Causes of stomatitis
The imperfection of local and general defenses of the child’s body makes the mucous membranes of the oral cavity vulnerable to adverse factors. And the healthy curiosity characteristic of every child has made stomatitis one of the most common diseases among children. Sometimes, for the development of an illness, it is enough to taste any less than sterile object. The main causes of the disease include the following:
- insufficiently good oral hygiene;
- minor injuries - cheek biting, scratch, etc.;
- burns, including chemical burns;
- exposure to pathogens from unwashed hands or dirty toys.
Dentists focus on stomatitis associated with biting the inside of the cheek.
This is often associated with recent dental treatment under local anesthesia. For some time after the procedure, there is reduced sensitivity in the area of the lip or cheek, so you need to eat food after treatment very carefully and only after you have waited for the recommended period of time - usually from 1 to 2 hours. The likelihood of developing stomatitis for these reasons increases after infectious diseases, previous interventions, hypothermia and other factors that contribute to a decrease in protective forces.
The best medicinal antipyretics
Body hyperthermia brings a lot of discomfort, especially to infants. Therefore, every mother should have antipyretic drugs in her home medicine cabinet.
Thanks to their pharmacological action, they significantly alleviate the child’s condition: they relieve pain, eliminate body aches and relieve inflammation. Pediatricians identify the following most effective medications among such drugs.
| Drug name | Features of application |
| Ibuprofen | Effect:
Acceptable age:
Mode of application: Suppositories are administered rectally: for infants up to one year, 1 suppository three times a day with an interval of 8 hours. Children over one year old: 1 suppository four times a day with an interval of 6 hours. The daily dose of the drug should not exceed 30 mg per 1 kg of body weight of the child. Suspension:
|
| Paracetamol | Effect:
Acceptable age:
Mode of application: Suppositories are administered rectally 2–4 times a day. The suspension is taken before meals 3-4 times a day. A single dose should not exceed 10 mg/kg, and a daily dose should not exceed 60 mg/kg. Tablets 0.5 g 4 times a day. The maximum daily dose should not exceed 4 g. |
| Viburkol | Effect:
Acceptable age: From 0 to 14 years Mode of application: Newborns and children up to 3 years old: 1 suppository 1 – 2 times a day; 3 – 6 years, 1 suppository 2 – 3 times a day, for acute conditions, 1 suppository every half hour; 6 – 14 years: 1 suppository 3 – 4 times a day, acute conditions will require the administration of a suppository every 30 minutes. |
| Panadol | Effect:
Acceptable age:
Mode of application: The suspension is intended for oral administration with a single dose of 15 mg/1 kg 3–4 times a day. Suppositories aged from 6 months to 2.5 years, 1 suppository at a dose of 125 mg; 3 – 6 years: 1 suppository at a dose of 250 mg. 3 – 4 times a day. The maximum dose of the drug per day should not exceed 60 mg/1 kg. |
| Efferalgan | Effect:
Acceptable age:
Mode of application: A single dosage of syrup is prescribed taking into account the child’s body weight 10 mg/1 kg three times a day with an interval of 4 – 6 hours. Suppositories are administered rectally no more than 2 times a day in a dosage of 125–250 mg, depending on the age of the patient. |
Important! The use of an antipyretic drug, its dosage and regimen should be prescribed exclusively by a doctor. It takes into account the child’s age, body weight, and the clinical picture of stomatitis.
How to choose the right antipyretic drug for a child:
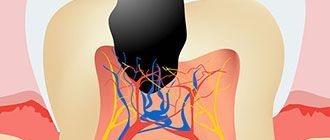
Types of stomatitis
The treatment regimen for stomatitis in children is based on the type of disease. There are several types of stomatitis:
- bacterial;
- viral, including herpes;
- fungal;
- aphthous;
- angular;
- allergic;
- traumatic.
All types of stomatitis occur in children, but the most common among children under 3 years of age are aphthous, candidal, herpetic and allergic. An increase in the incidence of traumatic stomatitis is usually associated with a period of active growth of primary teeth.
It is important to understand that in some cases, stomatitis is combined with other diseases with similar symptoms and is the first sign of more serious diseases. For example, with cheilitis - inflammation of the mucous membrane and red border of the lips, food allergies, etc.
Symptoms
Common symptoms of stomatitis are pain, burning, swelling of the mucous membrane and redness, and bad breath. Salivation also changes - it can be excessive or insufficient, with dry mouth. In some cases, there may be an increase in temperature and enlargement of the submandibular lymph nodes.
The types of stomatitis in children and treatment methods differ, as do the specific manifestations. For example, with aphthous stomatitis, only one large ulceration may appear, but with viral stomatitis, inflammation almost always takes the form of numerous elements or a rash merging into one focus.
Candidal stomatitis is characterized by the formation of a white or yellowish cheesy coating. It is easier to recognize traumatic stomatitis because it is preceded by damage or the source of injury is nearby - a chipped tooth or a rough filling.
Traditional methods
Often, parents use alternative medicine methods as an auxiliary therapy for reducing the child’s body temperature.
The most common in this case is rubbing the baby. For this, the following solutions are used:
- Acetic
- Alcoholic
- Herbal
- Vodka
They are prepared independently using warm water to which the main ingredient is added. In this case it is important to prepare a weak solution , since its composition contains a high concentration of alcohol, vodka and vinegar that can harm the baby’s health and also lead to skin burns.
It is also important to strictly follow the rubbing technique, which consists of sequentially treating the main parts of the body and folds of skin in infants. It is also important to take into account the intensity of rubbing. Palms and heels can be rubbed intensively, and other areas should be gently wiped with a damp cloth or simply sprayed with the solution.
Attention! Pediatricians strictly prohibit the use of vinegar and alcohol solutions if the child has dermatological rashes or any damage to the skin.
Komarovsky on reducing temperature in children without medication:
Diagnostic features
A dentist can detect stomatitis during the first visual examination. But in controversial cases, laboratory tests may be required. Thus, bacterial inflammation may require identification of the causative agent of the disease and its sensitivity to antibiotics. A scraping and/or virological study will help determine the cause of the disease and prescribe appropriate treatment.
If a combination of several ailments with a similar picture is suspected, as well as if the child’s general well-being deteriorates, laboratory tests of blood and urine and consultations with other specialists may be prescribed.
Sometimes stomatitis can be the first manifestation of systemic diseases, general somatic pathology, for example, diabetes mellitus or malignant neoplasms. Therefore, a timely visit to the doctor is extremely important.
Features of treatment
As is often the case with diseases that are at the intersection of several areas of medicine, inflammatory lesions of the oral mucosa are one of the least studied areas of dentistry. Therefore, several specialists can be involved in the treatment of stomatitis in children in the mouth: pediatrician, dentist, dermatologist, immunologist-allergist, otolaryngologist, etc. This is especially convenient when you go to a multidisciplinary clinic.
Self-medication of stomatitis is unacceptable, and although it is now easy to find ready-made treatment regimens and folk recipes, it is important not to experiment with the baby’s health.
Conservative treatment is mainly used, which involves treating the underlying cause of the disease. Your doctor may prescribe the following medications:
- antibacterial drugs (systemic and local in the form of ointments): for bacterial inflammation;
- antiviral agents for herpes and other types of viral stomatitis;
- antifungal drugs for fungal diseases;
- antihistamines - both for allergic origin of stomatitis, and as part of complex therapy to reduce swelling and itching;
- symptomatic drugs - anti-inflammatory, analgesic, antipyretic.
Treatment of candidal stomatitis in infants should be carried out with caution. At the same time, it is important to pay attention to your health; sometimes the cause of such a disease can be insufficient breast hygiene during lactation.
Often, only local remedies are sufficient, but make sure that the entire oral cavity is treated with the rinse - inflammatory agents can be found on the entire surface of the mucous membranes. Healing applications can be used to a limited extent, only on areas of inflammation.
Treatment of stomatitis of any kind in children involves strict adherence to a diet. The diet should be gentle, it is important to avoid salty, spicy, sour foods and drinks, serve the child warm meals, and limit the consumption of sweets.
If traumatic stomatitis occurs, the doctor will prescribe medications to speed up healing. However, it is very important to prevent re-injury. If it was caused by sharp edges of a tooth or filling, this cause should be eliminated. The doctor will suggest grinding off the filling or replacing it, and will also choose the appropriate option for restoring the shape of the crown in case of chips and cracks.
Clinic, diagnosis and treatment of acute herpetic stomatitis in children
- What is the clinical picture of acute herpetic stomatitis?
- What are the new treatment regimens?
The problem of diseases of the oral mucosa is one of the most important in dentistry.
Acute herpetic stomatitis occupies a special place here, primarily because it accounts for more than 80% of all diseases of the oral mucosa in children. The combined use of virological, serological and immunofluorescence research methods confirms that acute herpetic stomatitis is one of the clinical forms of primary herpetic infection.
The spread of the disease in 71% of cases among children aged 1 to 3 years is explained by the fact that at this age, antibodies received from the mother interplacentally disappear in children, as well as the lack of mature specific immune systems. Among older children, the incidence is significantly lower due to acquired immunity after a herpes infection in its various clinical manifestations.
Great importance in the pathogenesis of the disease is attached to the lymph nodes and elements of the reticuloendothelial system, which is quite consistent with the pathogenesis of the sequential development of clinical signs of stomatitis. The appearance of lesions on the oral mucosa is preceded by lymphadenitis of varying severity. Most often they are observed in severe and moderate stomatitis. As a rule, lymphadenitis is bilateral, submandibular. However, with moderate and severe forms of the disease, simultaneous involvement of the cervical lymph nodes in the process is also possible. Lymphadenitis accompanies the entire period of the disease and persists for 7-10 days after complete epithelization of the elements.
The body's resistance to the disease is determined by its immunological defense. Both specific and nonspecific immune factors play a role in immunological reactivity. Violation of nonspecific immunological reactivity determines the severity of the disease and the periods of its development. Moderate and severe forms of stomatitis led to a sharp suppression of natural immunity, which was restored 7-14 days after the child’s clinical recovery.
The severity of acute herpetic stomatitis is assessed by the severity and nature of toxicosis and damage to the oral mucosa. The development of the disease goes through five periods: incubation, prodromal, period of disease development, extinction and clinical recovery.
| Elements of herpetic stomatitis |
The mild form of acute herpetic stomatitis is characterized by an external absence of symptoms of intoxication; the prodromal period is clinically absent.
The disease begins suddenly with an increase in temperature to 37-37.5°C. The general condition of the child is quite satisfactory. In the oral cavity there are signs of hyperemia and slight swelling, mainly in the area of the gingival margin (catarrhal gingivitis). In most cases, against the background of increased hyperemia, single or grouped lesions appear in the oral cavity, the number of which usually does not exceed six. The rashes are one-time only. The duration of the disease development is 1-2 days.
The period of extinction of the disease is longer. Within 1-2 days, the elements acquire a marble-like color, their edges and center are blurred. They are already less painful. After epithelialization of the elements, the phenomena of catarrhal gingivitis persist for 2-3 days, especially in the area of the anterior teeth of the upper and lower jaw.
In children suffering from this form of the disease, as a rule, there are no changes in the blood, sometimes only towards the end of the disease a slight lymphocytosis appears (in children 1-3 years old, the number of lymphocytes is normally up to 50%). Herpetic complement-fixing antibodies are not often detected during convalescence. In this form, the protective mechanisms of saliva are well expressed: pH 7.4±0.04, which corresponds to the optimal state. At the height of the disease, the antiviral factor interferon appears in saliva from 8 to 12 units/ml. The decrease in lysozyme in saliva is not pronounced.
The moderate form of acute herpetic stomatitis is characterized by fairly clearly defined symptoms of toxicosis and damage to the oral mucosa during all periods of the disease. Already in the prodromal period, the child’s well-being worsens, weakness, loss of appetite appear, the child is capricious, there may be catarrhal tonsillitis or symptoms of an acute respiratory disease. The submandibular lymph nodes enlarge and become painful. The temperature rises to 37-37.5°C.
As the disease progresses (catarrhal phase), the temperature reaches 38-39°C, headache, nausea, and pale skin appear. At the peak of the rise in temperature, increased hyperemia and severe swelling of the mucous membrane, elements of the lesion appear both in the oral cavity and on the skin of the face in the perioral area. In the oral cavity there are usually from 10 to 20-25 lesions. During this period, salivation increases, saliva becomes viscous and viscous. Severe gingivitis and bleeding gums are noted.
Rashes often recur, as a result of which, when examining the oral cavity, one can see elements of the lesion that are at different stages of clinical and cytological development. After the first eruption of lesions, body temperature usually drops to 37-37.5°C. However, subsequent rashes are usually accompanied by a rise in temperature to the previous levels. The child does not eat, sleeps poorly, and symptoms of secondary toxicosis increase.
An ESR of up to 20 mm/hour is observed in the blood, often leukopenia, sometimes slight leukocytosis. Band and monocytes within the higher limits of normal, lymphocytosis and plasmacytosis. An increase in the titer of herpetic complement-fixing antibodies is detected more often than after suffering a mild form of stomatitis.
The duration of the period of extinction of the disease depends on the resistance of the child’s body, the presence of carious and damaged teeth in the oral cavity, and irrational therapy. The latter factors contribute to the fusion of lesion elements, their subsequent ulceration, and the appearance of ulcerative gingivitis. Epithelization of the lesion elements takes up to 4-5 days. Gingivitis, severe bleeding and lymphadenitis last the longest.
With a moderate course of the disease, the pH of saliva becomes more acidic, reaching 6.96 ± 0.07 during rashes. The amount of interferon is less than in children with a mild course of the disease, but does not exceed 8 units/ml and is not detected in everyone. The content of lysozyme in saliva decreases more than in mild forms of stomatitis. The temperature of the unchanged oral mucosa is in accordance with the child’s body temperature, while the temperature of the affected elements in the degeneration stage is 1.0-1.2°C lower than the temperature of the unchanged mucosa. With the beginning of regeneration and during the period of epithelization, the temperature of the affected elements rises to 1.80 and remains at a higher level until complete epithelization of the affected mucosa.
The severe form of acute herpetic stomatitis is much less common than the moderate and mild form.
During the prodromal period, all the signs of an incipient acute infectious disease occur: apathy, adynamia, headache, musculocutaneous hyperesthesia and arthralgia, etc. Symptoms of damage to the cardiovascular system are often observed: bradycardia and tachycardia, muffled heart sounds, arterial hypotension. Some children experience nosebleeds, nausea, vomiting, and pronounced lymphadenitis of not only the submandibular, but also the cervical lymph nodes.
During the development of the disease, the temperature rises to 39-40°C. The child has a mournful expression on his lips and painfully sunken eyes. There may be a mild runny nose, coughing, and the conjunctivae of the eyes are somewhat swollen and hyperemic. Lips are dry, bright, parched. In the oral cavity, the mucous membrane is swollen, clearly hyperemic, with pronounced gingivitis.
After 1-2 days, lesions up to 20-25 begin to appear in the oral cavity. Often, rashes in the form of typical herpetic blisters form on the skin of the perioral area, the skin of the eyelids and conjunctiva of the eyes, the lobes of the ears, on the fingers, like a panaritium. Rashes in the oral cavity recur, and therefore at the height of the disease in a seriously ill child there are about 100 of them. The elements merge, forming extensive areas of mucosal necrosis. Not only the lips, cheeks, tongue, soft and hard palate are affected, but also the gingival margin. Catarrhal gingivitis turns into ulcerative-necrotic. A sharp putrid odor from the mouth, profuse salivation mixed with blood. Inflammation in the mucous membranes of the nose, respiratory tract, and eyes worsens. Streaks of blood are also found in secretions from the nose and larynx, and sometimes nosebleeds are observed. In this condition, children need active treatment from a pediatrician and dentist, and therefore it is advisable to hospitalize the child in a boxed ward of a children's or infectious diseases hospital.
In the blood of children with severe stomatitis, leukopenia, a band shift to the left, eosinophilia, single plasma cells, and young forms of neutrophils are detected. In the latter, toxic granularity is very rarely observed. Herpetic complement-fixing antibodies are, as a rule, always detected during the period of convalescence.
Saliva has an acidic environment (pH 6.55±0.2), which can then be replaced by more pronounced alkalinity (8.1-8.4). Interferon is usually absent, the content of lysozyme is sharply reduced.
The diagnosis of acute herpetic stomatitis is made based on the clinical picture of the disease. The use of virological and serological diagnostic methods, especially in practical healthcare, is difficult. This is primarily due to the difficulty of conducting special research methods. In addition, with these methods, results can be obtained at best towards the end of the disease or some time after recovery. Such a retrospective diagnosis cannot satisfy the clinician.
It should be emphasized that in recent years the immunofluorescence method has been increasingly used. The high percentage of coincidences (79.0±0.6%) of the diagnosis of acute herpetic stomatitis, according to immunofluorescence data, with the results of virological and serological studies make this method the leading one in diagnosing the disease.
The doctor’s tactics when treating patients with acute herpetic stomatitis should be determined by the severity of the disease and the period of its development.
Due to the peculiarities of the course of acute herpetic stomatitis, rational nutrition and proper organization of feeding the patient occupy an important place in the complex of therapeutic measures. Food must be complete, that is, contain all the necessary nutrients, as well as vitamins. Therefore, it is necessary to include fresh vegetables, fruits, berries, and juices in your diet. Before feeding, the oral mucosa should be anesthetized with a 2-5% solution of anesthetic emulsion.
The child is fed predominantly liquid or semi-liquid food that does not irritate the inflamed mucous membrane. It is necessary to give the child enough fluids. This is especially important during intoxication. During meals, natural gastric juice or its substitutes should be given, since when there is pain in the mouth, the enzymatic activity of the stomach glands reflexively decreases.
Local therapy for acute herpetic stomatitis has the following objectives:
- relieve or reduce painful symptoms in the oral cavity;
- prevent repeated eruptions of lesions (reinfection) and promote their epithelization.
From the first days of the disease, given its etiology, in local treatment, serious attention should be paid to antiviral therapy. For this purpose, it is recommended to use 0.25% oxolinic, 0.5% tebrofen ointments, Zovirax, solutions of interferon and neoferon.
It is recommended to use the listed medications repeatedly (3-4 times a day) not only when visiting a dentist, but also at home. It should be borne in mind that antiviral agents must be applied to both the affected areas of the mucosa and areas that do not contain elements of the lesion, since they have more of a preventive effect than a therapeutic one.
During the period of extinction of the disease, antiviral drugs can be discontinued.
Particular importance should be attached to keratoplasty agents at this time. These are primarily oil solutions A and B, sea buckthorn oil, caratoline, rosehip oil, ointments with methyluracil, and an oxygen cocktail.
A study of the state of local immunity in children with acute herpetic stomatitis revealed that it correlates with the nature of the pathological process, therefore we consider it pathogenetically justified to include measures aimed at their elimination in a comprehensive treatment regimen.
At the Department of Pediatric Therapeutic Dentistry of the Moscow State Medical University, the drug imudon from Solvay pharma was prescribed to 80 children aged 2 to 4.5 years in the complex treatment of acute herpetic stomatitis. 40 children were diagnosed with mild, 38 children with moderate and 2 with severe forms of stomatitis.
Imudon is a mixture of lysates: 0.050 g (dry product) Lactobassillus acidophilus, fermentatum, helveticus, lactis Streptococcus pyogenes (2 var.), faecalis, faecium, sanguinis Staphilococcus aureus Klebsiella pneumoniae, Corynebacterium pseudodiphteriticum, Fusiformis fusiformis, Candida albicans.
Preservative: Sodium mercurothiolate: 0.0125 mg.
Excipients: lactose, mannitol, saccharin, sodium bicarbonate, anhydrous citric acid, precirol fine, magnesium stearate, polyvinylpyrrolidone.
pharmachologic effect
Imudon is intended for local specific immunotherapy of diseases of the oral cavity and pharynx. The effect of the drug on the immune system is expressed in an increase in the phagocytic activity of macrophages, an increase in the content of lysozyme in saliva, as well as an increase in the number of immunocompetent cells and the content of local antibodies (class A immunoglobulins). Thus, imudon has a therapeutic specific antimicrobial and anti-inflammatory effect, and also, by increasing the immune local protective barrier, ensures the prevention of relapses.
The first group consisted of children treated with 0.5% tebrofen ointment, the second group included children treated with interferon solution. In the third group, on the day of treatment, in addition to 0.5% tebrofen, imudon was prescribed, and in the fourth group, imudon + interferon. Children took Imudon tablets 5-6 times a day, no earlier than 30-40 minutes after treating the oral cavity with antiviral ointment, and dissolved it in the oral cavity.
Criteria for clinical and laboratory assessment of the therapeutic effectiveness of the drug imudon:
- The therapeutic effect is the average recovery time.
- Analgesic effect.
- General and local reactions to the drug.
- Influence on the state of local immunity.
Recovery was considered to be the epithelization of the lesion elements without a complete cure of the child from acute herpetic stomatitis, the duration of which is determined not only by the end of the epithelization of the lesion elements, but also by the duration of gingivitis and lymphadenitis, as well as deviations in the general well-being of the child.
As can be seen from table. 1, timely correction of local immunity increases the effectiveness of ongoing treatment measures and allows for faster recovery of children with AHS.
The effectiveness of the drug was manifested in groups 3 and 4 on the second day in case of contacting a doctor on the first day of the disease: erosions did not develop into aphthae, and the surrounding mucous membrane was not infiltrated.
Table data 1 indicate the advantage of complex therapy for OGS over generally accepted methods of treatment, its high efficiency, confirmed by a reliable reduction in the time of epithelization of elements and recovery of children.
The more effectively the drug stops the disease, the faster it normalizes the pathological infectious process, the more actively the factors of local immunological defense are restored. (Table 2).
We have given a high assessment of the effectiveness of the new regimen of complex therapy for AHS using stimulating immunotherapy, in particular imudon; It was concluded that there is a fundamental need for an integrated approach to the treatment of acute herpetic stomatitis with the mandatory inclusion of imudon, both a stimulating and a replacement agent for the correction of local immunity.
Thus, the high effectiveness of imudon in the treatment of AHS due to the immune correction of saliva has been established. Imudon has a therapeutic, anti-inflammatory effect, reduces the time for epithelization of lesions. There were no complications or side effects when using the drug imudon. Children used the drug with pleasure, as it has a pleasant, minty taste that does not irritate the mucous membrane. Apparently due to the mint aroma there is a weak analgesic effect.
All this allows us to recommend imudon in the complex therapy of acute herpetic stomatitis in children.
In conclusion, it should be noted that acute herpetic stomatitis, occurring in any form, is an acute infectious disease and requires in all cases the attention of a pediatrician and dentist in order to provide comprehensive treatment, eliminate contact of a sick child with healthy children, and take measures to prevent this diseases in children's groups.
Prevention of stomatitis
You can reduce the risk of developing stomatitis using the following recommendations:
- regular washing of toys, bottles, pacifiers, breast hygiene if the baby is breastfed;
- general strengthening activities: walks, wet cleaning, a balanced diet, moderate hardening, adherence to a daily routine;
- fighting bad habits of biting nails, pencils, etc.;
- regular dental examinations and timely interventions in case of dental injuries.
The dentists of the Family Doctor clinic treat and prevent stomatitis in children.
Advanced equipment allows us to quickly and accurately assess the condition of the oral cavity and perform the necessary studies in a short time. We practice modern approaches to the treatment of inflammatory diseases of the oral cavity and adhere to an individual approach to each small patient. Consultation with a pediatric dentist is carried out by appointment. To make an appointment, call the single contact center or fill out a special online appointment form for a pediatric dentist on the website, or you can also visit the clinic’s reception in person.