries, pathogenic microflora enters the tooth pulp. If the infection affects the pulp space so severely that it can no longer serve as a barrier to pathogens entering, then the inflammatory process penetrates deep into the ligament in a very short time. For this reason, the apex becomes inflamed, the dental nerve dies and decomposes, and a cyst with purulent contents begins to form in the bone.
The causative agents of periodontitis can be: staphylococci, streptococci, lactobacilli, actinomycetes and pneumococci.
Functions
- supporting and holding. Perception and redistribution of pressure during chewing.
- reflexogenic. Regulation of chewing loads due to the fact that the periodontium contains many nerve endings.
- plastic. Promotes the restoration of ligaments and the formation of alveolar walls. Performed by osteoblasts, cementoblasts and fibroblasts.
- trophic. It is carried out with the help of nerves and capillaries and is associated with chewing pressure.
- barrier It is performed with the help of histiocytes, which do not allow pathogenic bacteria to penetrate into the tooth root area.
- sensory.
Additionally, we note that without periodontium, teething in infants is impossible; it regulates the adaptation of the tooth to the stresses that arise during chewing and biting food, performs a reparative function in the event of a tooth root fracture, and also provides root protection with the help of leukocytes and macrophages.