In accordance with the generally accepted classification, purulent pulpitis is a type of acute form of the disease, which is accompanied by inflammatory processes with purulent formation inside the pulp or on its surface.
Due to the fact that the amount of serous substance that is released into the tooth tissue during inflammation increases, purulent pulpitis of the tooth
characterized by oxygen starvation of the pulp. This negatively affects the metabolic processes that occur in its connective tissues and ultimately causes a deterioration in the protective reaction of cells. This is how an abscess occurs in the affected area, which led to another name for this disease: “pulp abscess.”
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 700
- The cost of an orthodontist consultation is 2,000
Make an appointment
Why does purulent pulpitis occur?
Precursor of purulent pulpitis in children
and adults is acute pulpitis. The formation of pus occurs from the serous exudate that is present in the nerve. Due to an increase in its volume, metabolic processes occurring in the nerve suffer, which stimulates the accumulation of lactic acid and, as a result of this process, a decrease in the protective function of cells. It is accompanied by tissue breakdown and abscess. The infection that provokes the development of purulent pulpitis penetrates the pulp in different ways:
- from a carious cavity in the absence of treatment;
- during the treatment of periodontitis with dissection of the gums;
- through blood and lymph in infectious diseases.
Treatment of periodontitis, gum incision and antibiotics
Among the measures aimed at diagnosing periodontitis with its subsequent treatment, there may be the following procedures:
- dental x-ray;
- administration of local anesthesia;
- removal of destroyed tissue, stone overhangs, inflamed pulp (cystectomy);
- coronoradicular separation, that is, dissection of the tooth;
- unsealing, straightening channels (giving them a conical shape), measuring their depth with subsequent mechanical processing;
- antiseptication of the canals using cotton swabs and chlorine or other antiseptics (the dentist can also leave the disinfectant in the canals for a while, covering it on top with a temporary filling or hermetic bandage);
- installation of a permanent filling.
Treatment of different stages of the disease can be done therapeutically or surgically. In some cases, the patient is also asked to undergo physical therapy, which consists of the use of magnetic therapy, UHF, electrophoresis, laser therapy, and paraffin baths.
If the nature of the development of the disease is such that the natural canal of the tooth is not enough to drain the resulting pus and other fluids, surgical intervention is prescribed - an incision in the gums (gingivotomy) to perform resection of the apex of the tooth root. Gingivotomy is used if the gum pocket is too narrow for further treatment or the patient has developed a periodontal abscess.
If the dentist considers it advisable to take measures to stop the destructive processes occurring in the cavity formed near the roots of the tooth, antibiotics are prescribed. Among the drugs used after pulp removal and root canal filling, a course of antibiotics is prescribed, such as Augmentin, Ciprofloxocin, instead of the classic Lincomycin for dental practice, which has too narrow a spectrum of action.
Forms of purulent pulpitis
Acute purulent pulpitis
there are two types:
- Focal purulent-serous - characterized by damage to part of the dental nerve and the release of exudate in the form of a clear liquid;
- Diffuse - characterized by damage to the entire pulp and its death. The exudate that is released has a yellowish-greenish tint and smells of rot.
It is worth noting that under favorable conditions, focal purulent pulpitis can become diffuse within 24 hours.
Prevention
For prevention, follow the recommendations:
- One of the main tips is to visit the dentist frequently. Inspection should be at least once every 6 months. This eliminates the appearance and development of caries or other pathologies. A doctor can provide treatment and prevent the condition from getting worse.
- Teach children to brush their teeth at least 2 times a day. It is better to do this after each contact with food. If this is not possible, then at least rinse your mouth.
- Dental floss removes food debris from the space between teeth. In this case, the characteristic mass from accumulated particles, which is not cleaned out, can be visually observed upon close examination. If you allow it to have a long-term effect on tooth enamel, then gradually caries and possibly pulpitis will appear in the interdental space.
- If you do not use floss, you can replace it with rinsing with antiseptic liquids.
- If you experience a negative sensation of greater or lesser intensity from cold or hot, then contact the dentist.
- Monitor the health of your child's teeth. It is necessary to treat baby teeth. Ignoring the problem leads to the appearance of an infection that affects the root units in the future.
Symptoms of purulent pulpitis
One of the symptoms of acute purulent pulpitis
are severe pain. They are caused by the fact that the pulp tissue is closed from the carious cavity by a septum, so the serous substance accumulates inside the tooth and at some point begins to put pressure on the nerve. The patient constantly experiences boring pain, which intensifies at night. In addition, there is pressure in the tooth. It is worth noting that in an advanced form, when the partition between the pulp and the carious cavity has broken through and the serous fluid begins to flow out, the nature of the pain symptoms changes. They will depend on the influence of external factors. The attacks will become long, and the “light” intervals between them will be short.
Throbbing pain spreads along the branches of the ternary nerve, covering the entire jaw. In order to prescribe treatment for purulent pulpitis
, it is important to correctly identify the diseased tooth, and this is sometimes difficult for this very reason. The pain may increase when exposed to hot substances and subside for a while when exposed to cold ones. However, with prolonged exposure to cold substances they can still intensify.
During a dental examination, the doctor notes swelling of the oral mucosa around the affected tooth. Sometimes there may be darkening of the tooth enamel and bleeding gums. Painful symptoms often spread to the entire oral cavity, ears and even the head and are accompanied by a feeling of weakness and malaise, and a slight increase in body temperature.
Causes of gingivitis and periodontitis in cats
Gingivitis in cats may begin with or without tartar or plaque present on the teeth. Dental plaque consists of a variety of bacteria and organic substances attached to an inorganic matrix composed of hydroxyapatite, calcium and phosphorus (from saliva), forming a mineralized plaque [8, 9]. Some bacteria located in the gingival crevice produce toxins (hyaluronidase and lysosomal enzymes), which, combined with a large influx of inflammatory cells, irritate the gums and cause an inflammatory response that causes swelling and redness of the gums, as well as the development of loose tissue [10, 11]. Plasmocytes and lymphocytes are the more common cells present in this type of gingival inflammation (pathogenesis of periodontitis, gingivitis and stomatitis in cats). Plasmocytes produce antibodies against bacterial endotoxins, and this antigen/antibody complex activates the complement system. These substances attract a large number of inflammatory cells through chemotactic factors and increase local vascular permeability, causing smooth muscle contraction and intense gingival retraction [12, 13, 14, 15].
- Diet—resulting in increased plaque formation—is often attributed to commercial foods (starch and vitamin D content).
- Oral conformation is common in Persian cats with brachycephalic syndrome.
- Poor oral hygiene – brushing your teeth daily reduces the build-up and adhesion of bacteria to dental cement.
- Genetics - juvenile gingivitis of Abyssinian, Persian and Maine Coon breeds
- Bacteria - Gingivitis begins with the deposition of microorganisms in the gum area, which predisposes to the formation of tartar, which is characteristic of this disease.
Common bacteria include:
- Porphyromonas circumdentaria [16],
- Capnocytophaga canimorsus, Pasteurella spp [17],
- Fusobacterium nucleatum [18]
- Less common infections include Bacteroides spp., Actinobacillus spp., Staphylococcus spp., Streptococcus spp., Pseudomonas spp. Tannerella forsythia [19], Aggregatibacter spp. [20], Prevotella spp. [21].
- It is clear that Bartonella spp. is not associated with this disease [22].
- Viruses—all infectious agents, including feline calicivirus (FCV)—are most often associated with gingivitis and lymphocytic plasmatic stomatitis [23]. Rarer causes include FHV, FIV and FeLV [24, 25].
- Anodontia / Oligodontia - reduction or complete absence of teeth (without an inflammatory process, present in young animals).
- Eosinophilic granuloma complex - usually perioral lesions (eg, ulcers in the mouth, skin, and other organs) and other skin lesions.
- Mandibular osteosarcoma
- Oral carcinoma
- Oral melanoma
Diagnostics
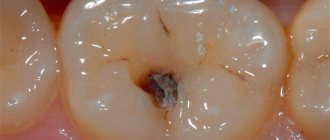
Looking at the photo of purulent pulpitis, you can see the presence of a deep carious cavity with softened dentin, emitting a putrid odor. The color of dentin can be light in acute forms of the disease, and dark in chronic ones. On the mucous membrane around the diseased tooth you can see a whitish coating and (sometimes) swelling of the transitional fold.
During probing and percussion, a pronounced pain reaction is observed. When you press on the layer that separates the tooth cavity, pus is released and a throbbing pain appears, which subsides as the pus drains. All these signs are identified by a dentist during a visual examination. In addition, radiography and electroodontodiagnostics are prescribed to diagnose the disease.
Differential diagnosis of acute purulent pulpitis requires that this disease be distinguished from:
- diffuse pulpitis in the acute phase - with it there is no pus and pain symptoms are not so intense;
- focal pulpitis - characterized by the absence of purulent discharge and weaker pain;
- purulent periodontitis - characterized by sharp “shooting” pain in the affected tooth at the slightest pressure on it;
- trigeminal neuralgia - there is no feeling of discomfort during thermal exposure, but pain occurs when touching certain points on the face.
Cost of periodontitis treatment
The price for treatment of periodontitis in a dental clinic will depend on the area and degree of damage (fibrous, granulosa or granulomatous periodontitis), the general price level in a particular medical institution and the number of visits to the doctor that will be needed to carry out the planned course. Typically, the cost of treatment is also directly dependent on the number of tooth canals: for single-canal – 5,000-10,000 rubles, two-canal – 6,000-12,000 rubles, three-canal – 8,000-20,000 rubles.
Treatment of purulent pulpitis
It is worth noting that few people can endure the acute pain characteristic of purulent pulpitis, therefore, as a rule, patients turn to the dentist already on the first/second day of the onset of the disease. The acute form of purulent pulpitis responds well to treatment, especially when using modern techniques.
When treating focal pulpitis, it is possible to preserve the pulp with restoration of its functioning, but depending on the situation, they often resort to removing it from the canals, which are thoroughly washed and filled. Treatment of acute purulent pulpitis involves depulpation, which can be carried out using the vital or non-vital method. The first method consists of the following steps:
- removal of affected tissues of the carious cavity;
- carrying out treatment with antiseptic drugs;
- removal of pulp from the coronal part of the tooth;
- removal of pulp from the root part of the tooth;
- root canal filling;
- tooth filling.
Thus, all necessary manipulations are carried out in one visit - in contrast to the devital method, which requires two visits to the dentist:
- The first involves cleaning with an antiseptic, opening the pulp, applying a special paste and installing a temporary filling;
- In the second, which is carried out after 1–10 days, the dead pulp is removed.
The Dentistry Department of the CELT Clinic has modern technologies, equipment and high-quality materials that make it possible to successfully treat purulent pulpitis.
Literature
- Gaskell RM, Gruffydd-Jones TJ (1977) Intractable feline stomatitis. Veterinary Annual 17:195-199
- Gaskell RM, Bennet M (2001). Doenças Infecciosas Felinas In Dunn JK. Tratado de Medicina de Pequenos Animais pp:953-978
- Gruffyd-Jones TJ (1991). Gingivitis and Stomatitis. In August JR. Consultations in Feline Internal Medicine Vol 3 pp:397-402
- Andrade, M (2002) Antiinflamatorios esteroidais. In Spinosa HS, Górniak SL, Bernardi MM: Farmacologia aplicada à medicina veterinária. Rio de Janeiro, Guanabara Koogan, pp:240-252
- August JR (1992), Molestias virais felinas. In: Ettinger SJ: Tratado de Medicina Interna Veterinária. 3 ed. São Paulo p 340-6.
- Barlough JE, et al (1991). Acquired immune dysfunction in cats with experimentally induced feline immunodeficiency virus infection: comparison of short-term and long-term infections. Journal of Acquired Immune Deficiency Syndrome 4(3):219-27
- Barr MC, et al (2000). Exogenous glucocorticoids alter parameters of early feline immunodeficiency virus infection. Journal of Infectious Diseases 181(2):576-586
- Holzangel E, et al (1998) The role of in vitro-induced lymphocyte apoptosis in feline immunodeficiency virus infection: correlation with different markers of disease progression. Journal of Virology 72:9025-33
- Knowles JO, Gaskell RM, Gaskell CJ, Harvey CE, Lutz H (1989). Prevalence of feline calicivirus, feline leukemia virus and antibodies to FIV in cats with chronic stomatitis. The Veterinary Record 1:336-338
- Harvey CE (1991) Oral inflammatory diseases in cats. Journal of American Animal Hospital Association 27:585-591
- Harvey CE (1994) Oral and dental diseases. In Sherding RG. The Cat: Diseases and Clinical Management 2nd Ed: pp:1117-1151
- Beebe AM, Dua N, Faith TG, Moore PF, Pedersen NC, Dandekar S (1994). Primary stage of feline immunodeficiency virus infection: viral dissemination and cellular targets. Journal of Virology 68:3080-91
- Bendinelli M, et al (1995) Feline immunodeficiency virus: an interesting model for AIDS studies and an important cat pathogen. Clinical Microbiology Review 8:87-112
- Ceballos-Salobrena A, et al (2000). Oral lesions in HIV/AIDS patients undergoing highly active antiretroviral treatment including protease inhibitors: a new face of oral AIDS? AIDS Patient Care 14:627–635
- Comcen.com
- Pérez-Salcedo L et al (2011) Comparison of two sampling methods for microbiological evaluation of periodontal disease in cats. Vet Microbiol 149(3-4):500-50
- Dolieslager SM et al (2011) Identification of bacteria associated with feline chronic gingivostomatitis using culture-dependent and culture-independent methods. Vet Microbiol 148(1):93–98
- Pérez-Salcedo L et al (2013) Isolation and identification of Porphyromonas spp. and other putative pathogens from cats with periodontal disease. J Vet Dent 30(4):208–213
- Dolieslager SM et al (2013) The influence of oral bacteria on tissue levels of Toll-like receptor and cytokine mRNAs in feline chronic gingivostomatitis and oral health. Vet Immunol Immunopathol 151(3-4):263-274
- Pérez-Salcedo L et al (2011) Comparison of two sampling methods for microbiological evaluation of periodontal disease in cats. Vet Microbiol 149(3-4):500-503
- Hess MO (2009) Necrotizing fasciitis due to Prevotella bivia in a cat. J Small Anim Pract 50(10):558–560
- Dowers, KL et al (2010) Association of Bartonella species, feline calicivirus, and feline herpesvirus 1 infection with gingivostomatitis in cats. JFMS 12:314-321
- Belgard S et al (2010) Relevance of feline calicivirus, feline immunodeficiency virus, feline leukemia virus, feline herpesvirus and Bartonella henselae in cats with chronic gingivostomatitis. Berl Munch Tierarztl Wochenschr 123(9-10):369-376
- Hartmann K (2005). Feline immunodeficiency virus and related diseases. In Ettinger SJ & Feldman EC. Textbook of Veterinary Internal Medicine 6th Edn: pp:659-662
- Hartmann K (1998) Feline immunodeficiency virus infection: an Overview. The Veterinary Journal 155:123 – 137
- Hennet PR et al (2011) Comparative efficacy of a recombinant feline interferon omega in refractory cases of calicivirus-positive cats with caudal stomatitis: a randomized, multi-centre, controlled, double-blind study in 39 cats. J Feline Med Surg 13(8):577–587
- Corbee RJ et al (2011) Inflammation and wound healing in cats with chronic gingivitis/stomatitis after extraction of all premolars and molars were not affected by feeding of two diets with different omega-6/omega-3 polyunsaturated fatty acid ratios. J Anim Physiol Anim Nutr (Berl) Jul 18
- Cohn LA (1997). Glucocorticosteroids as immunosuppressive agents. Seminars in Veterinary Medicine and Surgery (Small Animal) 12:150-156
- Daniel AGT, Reche Jr A (2005). Oral bacteria from cats with gingivitis and feline immunodeficiency virus. Online Journal of Veterinary Research 9:74-78
^Top