- Work examples
- Questions and answers
- Stock
- Reviews
Dentistry "NovaDent" offers services for the treatment of periodontitis at a price of 1,200 rubles in 15 of our clinics in Moscow and the Moscow region.
We will restore the healthy and beautiful condition of teeth and gums at any stage of the disease, and also teach measures to prevent periodontitis.
- Prices
- Types of periodontitis
- Stages of the disease
- Symptoms
- What contributes to the emergence?
- Diagnostics
- How is periodontitis treated?
- Implantation for periodontitis
- Is it possible to cure with folk remedies?
- Prevention
What is periodontitis?
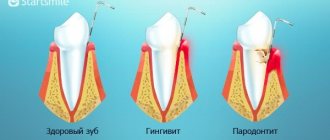
Periodontitis, or, as it is popularly called, dental periodontitis, is an inflammatory disease of the periodontal tissues that surround the tooth (gums, dental ligament and surrounding jaw bone). In professional terms, periodontitis is an inflammation of the ligaments of the tooth.
Periodontitis can be localized, that is, spread to the area of one or two teeth, or generalized, that is, affect most of the dentition. If a patient has periodontitis, it is usually chronic. Therefore, the main task of a specialist is to identify the cause of the disease, prescribe the correct treatment and, most importantly, prevent subsequent exacerbations and complications.
Plasma therapy or plasma lifting APRF and IPRF
The method is based on strengthening local immunity due to the introduction of the patient's autoplasma enriched with growth factors (I-PRF and APRF) into the periodontal tissue area.
Features of the procedure: The patient's venous blood is collected and placed in a centrifuge for several minutes to separate the plasma. Then the patient is given an injection of platelet autoplasma into the gum area.
Advantages: the method allows you to restore nutrition to the gums and activate the process of regeneration of damaged tissue.
What are the signs of periodontitis?
The initial signs of periodontitis are bleeding gums when pressing on them or when brushing teeth, bluish or red gums, and bad breath. Already in the later stages of the disease, tooth mobility and visible exposure of their roots appear, which indicates a severe and advanced form of the inflammatory process. When periodontitis becomes chronic, the tissues surrounding the tooth are “reabsorbed” and pathological gum and bone pockets are formed. As a result, the tooth gradually becomes loose and falls out.
It is necessary to distinguish the exposure of roots during periodontitis from the so-called gum recession - a decrease in the height of the gingival margin, as a result of which the root of the tooth is exposed, in other words, “sliding” or gum atrophy. Unlike periodontitis, recession is not caused by inflammation and does not entail the formation of pathological pockets and loosening of teeth. Additionally, in most cases, gum recession can be successfully treated.
Flap surgery for periodontitis
Flap surgery is indicated for patients with pronounced periodontal changes: pocket depths of more than 5 mm, active inflammation, etc. This technique allows not only to eliminate various types of deposits and granulations, but also to restore interdental defects and bone tissue defects. To form a flap, precise cuts are made in a specific direction:
- Horizontal cuts are always made. They can run either inside the gingival sulcus or parallel to the gum edge.
- Vertical incisions allow you to expand the surgical field, but lead to the formation of scar changes in the gums, so they are performed only when necessary.
Among the disadvantages of flap surgery, there is a possibility of flap displacement and exposure of the neck of the tooth. This complication worsens the aesthetics of the oral cavity, contributes to increased tooth sensitivity and the development of tooth root caries.
What are the causes of periodontitis?
Understanding the causes of the disease is a very important point, which helps the doctor correctly determine how to treat gum periodontitis. The disease can be triggered by both general and local factors. Common causes include diseases of the gastrointestinal tract, diseases associated with pathology of the endocrine system, some gynecological and urological diseases, sexually transmitted infections, and a weakened immune system. Local, or local, factors are missing teeth, malocclusion, incorrectly installed fillings or crowns, which mechanically irritate the gums and create conditions for the accumulation of bacterial plaque. A significant role is played by the specific microbial flora of the oral cavity, which occurs in some patients and causes periodontitis. But the main factor in the development of periodontitis is poor oral hygiene.
How is periodontitis diagnosed?
It is possible to determine whether a patient has periodontitis or not already at the first appointment, focusing on his complaints and the condition of the oral cavity. Moreover, when diagnosing the disease, special tests are used, the most popular of which is the Parma index. It works as follows: a special Schiller solution is applied to the gums, which reacts to unhealthy tissues and colors them in a bright color, revealing the source of inflammation. There is also an index that determines the level of bleeding, and a Russell test that reveals the condition of not only the gums, but also the bone tissue.
X-ray studies, which determine the degree of the disease that has arisen, are the main ones in the diagnosis of periodontitis. For such a study, you can use a radiovisiograph (a device for conventional targeted X-rays), or an orthopantomograph (an extraoral device that can take a picture of both jaws at once). However, the most informative method is considered to be extraoral cone-beam computed tomography, which allows layer-by-layer examination of each piece of the jaw and tooth in three-dimensional format.
Currently, the Florida probe computer diagnostic technique has appeared, which allows you to most accurately determine and record the depth of periodontal pockets - the main pathological manifestation of periodontitis. The examination is easily tolerated by patients and helps the doctor prescribe appropriate treatment.
For periodontitis, a microbiological study is also carried out, with which you can study the microflora of the oral cavity and determine the sensitivity of microorganisms to antibiotics for a more accurate selection of drug treatment.
Another mandatory test is a blood test. It allows you to identify the cause of the disease, which may be either the initial stage of diabetes or a chronic infectious process in other organs and systems, as well as disorders associated with hormonal levels and metabolism.
In the process of diagnosing periodontitis, consultation with related specialists is often required to identify and treat concomitant diseases.
Restoration of periodontal tissues with Straumann®Emdogain®
Innovative technology for targeted regeneration of periodontal tissue is used for moderate and severe periodontitis with severe gum recession and destruction of periodontal tissues. Allows you to avoid tooth extraction in almost hopeless cases.
Technology
: Restoration of periodontal tissue is carried out with the drug Straumann®Emdogain® with scientifically proven effectiveness. The gel, saturated with proteins and growth factors, is applied to the cleaned and dry surface of the tooth roots after the open curettage procedure. In case of severe bone resorption, the drug is mixed with bone chips. After this, the gum is sutured.
Advantages of the method
: According to clinical trials, the use of Straumann®Emdogain® in the treatment of moderate and severe periodontitis helps restore the lost volume of gums, connective and bone tissue in the area of the tooth socket.
How is periodontitis treated?
Successful treatment of periodontitis can only be achieved in a well-coordinated team of “doctor plus patient”. Much depends on the doctor, but even more depends on the patient himself. The doctor is responsible for the treatment, and the patient is responsible for maintaining the result, because periodontitis is a chronic disease.
Treatment methods for periodontitis are divided into medicinal and surgical. In case of minor inflammation caused by dental plaque, the doctor thoroughly cleans the teeth, eliminates conditions that contribute to the retention of microbial plaque, polishes the surfaces of the teeth and applies a therapeutic bandage with medication to the inflamed area. If a deep periodontal pocket forms and severe pain occurs, the patient may be prescribed antibiotics. When treating severe periodontitis, it is necessary to resort to more serious (surgical) procedures, such as curettage and flap operations. But in any case, periodontitis requires complex treatment, including professional hygiene, drugs for local and internal use, and, if necessary, surgical procedures.
There is also a hardware method for treating periodontitis - Vector. The method involves using ultrasound in combination with medications aimed at fighting microbes and stimulating healing. The Vector device is used both as an independent technique and in combination with surgical treatment.
Basic orthodontic treatment of patients with periodontal diseases
E. S. Bimbas Doctor of Medicine, Professor, Head of the Department of Pediatric Dentistry and Orthodontics, USMU (Ekaterinburg)
T. V. Zakirov Ph.D., Associate Professor, Department of Pediatric Dentistry and Orthodontics, USMU (Ekaterinburg)
Unfavorable periodontal conditions are quite common in children and adult patients who have problems with the position of teeth and bite. The degree of periodontal damage can range from simple gingivitis to severe periodontitis, which can be localized or generalized. Therefore, in such patients, during orthodontic treatment it is necessary to take into account already manifested periodontal changes [1–3].
All patients with periodontal diseases who consult an orthodontist can be divided into two main groups.
The first group includes people with congenital malocclusions and dentition and already manifested periodontal diseases.
The second category includes patients whose initial indication for orthodontic treatment is pathological changes in the position of the teeth due to periodontopathies [4].
In this article we will consider the first option, in which dental anomalies are primary and directly lead to periodontal damage. It must be taken into account that pathological occlusion cannot function without contributing to its own destruction. Without eliminating the anomalies listed below, a complete correction of periodontal pathology is practically impossible and requires the intervention of an orthodontist: deep traumatic bite; severe crowding of teeth; vestibular displacement of individual teeth (traumatic occlusion).
Let's look at each of these violations in more detail.
A deep traumatic bite is associated mainly with class II anomalies, when the incisal-tubercle contact in the area of the incisors is disrupted and, as a result, their dentoalveolar elongation is observed, the incisal path increases, and overload of periodontal tissue occurs. With class II occlusion anomalies of the 1st subclass, chronic periodontal trauma is observed on the palatal side of the upper incisors, with class II occlusion anomalies of the 2nd subclass - in the cervical region on the vestibular side of the lower incisors, and often on the palatal side. Such an anomaly in the absence of orthodontic treatment leads to severe periodontal destruction: atrophy of the mucous membrane, resorption of bone tissue of the alveolar process and ultimately to tooth loss (Fig. 1, 2).
Rice. 1. Malocclusion due to loss of 4.5, 4.6.
Rice. 2. Chronic periodontal trauma, gum recession.
Severe crowding of teeth. With a pronounced crowded position of the teeth, unfavorable topographic-anatomical relationships are observed: the gums lose their garland-like shape, the interdental papillae hypertrophy (Fig. 3).
Rice. 3. Severe crowding of teeth.
When the teeth are closely positioned, the interradicular bone structure is changed: the septa are thin, linear in shape, poorly vascularized, and poor in spongy substance. Unfavorable structure of the interdental gingiva and interradicular bone is a predisposing factor for the progressive loss of supporting tissues of the teeth.
Traumatic occlusion of individual teeth. When a palatal displacement of one of the maxillary incisors occurs, a traumatic effect on the lower incisors occurs - traumatic occlusion; direct damage to their periodontium is noted due to unfavorable occlusal relationships. With this anomaly, the incisal path is disrupted, the load falls on the lower incisor at an angle to the axis of the tooth, and its vestibular displacement occurs, which increases over time under the influence of occlusal forces. As a result, gum recession develops on the vestibular side of the lower incisor.
Indirect influence of dentoalveolar anomalies on the condition of the periodontium. The first group also includes patients whose periodontal changes are not pathogenetically related to existing dental anomalies: mild and moderate crowding, disocclusion in the area of individual teeth. The reasons for the development of periodontal pathology with these anomalies are: impaired self-cleaning of teeth, stagnation in periodontal tissues, and in some cases, the impossibility of adequate oral hygiene.
Mild to moderate crowding of teeth. If with this anomaly there is no crowding of the roots, then the trophism of the periodontium is not disturbed. There is a violation of self-cleaning of teeth, stagnation. Adequate hygiene in cases of mild crowding can eliminate inflammatory phenomena in the periodontium, even without orthodontic treatment.
Disocclusion of individual teeth. The reasons for the development of periodontitis in the area of disocclusion are the following: impaired self-cleaning of teeth in this area, rapid formation of plaque; In the absence of contact with antagonists, the tooth does not receive chewing load, and stagnation is observed in the periodontal tissues.
Algorithm for complex treatment of patients with dentofacial anomalies and deformities and periodontal diseases:
1. Sanitation of the oral cavity: treatment of hard dental tissues, endodontic treatment, periodontal treatment, surgical sanitation. 2. Orthodontic treatment after the onset of stable remission of periodontal disease:
- creation of parallelism of supporting teeth in patients with dentition defects;
- establishing a favorable crown-to-root ratio;
- restoration of the occlusal line, canine and incisal occlusal paths, elimination of supracontacts, creation of multiple occlusal contacts;
- retraction of the anterior teeth of the upper jaw with a fan-shaped discrepancy with the loss of lateral teeth and supporting tissues.
3. Periodontal surgical interventions. 4. Dental restoration. 5. Implantation. 6. Selective grinding. 7. Splinting and prosthetics.
After developing an overall treatment plan, the first priority is to control all active dental disease. Before any tooth movement, active caries and pulp pathology must be eliminated, and endodontic treatment is carried out as necessary. Orthodontic movement after root canal treatment of teeth follows general principles.
Before completion of orthodontic treatment, crowns, bridges and restorations that require a detailed approach to occlusal contacts should not be made. This is due to the fact that when teeth move, changes in occlusal relationships are inevitable and new dentures may need to be made.
It is necessary to achieve remission of inflammatory periodontal diseases before orthodontic treatment begins, because tooth movement due to periodontal pathology can lead to rapid and irreversible deterioration of the supporting apparatus of the tooth. It may take up to 6 months for the inflammation to subside before tooth movement begins. Scaling and curettage should be undertaken before any tooth movement begins. The decision on the timing of flap operations is made in each case individually. It is better to postpone these interventions until the teeth have been moved. If it is not possible to achieve remission of periodontitis without surgery, then to fill bone defects it is better to use natural-based osteoplastic materials (allogeneic, xenogeneic) with a high osteoconduction index, and orthodontic treatment should be carried out no earlier than 6-12 months after periodontal surgery. It is necessary to avoid the use of preparations based on glass ceramics: this can lead to difficult tooth movement.
Clinical studies have shown that orthodontic treatment of adults with both healthy and damaged periodontal tissues can be completed without loss of attachment if adequate supportive care is provided by the periodontist both initially and during tooth movement [7].
During this preliminary stage, the patient's enthusiasm for treatment and ability to achieve and maintain good overall oral hygiene are carefully tested and are an indicator of motivation. Dental repositioning and restorative efforts in patients who are not adequately trained to maintain good oral hygiene are doomed to fail. On the contrary, if the disease process can be controlled and the patient has demonstrated readiness for the necessary treatment, orthodontic tooth movement can significantly improve periodontal health and reduce the need for surgical treatment (Fig. 4 a - l).
Rice. 4a. Severe chronic periodontitis in a 52-year-old patient. Condition before treatment. Maximum bone resorption in the area 1.2, 1.3.
Rice. 4b. Severe chronic periodontitis in a 52-year-old patient. Condition before treatment. Maximum bone resorption in the area 1.2, 1.3.
Rice. 4c. Severe chronic periodontitis in a 52-year-old patient. Condition before treatment. Maximum bone resorption in the area 1.2, 1.3.
Rice. 4g. Severe chronic periodontitis in a 52-year-old patient. Condition before treatment. Maximum bone resorption in the area 1.2, 1.3.
Rice. 4d. Severe chronic periodontitis in a 52-year-old patient. Condition before treatment. Maximum bone resorption in the area 1.2, 1.3.
Rice. 4e. Severe chronic periodontitis in a 52-year-old patient. Condition before treatment. Maximum bone resorption in the area 1.2, 1.3.
Rice. 4g. Condition after complex treatment. Partial restoration of the bone of the interdental septa in the area 1.2, 1.3. Normalization of aesthetics while maintaining the scalloped gum contour.
Rice. 4z. Condition after complex treatment. Partial restoration of the bone of the interdental septa in the area 1.2, 1.3. Normalization of aesthetics while maintaining the scalloped gum contour.
Rice. 4i. Condition after complex treatment. Partial restoration of the bone of the interdental septa in the area 1.2, 1.3. Normalization of aesthetics while maintaining the scalloped gum contour.
Rice. 4k. Condition after complex treatment. Partial restoration of the bone of the interdental septa in the area 1.2, 1.3. Normalization of aesthetics while maintaining the scalloped gum contour.
Rice. 4l. Condition after complex treatment. Partial restoration of the bone of the interdental septa in the area 1.2, 1.3. Normalization of aesthetics while maintaining the scalloped gum contour.
Rice. 4m. Condition after complex treatment. Partial restoration of the bone of the interdental septa in the area 1.2, 1.3. Normalization of aesthetics while maintaining the scalloped gum contour.
During the entire period of orthodontic treatment, in order to preserve the gum tissue in a healthy state, once every 3 months it is necessary to monitor the condition of the periodontium by a periodontist; if necessary, remove dental deposits and smooth the surface of the roots.
Rice. 4 a - f. An example of complex treatment of a 52-year-old patient. Condition before treatment. In the absence of significant external signs of gum inflammation and a large amount of dental plaque, there are deep periodontal pockets with active exudation and suppuration. Radiologically, pronounced resorption of bone tissue of the alveolar processes is noted, reaching a maximum in the area of 1.2, 1.3 teeth.
Rice. 4 f - m. Condition after complex treatment. Although orthodontic treatment does not eliminate the possibility of further progression of periodontitis, it can significantly improve the condition of the periodontal supporting tissues. Alignment of teeth and improvement of the occlusal relationship had a positive effect on the level of supporting tissues and the morphology of the alveolar process. The following periodontal effects have been achieved: interdental craters are flattened; the course of the circular ligament of the tooth has improved; bifurcation defects were reduced. Partial restoration of the bone tissue of the interdental septa in the area of 1.2, 1.3 teeth, together with a significant reduction of periodontal pockets, made it possible to avoid surgical intervention with flap folding and achieve an optimal result while maintaining the scalloped gum contour. The patient was pleased with the changes in the aesthetics of her teeth and face.
There are several periodontal surgery procedures that may be necessary before starting orthodontic treatment. Such manipulations include:
1. Increasing the width of the attached gum: a) Plastic surgery with a free gum flap. If the patient has insufficient thickness and/or width of the attached gum (usually in the anterior part of the lower jaw), plastic surgery with a free gum flap is required before starting orthodontic treatment. If the transplantation is not performed before the start of orthodontic treatment, then during the process there is a high risk of gum atrophy. Free gum grafting is an effective way to increase the area of attached gum and reduce the likelihood of recession. If a new support is built through controlled tissue regeneration, then new intact desmodontal fibers are created to transfer orthodontic force. The period of time between the end of periodontal therapy and orthodontic treatment ranges from 6 to 8 weeks. The disadvantages of palatal flap transplantation are the traumatic nature of the intervention, a long postoperative period, additional wound surface in the oral cavity and the “patch effect”, which can reduce the aesthetics of the gums in the anterior region. b) Plastic surgery of the oral vestibule. In case of a small vestibule or in the presence of mucosal strands that cause gum recession, plastic surgery of the oral vestibule is indicated, which is often performed in the lower jaw in the anterior region (Fig. 5, 6).
Rice. 5. Small vestibule in the frontal region of the lower jaw.
Rice. 6. View 1 week after vestibuloplasty.
2. Plastic surgery of the upper lip frenulum Plastic surgery can be recommended for a patient with diastema if the upper lip frenulum is a thick connective tissue cord that causes tissue ischemia when the upper lip is pulled. There are 4 types of attachment of the frenulum: to the mucosa, to the gingiva, to the papilla and penetrating the papilla. Indications for plastic surgery are the presence of gum recession with loss of the interdental papilla in the third type and the presence of diastema in the second type. For a more accurate diagnosis, targeted radiography is necessary to identify the weaving of the frenulum into the palatal suture. In this case, a strip of clearing between the central incisors will be visible on the radiograph [6]. Plastic surgery is performed in the presence of recession, regardless of orthodontic treatment, in the presence of a diastema after its closure by orthodontic means (Fig. 7, 8).
Rice. 7. Abnormal attachment of the frenulum of the upper lip.
Rice. 8. View immediately after frenuloplasty.
In this case, the postoperative scar will serve to retain the achieved results. 3. Closure of gum recession. When gum recession occurs in the area of the roots of individual teeth, a free connective tissue flap from the palate is used. The success of this procedure is due to the dual supply of blood from the underlying periosteum and the underlying gingival flap. The technique is predictable and has a positive aesthetic result. Recently, this procedure is most often performed after moving the tooth into place, but sometimes it is required before active orthodontic treatment. The prognosis for gum recovery after plastic surgery for recession depends on the degree of impairment (Fig. 9-12).
Rice. 9. Type of recession in area 2.3 before treatment.
Rice. 10. Immediately after recession plastic surgery.
Rice. 11. View after 2 weeks.
Rice. 12. In 3 months. To prevent relapse, orthodontic treatment is necessary.
Complete orthodontic treatment for periodontal diseases
Patients of the 1st group, in whom PCA directly or indirectly affect the condition of the periodontium, require complete orthodontic treatment and restructuring of the occlusion. Treatment in these cases requires a fixed appliance on both jaws and long-term movement of the teeth.
It must be remembered that orthodontic treatment, especially if it is not carried out competently, can cause complications, including periodontal complications. These include deterioration of oral hygiene (the orthodontic fixed appliance is a retention site for plaque), the development of caries and gingivitis, resorption of the apexes of the roots of the teeth, gum recession when teeth move to the occlusal or vestibular side. Periodontal changes may also develop on the mesial side and in the area of bifurcations of the mandibular molars as a result of their vertical movement, exacerbation of periodontitis, and hypertrophy of the gingival papillae.
Clinical and histological studies show that tooth movement is influenced by the width of the alveolar process and the structure of the gums. The main condition for the consistent transformation of alveolar bone is the balance between bone resorption and periosteal bone apposition in accordance with the direction of pressure.
In adult patients, if the periosteal remodeling response is slow (eg, with edentulous alveolar bone and thin surrounding mucosa), vertical and horizontal resorption may occur during tooth movement.
To prevent such a complication, prophylactic mucosal graft transplantation is indicated.
Orthodontic movement of teeth with periodontal damage is associated with certain difficulties and is somewhat different from conventional orthodontic treatment:
- The movement of teeth is limited (treatment with extraction is undesirable), since in a weakened periodontium, the movement of teeth over long distances causes a deterioration in its condition.
- Pre-orthodontic filling of bone pockets with hydroxylapatite ceramics should be abandoned, since experimental studies show that teeth do not move in the bone area filled with ceramics [4].
- When the periodontium is weakened, a reduction in the amount of force used is required, since this force is distributed over a smaller root surface. The amount of force used should decrease in proportion to the loss of bone tissue.
- A change in the biomechanics of tooth movement (system of forces) is required by shifting the resistant center of the tooth closer to the apex. Braces must be fixed higher, according to the degree of exposure of the roots.
- Splinting after orthodontic treatment for an indefinite period is mandatory (non-removable permanent splint made of multi-strand wire).
- In case of severe periodontitis and severe destruction of bone tissue (more than 1/2 the length of the root), it is necessary to immediately fix the teeth with a submersible splint.
- Selective grinding is mandatory after completion of orthodontic treatment.
Correction of deep incisal occlusion. In case of exacerbation of inflammatory periodontal diseases and the patient has an occlusal injury, emergency care includes the manufacture of a bite block. Periodontal trauma is immediately eliminated, and in combination with anti-inflammatory therapy, remission of the disease occurs faster.
After periodontal treatment, correction of deep incisal occlusion is carried out using fixed orthodontic equipment.
The best shown is the straight arc technique using weak forces (Damon system). As a result of treatment, the occlusal line is normalized, the height of the bite is restored, the incisal and lateral paths of occlusion are separated, the range of motion in the joints increases, support for the lips is created, and conditions for prosthetics are improved. If, with a deep bite, there are defects in the dentition of the lower jaw, their opening and subsequent replacement with prosthetic structures is indicated.
In case of deep incisal occlusion, intrusion of the anterior teeth should not be carried out: immersion of infected tissues is possible. In addition, the use of intrusive mechanics emphasizes the shortening of the lower third of the face in deep bites. Elimination of severe crowding of teeth restores favorable anatomical and topographic relationships: creates wide bone partitions rich in spongy substance, a favorable shape of interdental papillae, and improves blood supply (Fig. 13, 14).
Rice. 13. Condition before treatment of severe crowding of teeth.
Rice. 14. Result of correction with removal of the dystopic incisor.
Along with improving periodontal resistance, eliminating crowded teeth creates conditions for maintaining adequate oral hygiene and also facilitates the removal of deposits and root treatment.
More favorable conditions are created for bone tissue regeneration.
Correction of traumatic occlusion in childhood can be carried out using a removable device, for example, a plate that separates the bite from ejectors for abnormally positioned teeth [5]. After orthodontic treatment in children, the periodontium is completely restored, so eliminating anomalies in childhood is the prevention of periodontal diseases (Fig. 15, 16).
Rice. 15. Reverse incisal overlap, traumatic occlusion.
Rice. 16. Normalization of the position of the incisors, healthy periodontium.
Periodontal restoration in adults is also noticeable, but occurs more slowly and depends on the degree of destruction of supporting tissues (Fig. 17-19).
Rice. 17. Reducing recession during orthodontic treatment.
Rice. 18. Traumatic occlusion with the development of gum recession.
Rice. 19. Reduction of recession after normalization of teeth position.
In conclusion, it can be noted that only an integrated approach and the participation of a group of specialists (periodontist, orthodontist, orthopedic dentist) in providing the necessary dental care to patients with inflammatory periodontal diseases allows, in most cases, to achieve success in treatment and ensure a stable long-term result.
The list of references is in the editorial office
What are the surgical treatments for periodontitis?
Surgical treatment of periodontitis is important in the later stages of the disease with severe tooth mobility and deep periodontal pockets. This is, first of all, a curettage procedure, which involves removing dental plaque and pathological granulation tissue from under the gums. If the depth of the periodontal pocket is up to 4 mm, closed curettage is performed without opening the gum; if it is more, open or flap surgery is performed, when it is necessary to detach the periosteal flap, fold it back and clean out the pocket. This procedure is always performed with pain relief and is well tolerated by patients.
In addition to the procedures described above, splinting is performed for periodontitis, which secures loose teeth.
Open curettage of periodontal pockets
This type of operation does not have the disadvantages of the previous method. A good overview of the problem area allows the doctor to remove all granulation tissue and thereby prevent further progression of the disease. Open curettage is performed under local anesthesia and takes place in several stages:
- The surgeon makes an incision in the gum in the projection of the neck of the tooth.
- A certain area of the mucous membrane peels off.
- Granulations and deposits in periodontal pockets are eliminated.
- If necessary, plastic surgery of bone defects is performed.
- The flap is sutured, the surgical field is treated and protected with an aseptic dressing.
Due to the high traumatic nature of soft tissues, a limited area of gum can be treated in one operation, usually up to 8 teeth. After the wound has healed, repeated interventions are performed.
Is it possible to eliminate periodontitis with a laser?
Laser treatment of periodontitis is one of the most effective and minimally invasive ways to combat the disease, which is one of the stages of complex treatment. The laser has cleansing and antibacterial properties. During the procedure, each periodontal pocket is treated for a certain time, sufficient for the laser light beam to destroy pathogenic bacteria. The procedure is bloodless and virtually painless. However, a good effect can only be obtained with an integrated approach to the treatment of periodontitis.
Is it true that periodontitis can be cured with implantation?
Implantation is a method of combating not periodontitis itself, but its consequences. At a later stage of the disease, teeth become loose and fall out, so they have to be replaced with implants. It should be understood that dental implantation for periodontitis has its own difficulties and limitations, since bone tissue is absorbed in this disease. Its sufficient volume is the main condition for successful installation of implants. If periodontitis is in an advanced stage, implantation can be very difficult or even impossible due to a lack of bone volume. That is why patients should begin treatment as early as possible in order to do everything possible to preserve their teeth, and if they are lost, do not miss the opportunity to restore them with implants.
In any case, before installing implants, it is necessary to transfer periodontitis to the stage of remission (stabilization) or, if possible, eliminate the cause of its occurrence.
What consequences can untreated periodontitis lead to?
Loss of teeth
The advanced stage of the disease destroys the soft and hard tissues around the teeth, which leads to their loss.
Deterioration of conditions for implantation
As mentioned earlier, with severe periodontitis, the volume of the jaw bone is significantly reduced, which makes it difficult to install implants, requiring preliminary bone growth, and in extremely severe cases makes implantation impossible.
The occurrence of other diseases
Periodontitis contributes to diseases of the gastrointestinal tract, diseases of the lungs, heart and even the formation of blood clots.
Alveolar ridge bone augmentation and implantation
Bone grafting is used to restore bone volume in severe forms of periodontitis. The operation is performed after the inflammation has been relieved and the source of infection has been eliminated. Building up allows you to restore the bone layer around the root and strengthen the tooth. The procedure is also indicated after the removal of hopeless teeth to prepare the jaw for dental implantation.
To restore bone tissue volumes, our clinic uses premium materials Bio-Oss® (Germany) with high survival rates.
How to avoid further exacerbation of the disease?
This is where the patient becomes the main member of a well-coordinated doctor-patient team. To maintain the results obtained after treatment of periodontitis, you should brush your teeth correctly and regularly, following all the recommendations of the treating dentist, since with periodontitis, individual oral hygiene differs from usual. In particular, along with a regular brush and paste, there is a need to connect additional hygiene products: dental floss, various brushes for teeth, an irrigator, etc.
In addition, it is necessary to come to the dentist for professional cleaning at least once every six months, and for people with chronic periodontitis even more often - once every three months. Good hygiene is an excellent prevention of periodontitis and the only way to maintain the results of treatment.
Professional oral hygiene
Plaque and tartar are the main source of infection in the mouth and the main cause of inflammation of periodontal tissue. To get rid of dental plaque, professional cleaning is used - a mandatory component of the treatment of all forms and stages of periodontitis.
The procedure includes the following steps:
- Removing tartar using an ultrasonic scaler;
- Carrying out the Air-flow procedure (removing supragingival deposits with an air-abrasive mixture);
- Polishing the surface of teeth with fluoride-containing paste.
The procedure is carried out 2 times a year
How much does it cost to cure periodontitis? What does the cost consist of?
The price for periodontitis treatment depends on the complexity of the disease, whether surgical procedures will be performed and to what extent.
Important!
Folk remedies in the form of all kinds of herbal infusions do not help with periodontitis. They can bring temporary relief and mask the problem, but mouth rinses cannot radically solve it. Neither home treatment nor the miraculous toothpaste from TV commercials will help get rid of periodontitis. Rinses and toothpastes are just one of the auxiliary components in complex treatment. If you have periodontitis or suspect it, contact the dentist for timely diagnosis, since it is in the early stages of the disease that doctors have a lot of opportunities to help you!