According to international statistics, one of the most common diseases among the population is caries. Caries affects the teeth of about 95% of the population. Caries, according to the international classification, depending on its location/limitation, can be within the enamel, within the dentin, or within the cement. This article will focus specifically on dentine caries, since patients often complain about existing dentine caries (the previous stages do not cause much pain, there may be discomfort and aesthetic dissatisfaction), as well as on the diagnosis and treatment of dentine caries.
First, let's get acquainted with the position of dentin caries in generally accepted classifications.
Tooth structure and types of carious lesions
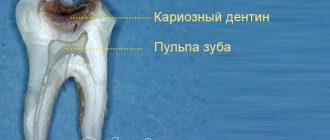
A tooth consists of several parts. On top it is covered with hard mineralized enamel, underneath there is dentin, and even deeper - the root of the tooth and pulp. Caries is a pathological process that is accompanied by demineralization and softening of hard dental tissues with the subsequent formation of a carious cavity. The process can affect any part of the tooth; depending on this, caries of enamel, dentin or cement is distinguished.
Carious lesions of the enamel are characterized by symptoms such as softening, the appearance of a white or brown spot, roughness, and sometimes the carious cavity is located in the enamel. If the lesion affects the bone tissue of the tooth, which makes up its bulk, in this case we speak of dentin caries. This form of lesion is characterized by the formation of a carious cavity directly in the dentin.
Cement caries affects the root of the tooth and contributes to its exposure. It often occurs with gum disease, when there is no close contact between the tooth and the gum.
Causes of average caries
The main factors for the development of secondary caries in dentistry include:
- the presence of cariogenic microorganisms in the oral cavity;
- following a diet high in carbohydrates;
- reducing the resistance of hard dental tissues to adverse conditions.
In addition to these main factors, there are also reasons predisposing to the appearance of average caries, which most often accelerate its development, namely:
- non-compliance with oral hygiene rules;
- the presence of dental anomalies (crowding, malocclusion, violation of the timing of teething and replacement of teeth);
- bleeding gums;
- presence of somatic diseases;
- violation of the diet, which involves eating carbohydrates (sucrose, glucose, fructose);
- a decrease in the degree of resistance of dental tissues to caries with a weakening of general immunity;
- changes in the mineral composition of saliva;
- disruption of the biochemical structure of tooth tissue;
- predisposition to dental diseases at the genetic level.
In addition, the cause of the development of average caries may be a low protein content (lysozyme), which inhibits the growth of microorganisms, as well as low mineralization of the enamel. Medium caries develops with the progression of superficial caries in the process of dentin destruction. The waste products of microorganisms penetrate deep into the tubules, causing demineralization and direct softening of dentin.
Dental caries and its features
Dentin is a hard bone tissue that is located between the tooth enamel and the root and forms the basis of the tooth. Although dentin is a hard substance, it has a loose structure, contains many organic components and, without reliable protection of tooth enamel, is easily destroyed by the acid produced by bacteria. If the carious process has already affected the dentin, the disease will develop faster than with enamel caries.
The following signs are characteristic of dentin caries:
- the formation of a carious cavity (if there may be no cavity when the enamel is damaged, then with dentine caries there is always a hole in the tooth);
- toothache (as a rule, carious damage to the bone tissue of the tooth is accompanied by pain - first as a reaction to hot, cold, sour, sweet, and with deeper damage - as independent pain);
- bad breath (it occurs as a result of decay processes occurring in the carious cavity);
- discomfort when chewing (occurs if a carious cavity is located on the chewing or contact surface of the teeth);
- difficulties when using dental floss (when cleaning between teeth, the floss gets stuck, breaks or is damaged);
- change in tooth color (takes on a yellowish or brownish tint).
Any of these symptoms, and especially a combination of signs, most likely indicates damage to dentin by caries and requires contacting a dentist.
What is caries?
Medical statistics are unpleasantly surprising: according to the World Health Organization, the incidence of dental caries in the world exceeds 95%. This indicator allows us to assign this pathology the status of the most common. Its name comes from the Latin “caries”, which translates as “rotting”. It is a complex destructive process that occurs in hard dental tissues due to the complex influence of a number of external and internal factors and, if left untreated, can lead to tooth loss.
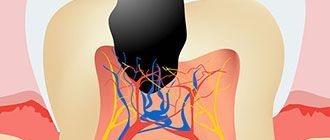
At an early stage of development, carious processes lead to the loss of salts and minerals by tooth enamel (demineralization) and the destruction of its organic matrix. Next, dentin begins to collapse, in which a cavity is formed filled with pathological contents. If you do not start treating acute dental caries at this stage, the periodontal tissue and pulp will become inflamed with all the ensuing consequences. In order to stop the process at this stage, you will have to remove the pulp.
How does a tooth hurt with dentin caries?
Different types of pain are characteristic of different stages of caries. When dentin is damaged, the stages of medium and deep caries are distinguished. In the first case, the carious cavity is located closer to the enamel; in the deep stage, it is as close as possible to the area of the dental nerves.
The middle stage of dentin caries is characterized by a painful reaction in response to temperature or taste stimuli, the pain quickly passes, and the intervals without pain are quite long.
If caries is in the stage of deep damage to dentin, it is characterized by intense long-term pain with short intervals without pain.
Deep caries is the most dangerous, because at any moment it can be complicated by pulpitis, periodontitis, purulent inflammation, and the spread of infection beyond the dental tissues. But even the moderate one can turn into the deep stage at any moment, so if you have a toothache of any nature, you should consult a dentist as soon as possible.
Classification of caries
The disease is classified according to a number of signs, which can be found in our table below:
| Type/form of caries | Distinctive features |
| According to the severity of the ongoing processes: | |
| Chronic caries (compensated form) | The pathological process proceeds sluggishly and slowly, carious cavities are lined with replacement pigmented dentin. Depending on the severity of the process, superficial, medium and deep chronic caries are distinguished. The first is manifested cosmetically - by a change in the color of the enamel, the second - by the appearance of a carious cavity and discomfort when consuming sweets, the third - by the appearance of moderate short-term pain when eating cold food. |
| Acute caries (decompensated form) | The pathological process proceeds quickly and intensively, its stages replace each other literally within a few weeks. Depending on the severity of the process, superficial, medium and deep acute caries are distinguished. The first manifests itself as sensitivity to sour or sweet foods, a feeling of being set on edge, the second - destruction of enamel and dentin, the appearance of pain symptoms, the third - pain when exposed to cold, the presence of a large carious cavity filled with softened dentin. |
| According to the depth of the carious process: | |
| Carious spot | There is a change in the color of the enamel in the affected area. A chalky spot with a smooth surface appears on it. If you start treatment at this stage, it will be easier and less expensive. The dentist will first remove the stain, then remineralize the enamel by applying sodium fluoride preparations to it. |
| Superficial caries | The process of demineralization of the enamel starts, so the surface of the chalk stain becomes rough. The affected tooth reacts to cold, hot, sour and sweet foods, but not everyone experiences such symptoms. Treatment at this stage involves grinding down the affected area and restoring the enamel - its remineralization. |
| Average caries | The pathological process spreads to dentin. The patient suffers from pain symptoms that become more frequent, more severe and last longer and longer. Treatment requires removal of the damaged area and filling. |
| Deep caries | Dentin around the pulp is damaged. Treatment of deep acute caries requires removal of the damaged area, application of medications and compounds that trigger remineralization processes, and installation of a filling. If treatment is not started at this stage, the pulp will be involved in the pathological process, pulpitis will begin to develop with severe pain symptoms, followed by periodontitis. |
| According to the occurrence of the carious process: | |
| Primary caries | Develops on a healthy dental unit. |
| Secondary caries | Develops on a tooth that has been filled. |
Isolated dentin caries: what are its features
Sometimes lesions and extensive carious cavities form in the dentin of a permanent tooth while maintaining the integrity of the enamel. This is how isolated, atypical caries develops. Its difference from the classical form is that the carious lesion does not affect the enamel, but immediately passes to the dentin.
This happens, for example, in cases where a person uses fluoride preparations for a long time for preventive purposes. This leads to strengthening of the enamel located on top of the affected dentin, and, as it were, “seals” the pathological process inside the tooth.
Basic diagnostic methods
Independent determination of dentin caries is possible based on pain and other unpleasant symptoms. However, only a doctor can make an accurate diagnosis after conducting a full dental diagnosis. It includes basic and additional research methods.
The main diagnostic methods for dentin caries include the following:
- Probing - using a sharp probe, the doctor determines the presence and depth of carious cavities. If the bottom of the cavity has a soft structure and a light brown color, this may indicate an acute course of caries. Dense pigmented dentin in the bottom area indicates a chronic form of the disease. Also, with the help of probing, you can detect hanging edges of tooth enamel, chips on it, and by the localization of pain during probing, determine the depth of the carious lesion.
- Percussion is tapping on the teeth with tweezers or the back of a dental probe.
- Palpation - feeling.
These methods are used to determine the viability of the pulp, which is especially important in differential diagnosis.
Additional research methods include:
- Thermometry - measuring the temperature of dental tissues.
- Electroodontometry is the study of pulp using electric current.
And the following methods are used to assess the condition of the pulp:
- X-ray - an X-ray of the tooth helps determine the exact location of the carious cavity and its depth.
- Transillumination - the transillumination method is widely used in the diagnosis of hidden dentin caries, for example, with an isolated, atypical form of progression. When transilluminated, healthy tissues appear transparent, while those affected by caries create a shadow effect.
When the doctor has made a preliminary diagnosis based on the above methods, differential diagnosis of dentin caries with other types of dental diseases - enamel caries, pulpitis, periodontitis may be required.
Causes
The cause, as with any caries, is bacteria developing in dental plaque. At the initial stage, the enamel is affected. If at this stage the patient does not go to the clinic and receive treatment, the process progresses. It involves deeper tissues. Dentin is less durable than enamel, so destruction occurs more rapidly. In just a few months, the disease can lead the patient to a prosthetist.
If the destructive process has reached the pulp, acute pain occurs. Such patients require emergency dental care. Through the canal, infection can penetrate into the root area, causing serious complications requiring surgical intervention.
How is dentin caries treated?
Treatment of moderate dentin caries and deep-stage carious lesions is carried out only surgically through preparation of the carious cavity. At any stage of such caries, pain will occur during treatment, so in most cases local anesthesia is used.
Dental treatment of dentin caries takes place in several stages:
- Cleaning the tooth surface from plaque and tartar.
- Selection of the optimal color of the filling, which will closely match the natural shade of the teeth.
- An anesthetic injection with an anesthetic drug into the area of the tooth that requires treatment. To reduce pain, the injection area is lubricated with anesthetic gel.
- Isolation of the tooth from saliva and neighboring teeth using a latex lining - rubber dam.
- Preparing a cavity using a drill. The dentist removes the lesion with caries: aligns the edges of the enamel that hang over the cavity, removes the softened and pigmented layer of dentin, and forms the correct cavity for convenient and high-quality filling.
- Washing, treating with antiseptics and drying the cavity after preparation.
- Acid etching and adhesive application are an important step in the treatment of caries in permanent teeth. These procedures provide better adhesion of the filling to the walls of the cavity.
- Installation of an insulating or therapeutic pad. The first prevents the negative impact of the filling on the dental pulp, the second has a therapeutic effect if it is necessary to relieve inflammation.
- After preparing the cavity and thoroughly preparing it for filling, a filling is installed. Today, fillings are mostly made from photocomposite materials. They dry quickly under the influence of light, have good strength and do not shrink.
- Alignment according to the bite, polishing and grinding help to adjust the filling to the anatomical features of the jaw and give it the necessary aesthetic characteristics.
- Dentist's recommendations for the prevention of recurrent caries, dental care, selection of optimal hygiene products.
At this point, the process of treating medium dentin caries can be considered complete. Therapy for deep caries has its own characteristics. After preparing the cavity, the dentist places a therapeutic pad with calcium on its bottom in the area of the most painful point. Some experts do not recommend completely preparing softened dentin in case of deep caries. After treatment with an antiseptic, they first recommend installing a temporary lining with a therapeutic effect, and after a certain period, removing the temporary filling and performing the final restoration of the tooth.
Doctor's tactics in the presence of root caries
L. A. Lobovkina
Candidate of Medical Sciences, Head of the Treatment and Prevention Department of Branch No. 6 of the Federal State Institution “GVKG named after. N. N. Burdenko" Ministry of Defense of the Russian Federation
A. M. Romanov
Candidate of Medical Sciences, Chief Physician of the Implamed Clinic (Moscow)
Tooth root caries is the result of the interaction of a complex of unfavorable factors leading to the emergence and progression of the demineralization process in the area of the tooth root. Root caries is a serious problem for dentists, as it can minimize the chances of success of therapeutic treatment of a tooth, lead to complications such as fracture of the crown of the tooth, the rapid development of endodontic complications, etc. The tendency for the circular spread of the pathological process can significantly complicate the surgical and restorative treatment of root caries. Ultimately, it is this localization of carious lesions that most often leads to tooth loss [9].
The most typical localization of root caries is in areas of the dentition with low salivary clearance (that is, less well washed by saliva). In the frontal part of the dentition, the exposed buccal surfaces of the roots of the upper incisors are more susceptible to root caries; in the lateral group, the molars of the lower jaw are more susceptible [9].
According to WHO expert forecasts, the problem of tooth root caries among the population of older age groups is steadily growing (Tkachenko O., 2014). The increase in the prevalence of root caries among the population of older age groups is due to an increase in average life expectancy, poor oral hygiene, a lack of effective methods for preventing gum recession, a high incidence of periodontal diseases, etc. [4]. Thus, the critical depth of the periodontal pocket for the occurrence of this nosology is a distance of 2-4 mm from the gingival margin [2].
RJ Billings identifies 3 groups of main risk factors for root caries:
1. biological factors (composition of dental plaque, level of salivary secretion, salivary pH, salivary buffer capacity, hereditary factors);
2. behavioral factors (hygienic behavior, general health awareness, eating habits, socio-cultural behavior, psychological awareness);
3. individual factors (general health, problems of mobility, coordination, understanding, periodontal treatment performed, functional disorders).
However, the key risk factor in the occurrence of root caries is not the amount of plaque, but its qualitative characteristics. While Streptococcus mutans dominates in the microbiological ratio when tooth crown caries occurs, actinomycetes (Actinomyces viscosus, Actinomyces naeslandii, Actinomyces species) predominate in root caries [3, 11].
Features of the development of root caries and its treatment are reduced tissue mineralization, proximity of the pulp, difficulties in preparation and selection of filling material [10]. Consequently, the main task in the treatment of root caries is the competent selection of rational filling material and correct restoration of the root shape, ensuring good hygiene.
In accordance with the principle of minimal intervention, it is advisable to treat a carious stain without a defect in the hard tissues of the tooth, if possible, without filling [4]. It is recommended to use fluoride-containing products in combination with careful regular individual and professional oral hygiene. If there is a defect in the hard tissues of the tooth, surgical treatment is performed.
Very often, during consultations, doctors work only with composite materials, although in some cases their use is unjustified. Despite their high mechanical strength, abrasion resistance, aesthetics and good adaptation to cavity walls, they have a number of disadvantages, including polymerization shrinkage and deformation of large-volume fillings over time, insufficient biocompatibility with hard dental tissues, lack of cariesstatic effect, high cost [ 8].
Glass ionomer cements (GIC) can be alternative materials in a number of clinical situations [5].
The undeniable advantages of the GIC are [6, 7]:
1. Formation of a strong chemical bond with the hard tissues of the tooth.
2. Bioactivity, cariesstatic and antibacterial effect.
The cariesstatic effect is achieved largely due to the prolonged release of fluoride from the cement mass. This process begins immediately after filling and continues for at least one year. Diffusion of fluorine into surrounding tissues causes increased mineralization and promotes the formation of fluorapatites in enamel and dentin. This leads to increased acid resistance and decreased dentin permeability, worsening living conditions for pathogenic microorganisms and preventing the development of recurrent caries.
3. A low modulus of elasticity provides high elasticity, which allows GIC to withstand occlusal loads under fillings and crowns, help compensate for polymerization shrinkage of composite materials, and also eliminate stresses that arise in the cervical region during microbending of the tooth during chewing.
4. The coefficient of thermal expansion of GIC is close to the coefficient of thermal expansion of tooth tissue, which is important for ensuring long-term tightness at the filling/tooth tissue interface.
However, glass ionomer cements also have the disadvantage of high opacity, which does not allow obtaining highly aesthetic restorations when using GIC alone. In this regard, companies producing dental materials are looking for ways to improve GICs, including increasing their aesthetics.
One of such GIC is “Ionolux” (VOCO, Germany), the peculiarity of which is that it combines glass ionomer and composite parts, which determine its excellent properties. Thus, due to the composite component, its aesthetic qualities have improved, the possibility of immediate finishing has become possible immediately after polymerization, the formation of a chemical bond with composites and very low solubility in water have been noted.
Unlike analogues, when working with Ionolux, there is no need for adhesive preparation of hard dental tissues (for example, there is no stage of priming of hard tissues, which is mandatory for some similar materials from other manufacturers), since it is a self-adhesive cement. It is well known that the more curing mechanisms GIC has, the less fluoride ions it releases into surrounding tissues. However, in terms of the release of fluoride ions, Ionolux is not inferior to classical GIC, which is especially valuable in children's and gerontological appointments.
Clinical case
Patient G., 59 years old, complained of an aesthetic defect and pain in the area of 2.2 and 2.3 teeth under the influence of chemical and temperature stimuli (Fig. 1).
Rice. 1. Initial clinical situation: teeth 2.2 and 2.3 - cement caries.
The patient was offered restoration of teeth 2.2 and 2.3, to which she agreed. It was also recommended to undergo orthopedic treatment due to the absence of a large number of teeth.
The preliminary stages included professional, individual oral hygiene, discussion with the patient of the features of the restoration and mutual responsibility for the results of the work.
The choice of color shade was preceded by mechanical cleansing of the vestibular surface of the tooth, symmetrical to the one being restored, and adjacent teeth using a brush and fluoride-free paste (for example, Klint, VOCO, Germany). Next, the color was selected by comparing the color scale included in the set of materials with the shade of the teeth. When performing this stage, the conditions of the optimal light-color environment were observed.
After anesthesia, preparation of defects in teeth 2.2 and 2.3 was carried out with pear-shaped and spherical burs. To ensure a smooth transition of the material, a bevel of the enamel was created towards the cutting edge using fine-grained flame-shaped burs (with red or yellow stripes) (Fig. 2).
Rice. 2. Teeth 2.2. and 2.3 after preparation.
For medicinal treatment of the formed cavities, a 2% solution of chlorhexidine was used. Then Ionolux glass ionomer cement was introduced into the cavity as a base liner (Fig. 3).
Rice. 3. Tooth 2.3: glass ionomer cement “Ionolux” was added.
Next, adhesive preparation of hard dental tissues was carried out, including conditioning the enamel with Vococid gel (35% orthophosphoric acid) and applying the self-etching bond Futurabond HP (VOCO, Germany). The superstable emulsion of nanoparticles contained in Futurabond HP, obtained using the patented Sol-gel technology, allows the material to be applied in only one layer and photopolymerizes for 10 seconds, which ensures extreme adhesion strength and ease of use. A special feature of Futurabond HP is that it releases fluorides, which prevent the development of secondary caries.
It is currently believed that self-etching adhesives are ideal for the restoration of cervical defects in dental hard tissues [3,4]. The fact is that over time, hypermineralization (dentin sclerosis) occurs in the area of the bottom of the defect, leading to the closure of the lumen of the dentinal tubules with mineral crystals, making it difficult for adhesive systems to access these areas. The use of self-etching adhesive systems makes it possible to transform the smear layer and simultaneously decalcify the surface layer in the defect area in combination with preliminary etching of the bevel boundaries with phosphoric acid.
We used Admira as a restoration system»
(VOCO, Germany) - material based on ORMOCERL®. This system includes the Admira microhybrid composite material, the Admira Flow fluid composite and the 5th generation Admira Bond dentino-enamel bond. However, if in a conventional composite the polymer matrix is only organic and shrinks during the polymerization process, then in the Admira material the matrix is inorganic-organic: its basis is an inorganic frame based on silicon oxide. This modification of the resin leads to the fact that after polymerization, almost all of the residual monomer is retained on the side chains, and is not in a free state, as in conventional composites. Therefore, “Admira” is the most biocompatible material, that is, the risk of developing allergic reactions, especially from the gingival margin, is minimized. In addition, this matrix is more wear-resistant.
Currently, a new material from VOCO based on one ceramic is being registered in Russia - «
Admira Fusion
»
(Admira Fusion). Thanks to the innovative combination of already proven nanohybrid technology with ORMOCER® technology, silica forms the chemical basis for both the filler and the resin matrix. This one-of-a-kind Nano-ORMOCER® technology offers a number of advantages, namely high filler content, extremely low polymerization shrinkage and very low shrinkage stress (polymerization shrinkage and polymerization stress levels are more than 50% lower compared to conventional composites). At the same time, “Admira Fusion” is distinguished by very high stability of color tone. The particle conversion rate of the material reaches 95-99%, which is almost the same as that of composites used for indirect restorations (Robert A. Lowe, 2016).
The restoration of tooth 2.2 was carried out similarly (Fig. 4).
Rice. 4. Teeth 2.2 and 2.3: final appearance after restoration.
Finishing of the restorations was carried out using the Safe End system (SSWHITE, USA), which includes carbide 10-, 20- and 32-point tungsten carbide burs. The 10-blade bur is used to remove excess material and contour the restoration. The 20-blade bur provides a smooth surface ready for polishing. Burs effectively remove composite material while preserving as much hard tooth tissue as possible. Unlike other systems, these burs have different lengths, specially adapted to the type of tooth and the area being treated. The tapered shape of Safe End burs is ideal for treating the transition between the composite material and the enamel surface. These burs are easy to clean before disinfection due to the straight blade shape.
In addition, carbide finishing burs have advantages over finely dispersed diamond ones:
- they work selectively (“distinguish” the softer composite from the harder enamel, allowing the natural tooth structures to be preserved);
- have a cutting rather than a grinding mechanism of action, that is, they remove material in the form of chips, which provides a smoother surface compared to diamond burs;
- They have a rounded tip, which allows treatment without trauma to the marginal edge of the gums and the circular ligament.
In order to reduce the marginal permeability of the root surface and to add shine to restorations, it is recommended to coat them with Easy Glaze filled light-curing varnish (VOCO, Germany).
Thus, for the treatment of root caries and filling subgingival defects, it is recommended to use glass ionomer cements, which ensure good adherence of the material to the root surface and isolation of dentin from external cariogenic factors. I would like to note the high efficiency of treatment of root caries using glass ionomer cement “Ionolux” both in the “sandwich” technique and independently in comparison with composite materials.
Literature
- Alimsky A.V. Gerontostomatology: present and prospects // Dentistry for everyone. - 1999, No. 1. - P. 29-31.
- Grudyanov A.I. Periodontology. Selected lectures. - M.: Dentistry, 1997.
- Grudyanov A.I., Chepurkova O.A. Root caries // Institute of Dentistry. - 2003, No. 4. - P. 87-90.
- Dedova L.N., Kandrukevich O.V. Root caries: clinical picture, diagnosis, treatment. Educational and methodological manual. - Minsk: BSMU, 2013.
- Dmitrieva L. A., Borisova E. N. Dental health of elderly and senile people depending on social status. — Moscow, Final Trade Board of the Russian Ministry of Health. Exhibition “Medicine - achievements and prospects”. - March 22-23, 2004.
- Mount G. J. Adhesion of glass ionomer cements // DentArt. - 2003, No. 2. - P. 17-22.
- Mount G. J., Ngo Hien. Bioactivity of glass ionomer cements // DentArt. - 2003, No. 4. - P. 28-33.
- Nikolaev A.I., Tsepov L.M. Practical therapeutic dentistry. - M.: MEDpress-inform, 2007.
- Solovyova A. M. Root caries and the role of fluoride prophylaxis in its prevention and treatment // New in dentistry. - 2011, No. 3. - P. 36-37.
- Schmidseder D. Aesthetic dentistry. Atlas of dentistry. - M.: MEDpress-inform, 2004.
- Nyvad B., ten Cate GM, Fejerskov O. Microradiography of experimental root surfasce caries in situ. G.Dent. Res 1997;78;12:1845–1853.
Prevention of dentine caries in permanent and baby teeth
Measures to prevent dentin caries are similar to the prevention of caries in other parts of the tooth.
These include:
- Proper nutrition with a minimum amount of sugars and fast carbohydrates, rich in fluoride, calcium, phosphorus. Avoiding frequent snacking.
- Thorough daily brushing of teeth twice a day using a toothbrush, paste, and floss. The additional use of an irrigator to clean hard-to-reach places and interdental spaces, as well as mouth rinses, helps reduce the risk of caries.
- Schedule a visit to the dentist twice a year, as well as immediately contact a doctor at the first sign of caries.
- Professional teeth cleaning using special equipment twice a year.
- If necessary and as prescribed by a doctor, use vitamin-mineral complexes, which contain components beneficial for dental health.
- Drinking fluoridated drinking water, which is enriched with minerals.
Compliance with these preventive measures allows you to maintain the health and beauty of your teeth and reduces the risk of developing caries and other dental diseases.
Diagnosis of cement caries
Unfortunately, it is impossible to diagnose the disease yourself. The patient can only feel a reaction to cold and hot drinks. This discomfort is fleeting and most people do not pay attention to it. And only a comprehensive dental examination will allow you to make the correct diagnosis.
For diagnosis, a Family Dentistry specialist:
- cleans the gums and removes subgingival deposits using hand instruments, ultrasonic instruments and Air Flow treatment;
- isolates the root from saliva secretion using a rubber dam - a special latex membrane;
- probes the root surface with a sharp probe to detect roughness characteristic of caries;
- prescribes radiovisiography, which will detect even the smallest subgingival and perigingival defects and carious processes at any stage;
After a set of examinations, the dentist may prescribe additional ones to confirm the diagnosis of cement caries and refute suspicions of pulpitis or periodontitis. This can be thermometry (checking the tooth’s reaction to hot and cold), EDI (checking the pulp’s reaction to current), etc.