The tissues surrounding the tooth and located in the space between the root and the alveoli are called periodontal. Periodontal tissues are mainly composed of connective tissues. From these connective tissues, the periodontal ligament is formed, which connects the cementum of the tooth with the bone tissue of the alveoli.
Periodontal tissues contain blood and lymphatic vessels, as well as nerve endings and nerve bundles.
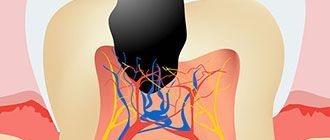
So, inflammation of the tissues in the area of the apical foramen is called periodontitis or apical periodontitis, and inflammation of the tissues surrounding the root of the tooth is called periodontitis.
Acute apical periodontitis
Acute periodontitis has 2 stages: The first stage is the intoxication phase. At this stage, the pain is long-lasting and constant. There may be pain when biting.
The second stage is the exudation phase.
It is characterized by continuous, prolonged pain, as well as pain when biting. Percussion is sharply painful. The pain radiates. Due to exudate and inflammatory acidosis, collagen fibers first swell and then melt. After this, the tooth can become mobile. X-ray examination showed no changes in the periodontium.
Features of the development of purulent periodontitis
In the absence of treatment, the focus of inflammation grows, the amount of pus increases, and then the abscess breaks out in one or more directions. The most favorable is considered to be the outflow of purulent masses into the tooth cavity through the root canals, but another scenario for the development of the disease is also possible.
In this case, periodontitis degenerates into periostitis of the jaw bone, which occurs due to the spread of pus under the periosteum of the alveoli. Pus can also flow directly into the oral cavity through a fistula formed in the gum.
Advanced purulent periodontitis can cause the development of sinusitis, osteomyelitis, and phlegmon of the maxillofacial area. Only high-quality and timely treatment of the source of inflammation can avoid the risk of these complications.
Chronic granulating periodontitis
This form of periodontitis occurs with severe and prolonged pain. A fistula appears. Pus is released from the fistula. The gums around the tooth are swollen. If we press on the gum with some kind of dental instrument, for example a smoothing iron, then a depression will appear behind it.
X-ray examination reveals bone loss around the tooth with unclear boundaries. Consequently, the cement and dentin of the tooth are destroyed.
Treatment
Treatment of apical P. includes endodontic (intracanal), physiotherapeutic and surgical methods.
Instrumental endodontic treatment of the tooth root canal (its expansion, removal of decayed tissue) is an important stage of treatment. In order to influence the microflora of the tooth root canal, antimicrobial treatment is carried out. For this purpose, decamine, decamethoxin, iodinol, chloramine, hydrogen peroxide, gastric juice, nitrofuran drugs (furacilin, furagni, etc.), bactrim, dimexide are used.
Filling the tooth root canal is regarded as the most important stage in the treatment of tooth root canal. The choice of filling material (see) depends on the shape of the tooth root canal, the structural features of the tooth root canal, and the age of the patient. In this case, pins are widely used.
Hyposensitizing therapy for P. involves transcanal administration of glucocorticoids (hydrocortisone emulsion) or oral administration of antihistamines.
Treatment of acute serous P. consists of removing the filling or trephination of the tooth crown, rapid evacuation of necrotic masses from the tooth root canal. In cases of toxic damage to the periodontium, antidotes are used (for example, unithiol, iodinol), and agents with an anti-exudative effect are used (furazolin solution, hydrocortisone emulsion, etc.). All of these agents are injected into the root canal of the tooth. Then the canal is filled within the opening of the tooth apex with hardening pastes.
In the treatment of acute purulent and aggravated chronic. P. it is necessary to create conditions for the outflow of purulent exudate through the tooth root canal; if this is not possible, they resort to an incision in the gum along the transitional fold or tooth extraction. The root canal remains open for 7-10 days. Sulfonamides, antibiotics, painkillers, hyposensitizing agents are prescribed internally, and a course of physiotherapy is carried out. All manipulations on the tooth for acute and aggravated chronic conditions. P. is carried out under local anesthesia. After the inflammatory phenomena subside, medicinal and instrumental endodontic treatment of the tooth root canal is performed, filling it with hardening pastes (for acute purulent P.), cements (for exacerbation of chronic P.). It is advisable to use gutta-percha or silver points.
Chron. It is better to eliminate infectious foci in the area of single-rooted teeth surgically. Several methods have been proposed for surgical treatment of P.: resection of the apex of the tooth root (apicotomy), tooth replantation, hemisection, amputation of the tooth root, coronoradicular separation. Multi-rooted teeth with chronic, granulomatous forms of P. should be removed.
Rice. 6. Scheme of resection of the apex of the tooth root for chronic periodontitis (operation stages): a - arcuate incision of the gum in the area of the operated tooth root; b — formation of a mucoperiosteal flap; c — the wall of the dental alveolus is trepanned, the root of the tooth is exposed; d — resection of the tooth root (1) with a fissure bur (2); e - expansion of the tooth canal (1) with a reverse-cone bur (2) - e - tooth root is filled with amalgam (1), the bone cavity is filled with bone filings and formalized bone (2); g — the mucoperiosteal flap is placed in place and fixed with sutures.
Resection of the apex of the tooth root is indicated in the presence of long-existing fistulas, underfilling of the tooth root canal, breakage of the instrument in the canal, excessive removal of the pin and filling material beyond the apex of the tooth root, cystogranuloma, as well as in all cases where transcanal endodontic treatment of the tooth is impossible (obliteration, curvature of the tooth root canal). The operation is performed under local infiltration or conduction anesthesia with the following steps: incision (arcuate or trapezoidal), formation of a mucoperiosteal flap, trepanation of the wall of the dental alveolus or expansion of the defect, if present, to expose the apex of the tooth root, resection of the tooth root, removal of granulation tissue and epithelium, formation of a cavity in the tooth root (expansion of the lumen of the tooth root canal with an inverted cone-shaped bur) and filling it with amalgam, suturing (Fig. 6).
Tooth replantation (see Replantation) is performed under local anesthesia, while the root canals of the extracted tooth are filled with amalgam or cement (often retrograde). After such treatment, the tooth is placed in a physiological solution, the dental alveolus is carefully treated with a curette, washed with warm physiological solution and the tooth is inserted into it, after which a splint is applied. The engraftment of the tooth depends on the type of fusion of the replanted tooth with the tissues, and the period of its preservation, according to V. A. Kozlov (1974), varies from 4 to 12 years.
Hemisection and amputation of tooth roots are indicated in the presence of deep bone pockets, exposure of the tooth root, caries of cement and dentin of one of the roots, perforation of the tooth root, obstruction of the tooth root canal, a progressive inflammatory-destructive process at the apex of the tooth root. Hemisection - removal of one of the roots (usually the medial root of the lower molars) and the crown of the tooth using the second half of the tooth under a bridge - is carried out with or without the formation of a mucoperiosteal flap. After filling the root canal and carious cavity, the tooth is dissected under local anesthesia and half of it is removed. The remaining part of the tooth serves as a support for the bridge.
Tooth root amputation involves removing one or two tooth roots while preserving or reshaping the crown, i.e., removing with a bur that part of the crown that corresponds to the amputated root. Amputation is carried out on the large molars of the upper jaw, and one or two cheek roots or only the palatal root of the tooth can be removed. It is better to carry out the operation without cutting out a mucoperiosteal flap; in this case, a wedge-shaped excision of a small part of the tooth crown is carried out with a bur and thus the area of origin of the tooth root to be removed is exposed. After cutting the bifurcation zone, the root is easily removed with an elevator or forceps.
Coronoradicular separation consists of cutting the tooth into pieces and then connecting the roots of the tooth under one common crown. The operation is indicated in the presence of perforation of the bottom of the tooth cavity, destructive changes, idiopathic resorption in the area of bifurcation of the roots of the lower molars. Under local anesthesia with a diamond bur, the tooth is cut into two halves, the overhangs are removed, and curettage (curettage) is performed in the bifurcation area. Subsequently, soldered crowns are made for each of the roots.
Complications during treatment:
periodontal burn during diathermocoagulation, removal of excess amount of cement or pin beyond the apex of the tooth root, perforation of the bottom of the tooth cavity or the wall of the root canal, underfilling of the root canal, breakage of the instrument in the canal.
Rice.
7. Intraoral radiographs of the upper anterolateral teeth in chronic periodontitis before treatment (a) and 2 years after treatment (b): a - cyst-granuloma (indicated by an arrow) at the apex of the second premolar root immediately after filling the tooth; b — the focus of rarefaction (indicated by an arrow) decreased after endodontic treatment. Long-term results of endodontic treatment of apical P. depend on sterilization and instrumental treatment of the tooth root canal, the nature of the filling material, wedge, forms of P., the size of the focus of destruction, and the adequacy of filling the root canal (Fig. 7, a, b).
Treatment of marginal P. involves eliminating the effect of etiol, factor (correction of a crown or filling, removal of tartar and excess filling material from the interdental space). Good results are obtained by treating the gum edge with antiseptics (hydrogen peroxide, iodinol, etc.), nitrofuran derivatives (furacilin, furagin), enzymes, and combination drugs (inhalipt, bactrim). Treatment of hron, regional P. is reduced to curettage (scraping) of the periodontal pocket under infiltration (1 - 2% solution of novocaine, trimecaine, lidocaine) or topical anesthesia (using lidocaine emulsion, pyromecaine ointment with collagen).
Forecast
with timely treatment, P. is favorable; In most cases, teeth can be saved.
Prevention of purulent periodontitis
As noted earlier, the purulent stage of periodontitis most often develops after the end of the serous stage, therefore, first of all, you need to try to prevent it. The main preventive measures for this are oral hygiene and dental health monitoring.
In most cases, purulent periodontitis is of an infectious nature; inflammation occurs under the influence of a large number of pathogenic bacteria. The creation of the correct microflora of the oral cavity can avoid their penetration into periodontal tissues and subsequent reproduction. Invaluable assistance in this will be provided by the ASEPTA SENSITIVE toothpaste and ASEPTA mouthwash, which actively counteract the development of microorganisms and fungal infections, significantly reducing the risk of periodontitis.
Regularity, quality and duration of teeth brushing also play an important role in reducing the likelihood of developing an inflammatory process. Brush your teeth at least twice a day for 2-3 minutes, rinse them after every meal and never allow yourself to go to bed without doing hygiene procedures - and your teeth will always be beautiful and healthy.
It should also be remembered that in most cases, periodontitis ends with untreated caries. If you ignore a small dark spot or a shallow carious cavity, you risk getting pulpitis, which over time turns into periodontitis. Do not neglect scheduled visits to the dentist and immediately consult a doctor as soon as you suspect the first symptoms of any dental and gum disease.