According to WHO, 98% of the world's population suffers from periodontal disease. That is, almost all of us with very rare exceptions. This prevalence is due to the fact that these pathologies remain undetected for a long time; pronounced symptoms appear in the later stages. This can be explained by features of anatomy.
TOOTH PULP
There is a cavity inside the tooth that resembles the shape of a crown, and at the root of the tooth it continues in the form of a canal. The root canal ends at the apex of the tooth root with an opening. The tooth cavity is filled with loose connective tissue, rich in blood vessels and nerves - pulp. The dental pulp is divided into crown and root parts. The pulp of the tooth crown is represented by loose connective tissue with a delicate network of collagen and precollagen fibers with a large number of cellular elements. In the tooth root pulp, collagen structures are denser, thicker and oriented longitudinally along the neurovascular bundle.
Based on the cellular composition of the pulp, they are divided into: peripheral, subodontoblastic and central layers.
The peripheral layer consists of specialized cells - odontoblasts, which take part in the metabolic processes of enamel and dentin. They are located in several rows.
The odontolast has an elongated pear-shaped shape. It has a peripheral protoplasmic process (or dentine), which runs in the dentinal tubule to the dentinoenamel junction, and short lateral processes that anastomose with neighboring cells in the early stages of differentiation.
The subodontoblastic and central layers consist of small, poorly differentiated stellate cells connected to each other by short processes. The pulp contains many fibroblasts that participate in the formation of a fibrous capsule that limits the focus of inflammation.
In the central layers there are cytoplasmic cells - histiocytes. During inflammation, they acquire the ability to move and phagocytose and are called macrophages.
The blood supply to the pulp is provided by blood vessels that penetrate into it through the opening of the apex of the tooth root and through additional canals from the periodontium. The lymphatic system in the pulp is presented in the form of slits, capillaries, and vessels. The outflow of lymph from the pulp occurs in the submandibular and mental lymph nodes. Arterial trunks accompany veins. The pulp vessels have numerous anastomoses. Through the apical foramen, sensitive pulpy and non-pulse fibers of the trigeminal nerve pass, which innervate the pulp, forming plexuses.
The dental pulp has a trophic, protective and plastic function. The trophic function is carried out due to the developed network of blood and lymphatic vessels; protective - due to histiocytes, plasma cells; plastic is the participation of the pulp in the formation of dentin.
The bulk of the tooth is dentin, which surrounds the tooth cavity. In the area of the tooth crown, dentin is covered with bright white enamel. The dentin of the root is covered with cement.
Gum structure
Gums are the mucous membrane that covers the alveolar processes of the jaws and covers the necks of the teeth. Normally, the mucous membrane of the gums is pale pink in color, its surface is uneven, similar to an orange peel due to small retractions that are formed at the site of attachment of the gums to the alveolar bone by bundles of collagen fibers. With inflammatory edema, the irregularities of the gum mucosa disappear, the gums become even, smooth, and shiny.
Gum zones:
- marginal gingiva, or free edge of the gum;
- alveolar gingiva, or attached gum;
- sulcular gum, or gingival groove;
- transitional fold.
Marginal gum is the gum surrounding the tooth, 0.5-1.5 mm wide. Includes the interdental or gingival papilla - papillary gum.
Alveolar gum is the gum covering the alveolar process of the jaws, 1-9 mm wide.
Sulcular gum (gingival groove) is a wedge-shaped space between the surface of the tooth and the marginal gum, 0.5-0.7 mm deep.
The gingival sulcus is lined with sulcular epithelium, which is attached to the enamel cuticle. The place where the epithelium attaches to the enamel is called the gingival attachment. The gingival attachment is considered as a functional unit consisting of 2 parts:
• The epithelial attachment , or junctional epithelium, which forms the floor of the gingival sulcus, lies above the enamel-cementum junction on the enamel. The width of the epithelial attachment ranges from 0.71 to 1.35 mm (average 1 mm);
• connective tissue fibrous attachment , which is located at the level of the enamel-cementum junction on the cement. The width of the connective tissue attachment ranges from 1.0 to 1.7 mm (average 1 mm).
For the physiological attachment of the gum to the tooth and for the healthy state of the periodontium, the gingival attachment must be at least 2 mm in width. This size is defined as the biological width of the gum.
The depth of the anatomical gingival groove is less than 0.5 mm, determined only histologically.
A clinical gingival sulcus with a depth of 1-2 mm is determined by probing.
The epithelial attachment is weak and can be destroyed by probing or other instruments. For this reason, the clinical depth of the gingival sulcus is greater than the anatomical depth. Disruption of the connection between the attachment epithelium and the enamel cuticle indicates the beginning of the formation of a periodontal pocket.
Histological structure of the gums.
Histologically, the gum consists of 2 layers:
• stratified squamous epithelium,
• lamina propria (lamina propria).
There is no submucosal layer.
The structure of stratified squamous epithelium of the oral cavity:
• basal layer - consists of cylindrical cells located on the basement membrane;
• stratum spinosum - consists of polygonal cells that are connected to each other by hemidesmosomes;
• granular layer - the cells are flat, contain grains of keratohyalin;
• stratum corneum - the cells are flat, without nuclei, keratinized, and constantly slough off.
The stratum basale lies on the basement membrane , which separates the epithelium from the lamina propria of the gingival mucosa.
In the cytoplasm of cells of all layers of the epithelium, except for the stratum corneum, there is a large number of tonofilaments . They determine gum turgor, which resists mechanical stress on the mucous membrane and determines its extensibility. The epithelium of the marginal gum is keratinized, which makes it more resistant to mechanical, temperature and chemical influences during food intake.
Between the cells of multilayered squamous epithelium there is an adhesive basic substance of connective tissue (matrix), which contains glycosaminoglycans (including hyaluronic acid). Hyaluronidase (microbial and tissue) causes depolymerization of glycosaminoglycans of the main substance of connective tissue, destroying the bond of hyaluronic acid with protein, as a result of which the hyaluronic acid molecule changes its spatial configuration, pores are formed and the permeability of connective tissue for various substances increases, including microbes and their toxins.
Histological structure of the attachment epithelium.
The attachment epithelium consists of several (15-20) rows of elongated cells located parallel to the surface of the tooth.
There are no blood vessels or nerve endings in the epithelium of the gum mucosa.
Histological structure of the lamina propria of the gingival mucosa.
The lamina propria is a connective tissue formation that consists of two layers:
• superficial (papillary),
• deep (mesh).
The papillary layer is formed by loose connective tissue, the papillae of which protrude into the epithelium. The papillae contain blood vessels and nerves and contain nerve endings.
The mesh layer is formed by denser connective tissue (contains more fibers).
Connective tissue composition:
• the main substance is the intercellular matrix (35%), formed by macromolecules of proteoglycans and glycoproteins. The main glycoprotein is fibronectin, which ensures the connection of the protein to the cell matrix. Another type of glycoprotein, laminin, ensures the attachment of epithelial cells to the basement membrane.
• fibers (collagen, argyrophilic) - 60-65%. The fibers are synthesized by fibroblasts.
• cells (5%) - fibroblasts, polymorphonuclear leukocytes, lymphocytes, macrophages, plasma, mast and epithelial cells.
Blood supply to the gum mucosa.
The gum is supplied with blood from the subperiosteal vessels, which are the terminal branches of the sublingual, mental, facial, greater palatine, infraorbital and posterior superior dental arteries. There are many anastomoses through the periosteum with the vessels of the alveolar bone and periodontium.
The microvasculature of the gums is represented by: arteries, arterioles, precapillaries, capillaries, postcapillaries, venules, veins, arteriovenular anastomoses.
Features of the capillaries of the gum mucosa.
The capillaries of the gum mucosa are characterized by:
• the presence of a continuous basement membrane, the presence of fibrils in endothelial cells,
• lack of fenestration of endothelial cells. (All this indicates a large volume of exchange between blood and tissues)
• the diameter of the capillaries is 7 microns, that is, the capillaries of the gums are true capillaries.
• in the marginal gum, capillaries have the form of capillary loops (“hairpins”), located in regular rows.
• in the alveolar gum and transitional fold there are arterioles, arteries, venules, veins, arteriovenular anastomoses.
Blood flow in the gum vessels is carried out due to the difference in intravascular pressure. From the arterial capillaries (where the pressure is 35 mm Hg) water, oxygen and nutrients are filtered into the tissues (where the pressure is 30 mm Hg), and from the tissues water, carbon dioxide and metabolites are filtered into the venules ( where the pressure is only 2 0 mm Hg t. s t.)
• The intensity of blood flow in the gums is 70% of the intensity of blood flow of all periodontal tissues.
The partial pressure of oxygen in the gum capillaries is 35-42 mmHg.
In the mucous membrane of the gums there are also non-functioning capillaries that contain only blood plasma and do not contain red blood cells. These are the so-called plasmatic capillaries.
Features of blood flow in the area of the periodontal sulcus.
In the area of the periodontal sulcus, the vessels do not form capillary loops, but are arranged in a flat layer. These are postcapillary venules, the walls of which have increased permeability, through which blood plasma is transudated and converted into gingival fluid. Gingival fluid contains substances that provide local immune protection of the oral mucosa.
Local immunity of the oral cavity is a complex multicomponent system, including specific and nonspecific components, humoral and cellular factors that provide protection to oral and periodontal tissues from microbial aggression.
Humoral factors of local immunity of the oral cavity:
• lysozyme - causes depolymerization of polysaccharides of the cell membrane of microorganisms;
• lactoperoxidase - forms aldehydes, which have a bactericidal effect;
• lactoferrin competes with bacteria for iron, exerting a bacteriostatic effect;
• mucin - promotes the adhesion of bacteria to epithelial cells;
• beta-lysines - act on the cytoplasm of microorganisms, promoting their autolysis;
• immunoglobulins (A, M, , G) - enter from the blood serum by passive diffusion through the intercellular spaces of the gingival sulcus and through epithelial cells. The main role is played by immunoglobulin A (Ig A). The secretory component 5C of immunoglobulin A is synthesized by the epithelial cells of the excretory ducts of the salivary glands. Immunoglobulin A combines with the secretory component in the oral fluid and is fixed on epithelial cells, becoming their receptor, giving the epithelial cell immunospecificity. Immunoglobulin A binds to the bacterial cell, preventing bacteria from settling on the surface of the teeth, and reduces the rate of plaque formation.
Cellular factors of local immunity of the oral cavity:
• polymorphonuclear leukocytes - released as part of the gingival fluid from the gingival sulcus in an inactive state. Neutrophil leukocytes have special Fc and C3 receptors for connecting with the bacterial cell. Leukocytes are activated in conjunction with antibodies, complement, lactoferrin, lysozyme, peroxidase.
• monocytes (macrophages) - phagocytose oral microorganisms and secrete substances that stimulate leukocytes.
• epithelial cells of the gum mucosa - have special receptors for connecting with microbial cells.
• salivary mucin promotes the adhesion of microbial cells and fungi to the surface of the epithelial cell.
Constant exfoliation of epithelial cells with microorganisms blocked on them helps remove microbes from the body and prevents them from entering the gingival sulcus and deeper into periodontal tissue.
Innervation of the gingival mucosa.
The nerve fibers of the gum (myelinated and unmyelinated) are located in the connective tissue of the gingival lamina propria.
Nerve endings:
• free - interoreceptors (tissue),
• encapsulated (glomeruli), which with age turn into small loops. These are sensitive receptors (pain, temperature) - the so-called polymodal receptors (which react to 2 types of stimuli). These receptors have a low threshold of irritation, which goes to the weakly adapting neurons of the nuclei of the V pair (trigeminal nerve). Sensory receptors react to pre-painful stimuli. The largest number of these receptors is located in the marginal zone of the gums.
PERIODONTIUM
The root of the tooth is held in the socket by connective tissue fibers that make up the root membrane or periodontium.
The periodontium is located in a narrow, slit-like space between the tooth root and the jaw bone. The thickness of the periodontium is 0.15-0.25 mm. With age, as well as from mechanical load, the thickness of the periodontium changes and amounts to 1.2-1.2 mm.
The basis of periodontal connective tissue are bundles of interdental and cemento-alveolar fibers, which are woven, on the one hand, into the compact plate of the alveoli, and on the other hand, into the cementum of the tooth root. In the area of the tooth neck, fibrous fibers have an almost horizontal direction and include numerous collagen fibers, circularly covering the cervical area (circular ligament). The apical periodontium contains more loose connective tissue and cellular elements. Fibrous fibers in the area of the tooth apex are represented by looser, more delicate bundles and are arranged radially; with the help of the fibers, the tooth is suspended and fixed in the bone bed.
The blood supply to the periodontium is abundant and it has a fairly developed lymphatic network. Periodontal vessels form several plexuses (external, middle, capillary) in the root area. Cellular elements are represented by fibroblasts, mast cells, plasma cells, histiocytes, cementoblasts, osteoblasts, and epithelial remnants of the neoplastic epithelium. The main function of the periodontium is support and retention. In addition, the periodontium distributes and regulates pressure on the tooth (shock absorbing), has a plastic function due to cellular elements and a barrier function (due to the unique anatomical structure and resistance to adverse environmental influences). The reflexogenic function of periodontium is also highlighted.
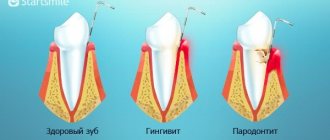
Gingival sulcus
Liquid is concentrated in the gingival groove, the chemical composition of which contains enzymes and microelements. The main task of this liquid is a barrier, that is, it does not allow aggressive agents to pass through and resists the factors of periodontal disease. Simply put, it destroys pathogens, neutralizes their toxins, etc. However, when it is destroyed, for example, due to the formation of subgingival stone, disruption of trophic processes, the physiological periodontal pocket turns into a pathological one. The collagen fibers that connect the tooth root and periodontal tissue are destroyed. Tooth mobility of varying degrees appears, gum recession (decay) occurs, and degenerative processes in the bones are detected.
Bone tissue and periosteum
The alveolar process of the jaw is formed by bone tissue, which consists of 60-70% minerals and water, the rest is organic substances, which are mainly represented by collagen.
On the x-ray, a clear strip is visible along the edge of the alveolus of the tooth, and behind it there is spongy bone - which has a looped, cavernous structure. It is these factors that are paid attention to when diagnosing and treating periodontal diseases. A decrease in the thickness of the cortical plate, a decrease in the height of the alveoli and a thinning of the clarity of the pattern, smoothing out its cavernous pattern are symptoms and at the same time the causes of gum loss, the appearance of tooth mobility and the formation of pathological periodontal pockets.
Blood, nerve and lymphatic vessels
Periodontal tissues, and the entire maxillofacial area, have a dense network of blood vessels. Nutrition is provided by the external carotid artery and veins. The arteries give branches to each alveolus, and passing through the periosteum, they nourish the gums and periodontium. The periodontal tissue is innervated by branches of the trigeminal nerve. In the depths of the alveoli of the jaw, this large branch is divided into parts: one of them goes to the pulp of the tooth, the other to the periodontium. These nerve fibers are involved in the control of chewing pressure and the perception of information about disease and pain. The accumulation of lymphatic vessels covering the root of the tooth provides the shock-absorbing function of the periodontium, but collagen fibers are involved in this process. It is the lymphatic vessels that play a huge role in the regulation of inflammation: they ensure the removal of inflammatory fluid from the lesion.
Periodontal diseases: general concepts and classification
The periodontium can be conditionally called a separate organ of the oral cavity, which has only an indirect relationship to the teeth due to its close relationship.
Today, periodontal diseases are one of the most common diseases among patients all over the world. But, despite this, there are still disputes in the classification, diagnosis (especially early) and methods of treatment of periodontal disease. Recent studies prove the close connection between periodontal diseases and the condition of internal organs. A connection has been established between periodontal pathologies and diseases of the kidneys, genitourinary system in women (up to premature birth) and men (prostatitis and erectile dysfunction), between heart disease and even vascular disasters: heart attacks and strokes and periodontal condition. Therefore, the only way to prevent all these consequences is to promptly treat periodontal diseases, and best of all, take comprehensive measures to prevent periodontal diseases. Text: Yulia Lapushkina.
DENTINE
Dentin in its structure resembles coarse-fibrous bone tissue, consisting of a basic substance penetrated by a large number of dentinal tubules. The main substance of dentin consists of collagen fibers, between which there is an amorphous adhesive substance. The outer layer of dentin (with a radial arrangement of fibers) is called mantle; the inner layer with a tangential arrangement of fibers is peripulpar. Dentinal tubules (tubules) have the shape of round, oval tubes. They begin in the tooth cavity, bending in a wave-like manner, pass through the thickness of the dentin and end in flask-shaped swellings in the area of the dentino-enamel junction.
In the lumen of these tubules there are dentinal processes of odontoblasts. Dentin contains 70-72% inorganic substances (mainly phosphate and calcium carbonate), and 28-30% is water and organic matter (proteins, fats and carbohydrates).
Tooth enamel Tooth enamel is the hardest tissue of the human body. In the area of the cusps of the tooth crown there is the thickest layer of enamel; towards the cervical area the thickness of the enamel decreases. Enamel prisms are the main structural formation of enamel. The enamel prism is a faceted cylindrical fiber that begins at the dentinoenamel junction.
It bends in an S-shape, runs radially and ends on the surface of the tooth crown. Enamel prisms are connected into bundles (10-20 each), directed radially from the dentinoenamel junction to the outer surface. The thickness of the prisms is from 3 to 6 microns. Each prism contains thin cytoplasmic fibers that form an organic mesh, in the loops of which crystals of mineral salts are located.
Enamel prisms and interprismatic spaces (in electron microscopic examination) consist of strictly oriented hydroxyapatite crystals arranged in a certain order, the length of which ranges from 50 to 100 nm.
Most of the tooth enamel consists of inorganic matter (95%), organic (1.2%) and water (3.8%). Tooth enamel contains 96.5% mineral salts, of which about 54% are phosphorus and calcium (17% and 37%, respectively), which are represented by hydroxyapatite crystals.
TOOTH CEMENT
The cementum of the tooth covers the root and is divided into primary and secondary. Primary (cell-free) cement is adjacent directly to dentin, covering the lateral surfaces of the tooth root. Secondary (cellular) contains cementocides, covers a layer of primary cement, is localized only in the area of the root apex and on the interroot surfaces of premolars and molars.
The main substance of cement is represented by collagen fibers running in different directions, most of which run in the radial direction. In some pathological conditions, hypercementosis is observed (excessive deposition of layers of cement on the surface of the tooth root). Cement consists of 68% inorganic and 32% organic substances.