From this article you will learn:
- what methods of treating pulpitis allow you to keep the tooth alive,
- what is the vital amputation method,
- stages of biological treatment of pulpitis.
The biological method of treating pulpitis is a conservative method that is aimed at completely preserving the pulp as viable. The use of this method is possible only if the following 2 conditions are met. Firstly, the patient should seek help from a dentist at the earliest stage of the development of pulpitis, i.e. at the very beginning of the development of pulp inflammation. Secondly, the age of the patient to whom the doctor can offer this method is very important, because Treatment without nerve removal is carried out only in children, adolescents and people no older than 25-27 years.
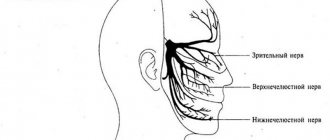
The latter is associated with the ability of the dental pulp to heal itself, which also depends on the age of the patient. In addition to the biological method, there is also a method of vital amputation, in which the pulp remains partially viable. This method involves removing the pulp only from the coronal part of the tooth, preserving it in the root canals. But the indications for such therapy are limited - it can only be carried out in multi-rooted teeth (they have a clearly defined transition between the coronal and root pulp).
Important: in dentistry, unfortunately, doctors very rarely offer conservative methods for treating pulpitis, even if the patient is suitable for their use. This is due to the flow of patients and the desire to use the usual familiar methods. It is best to ask your doctor whether such treatment methods are indicated for you, and if he answers “no,” then you must clarify: “why this method is not indicated specifically for you.”
Pulpitis of the tooth and its treatment
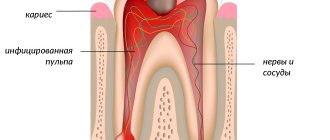
A characteristic sign of this pathology is inflammation in the pulp, which is located inside the tooth cavity, where blood vessels and nerves are concentrated. The cause of inflammation is the penetration of harmful bacteria into the cavity due to damage to the external dental tissues (enamel and dentin). This is the destruction that we most often owe to untimely treatment of deep dental caries: pulpitis becomes a consequence of the carious process. Much less often, it appears due to mechanical damage to the pulp, poor preparation of the tooth for filling, and unprofessional installation of orthopedic structures.
Treatment methods for pulpitis
In dentistry, two main methods are used to treat dental pulpitis in adults and children:
- biological - drug treatment of pulpitis with antibiotics and medications;
- surgical - treatment of pulpitis by amputation (partial removal of the pulp) or extirpation (in which the nerve of the tooth is completely removed).
The choice of technique remains with the dentist. The doctor studies X-ray diagnostic data, interviews and examines the patient. Based on these data, he selects the most rational method of treating pulpitis for a particular case.
New options for the treatment of deep caries
In the treatment of carious processes, it is important not only to possess manual skills and be aware of new filling materials, but also to know the biological characteristics of caries and dental pulp. There is no longer a need to prepare a tooth far beyond the boundaries of healthy tissue; on the contrary, with the development of adhesive dentistry, we try to excise tissue as conservatively as possible. Even the removal of tissue that could potentially be infected remains questionable.
This article discusses the treatment of deep caries, and also tries to answer some questions posed in the dental literature. Is it necessary to remove all carious tissue in every clinical case (even when the excavation is close to the pulp chamber)? Can the carious process be stopped? What type of filling material will provide the best result for the patient?
Traditional Concepts
In a classic text (1908), GV Black wrote: “It is better to expose the pulp of the tooth than to leave it covered only by a layer of softened dentin.” At the same time, Black argued that dentists must understand the pathological anatomy and pathophysiology of the carious process, otherwise they can consider themselves only mechanics. Of course, dental science has advanced our understanding of the caries process and the possibility of sealed fillings that recreate grooves and fissures. GV Black himself would probably refute his statement 100 years later.
The traditional concept of complete removal of carious tissue in deep cavities has been called into question. Absolute removal of all altered tissue may not be necessary to stop the carious process. It is well known that bacteria in dentin cause inflammation in the pulp. However, this weak inflammatory process can be a stimulator of regeneration. Leaving a small amount of carious tissue under the filling does not necessarily have a detrimental effect on the success of the treatment. Short studies from 36 to 45 months showed that reliably filled cavities with carious dentin showed a low percentage of relapse and an absolute decrease in the number of microorganisms. Remineralization of remaining carious dentin has been proven both biochemically and radiologically. Calcium hydroxide pads were used in these studies.
Leaving decay underneath a filling is a controversial concept. The traditional approach of indirect pulp capping usually requires a temporary filling. After a few weeks or months, the tooth is reopened, the remaining carious tissue is removed, and the filling is refilled permanently.
In the indirect method, demineralized tissue is left in the deepest parts of the cavity to prevent pulp exposure. The use of this method is limited to patients without symptoms of inflammation and pulp pathology. Complete removal of all carious tissue from the walls of the pulp chamber is necessary to control microleakage. The lesion may progress slowly or rapidly. It has been clinically, radiologically and bacteriologically proven that the carious process stops. In such cases, a sealed, well-fitting restoration is a prerequisite for a successful outcome.
Classic indirect pulp capping has a relatively high clinical success rate, pulp exposure is usually avoided and the tooth is not disturbed. Dentin during the second opening is described as drier, harder and darker. Microbiological tests reveal a decrease in bacterial contamination. It is also possible that the success of such treatment will depend on the chosen filling material, but too little research has been conducted on this matter. “Indeed, careful access may be preferable to radical excavation, because the pulp is exposed much less frequently, and the hermetically sealed separation of dentin from the oral microflora stops the development of the carious process. The restorative processes of sclerosis of dentinal tubules and the formation of tertiary dentin are stimulated, thereby reducing the permeability of the remaining dentin. Microorganisms are blocked on one side by a hermetically sealed filling, and on the other by reduced permeability of dentin.
Changing landmarks
It has long been accepted by everyone that the use of sealants protects the underlying tooth structure, preventing plaque accumulation and mineral loss. More recently, evidence has shown that reversal of non-cavitary caries lesions is possible with the use of sealants. But so far this non-invasive method of treating initial caries has not been widely introduced into dental practice.
The final outcome of conservative excision and complete excavation was carefully compared. In this study, in cases where placement of a temporary filling was possible, deep excavation was not performed. Soft, moist and discolored dentin was left at the bottom of the pulp chamber. A calcium hydroxide liner was placed over the carious dentin, which was then covered with a temporary glass ionomer cement filling. After 8-12 weeks, the cavity was reopened for the purpose of final excavation. The calcium hydroxide liner was placed again and the tooth was restored with composite material. The authors observed a much smaller number of exposed pulp chambers when carrying out step-by-step removal of carious tissues than during complete radical excavation.
In addition, when assessing long-term results after 1 year, the above method also turned out to be more successful. These results once again put emphasis on the importance of maintaining the dentinal barrier between the pulp and the cavity, even if carious lesions remain in it.
More recently, the need for step-by-step removal of carious dentin has been discussed again. Indirect pulp capping is a simple, well-accepted procedure that is less expensive than endodontics. Although some microorganisms may remain active, this is rarely enough to cause relapse: deposition of tertiary dentin also stops the decay process. All infected dentin should be completely removed from all walls, however, some may be left along the bottom of the cavity. Radical removal of altered dentin is not necessary in all clinical cases, since a hermetically installed filling reliably closes the cavity from oral microflora.
Therapeutic pads: effect on tooth pulp
Spacers are often placed under restorations to reduce potential field sensitivity. The following characteristics are important for an ideal installation:
1. The ability of the material to destroy microorganisms 2. Induction of mineralization 3. Provide a tight fit and insulation
Postoperative sensitivity is due in part to residual dentin thickness (RDT) after preparation and the presence of some microorganisms on the cavity walls. No material can protect the pulp better than natural dentin. The residual dentin thickness at the bottom of the cavity is one of the most important factors for protecting the pulp from toxins. A thickness of 0.5 mm reduces the effect of toxins by 75%, 1 mm - 90%, maintaining 2 mm or more leads to an incredibly small reaction of the pulp or its complete absence. In situations where about 0.5 mm remains, the use of spacers is especially important. With a decrease in the thickness of the dentinal layer, the survival of odontoblasts and the preservation of reparative mechanisms decrease.
Reactive dentin restoration was observed under cavities with both RTD greater than 0.5 mm and RTD less than 0.25 mm. However, maximum activity was observed under cavities with RTD between 0.5 and 0.25. Dentin restoration was also influenced by the material chosen (from most to least: calcium hydroxide, composite, modified GIC, and zinc oxide eugenol). Odontoblasts persisted at RTD greater than 0.25 mm.
Calcium hydroxide has been used as a gasket material since the 1920s. Due to its pH of 11, calcium hydroxide itself is bactericidal and also neutralizes acidic bacterial products. High pH creates good conditions for dentin repair. In addition, calcium hydroxide has the ability to mobilize growth factors in the dentin matrix, causing the formation of new dentin. Calcium hydroxide is an ideal lining material for very deep cavities for both direct and indirect pulp capping.
Adhesive resins may be too acidic and cause pulp irritation. And many dentin bonding agents and modified GICs are generally toxic to pulp tissue. Also, calcium hydroxide linings show a high potential for restoring soft tooth tissue, compared to cements and resins.
Unfortunately, self-curing calcium hydroxide pads are highly soluble and can dissolve over time. Traditional hydroxide gaskets dissolve easily during acid etching. Bond components: water, acetone, alcohol can also have a destructive effect on the properties of calcium pads. Sealing the cavity will help stabilize the lesion and stop the carious process. Thus, if a composite filling is planned, a protective GIC gasket should be installed on top of the hydroxide gasket.
Restorative materials that have antimicrobial properties are especially useful in minimally invasive and other types of dental procedures. Some studies show that modified GICs perform almost identically to conventional calcium hydroxide gaskets. Left soft, demineralized dentin becomes remineralized after GIC coating. This is mainly due to the release of fluoride and the presence of calcium phosphate in the cement. This phenomenon is also called “healing of diseased dentin.” However, in some other studies, modified GIC had a detrimental effect on monotoblasts, reducing their number. Therefore, before introducing the modified GIC into a deep cavity, it is recommended to lay at least a thin layer of calcium hydroxide. This allows the pulp to be protected from damage and bacterial microleakage.
In the last few years there has been a presentation of MTA (ProRoot MTA Dentsply Tilsa Dental Specialties). These silicate cements are antibacterial, biocompatible, have a high pH and allow the release of bioactive dentin matrix proteins. MTA is a powder consisting of hydrophobic tricalcium silicate, tricalcium aluminate, tricalcium oxide and silicate oxide. This mixture also contains small amounts of other oxides, which modify its chemical and physical properties. Adding liquid to the powder results in the formation of a colloidal gel with a pH of 12.5 (similar to calcium hydroxyl), which cures to a dense substance within 3-4 hours. There is a hypothesis that under the influence of tissue fluid, tricalcium oxide is converted into calcium hydroxide.
The material has low solubility and is slightly more radiopaque than dentin. Since MTA has very little resistance to compression, it should not be used in high-functioning areas. Another significant drawback is the long curing time: several hours.
To summarize, we can say that a two-stage treatment procedure is often important and requires a temporary filling. Indirect pulp capping is best performed in one visit. Any one-step restoration requires the application of a layer of modified GIC. MTA is an excellent material for pulp exposure and endodontic procedures. The material has good insulating properties, and some studies have shown greater treatment success than using conventional calcium hydroxide.
Clinical cases
Clinical case 1
The case report presents a 30-year-old patient with a large cavity on the lower first molar (Figure 1). The patient noted sensitivity of the tooth to cold, otherwise the caries was asymptomatic. The cold test confirmed the patient’s words; the pain attack lasted about 30 seconds. A targeted x-ray showed a close fit of the cavity to the dental pulp. Excavation of carious dentin continued until the dentin wall approached a thickness of 1 mm (Figure 2).
Photo 1. Large carious cavity with minimal symptoms.
Photo 2: Partial removal of carious dentin was carried out. Soft, moist, discolored dentin at the bottom of the cavity is left.
Biodentine (Septodont) was used to place a temporary filling (Photo 3). The tooth was left to recover for 4 months. During this period the tooth did not bother me. To confirm the vitality of the pulp, a cold test was again performed and a targeted x-ray was taken (Photo 4). The decision was made to restore the tooth with composite as the definitive restoration (Figure 5).
Photo 3: Biodentin (Septodont) - temporary filling.
Photo 4: X-ray of a temporarily filled tooth. The remaining caries is clearly visible in the picture. At the discretion of the dentist, a certain amount of Biodentine may be left for permanent restoration.
Photo 5: Final restoration of the tooth.
Discussion of the material
Based on the author's experience, the use of Biodentine is much more convenient and effective compared to MTA. Biodentine is a bioactive material for direct and indirect pulp capping, as well as in endodontic practice. The manufacturing process of biosilicate materials eliminates metal contamination. The curing process occurs when tricalcium silicate is moistened, which then forms calcium silicate gel and calcium hydroxide. When these substances combine with phosphate ions, a precipitate resembling hydroxyapatite is formed. “At the junction of dentin and Biodentin material, there is an increase in carbonate compounds, indicating the diffusion of minerals from the material to create a hybrid zone.” Biodentine prevents microleakage similar to modified GIC and also has an antibacterial effect.
Biodentine is completely cured in 10-12 minutes. This is much faster than the curing time of MTA, but biodentine also exhibits higher compression resistance. Thus, it can be easily used as a suitable temporary filling. The manufacturer recommends using the material in 2 steps. At the subsequent appointment, the dentist forms the cavity he needs and leaves a layer of Biodentine at the bottom as a spacer, on top of which he installs a permanent restoration.
Clinical case 2
The lower molar in photo 6 had a defective amalgam filling with recurrent caries. The filling is removed, the altered dentin is removed. A thin layer of TheraCal LC liner (BISCO Dental Products) was applied to the bottom of the cavity using a syringe (Photo 7) and then light-cured for 20 seconds. The cavity is etched (Photo 8), washed, coated with adhesive, dried and cured (Photo 9), and the tooth is now ready for a permanent filling.
Photo 6: Deep excavation of dentin.
Photo 7: Light-curing modified calcium silicate material TheraCal (BISCO Dental Products) was used as a lining.
Photos 8 and 9: Acid etching and installation of the seal is performed on top of the gasket.
Discussion of the material
TheraCal LC is another recently introduced material that combines the beneficial properties of calcium hydroxide and modified GIC.
The material has strong mechanical properties, low solubility, and can be cured in 1mm layers. TheraCal LC is an approved hydroxyapatite stimulant with crystal synthesis inducing properties similar to MTA products.
Dentin fluid absorbed by TheraCal releases calcium and hydroxide ions. Calcium is necessary for rapid stimulation of apatite synthesis, and an alkaline environment provides the necessary conditions for restoration and healing. TheraCal LC is designed to be used as an insulating liner to provide superior pulp protection. In direct pulp capping, the use of a rubber dam and control of pulp bleeding are important aspects of successful treatment. The material is suitable for professionals who want to make it easier to use conventional calcium hydroxide gaskets, but still want to take advantage of the benefits of newer calcium silicates. TheraCal LC allows for indirect pulp capping in one step.
Conclusion
Today, the dentist needs to analyze previous experience and clinical cases to provide optimal treatment to the patient. There is now a significant body of literature describing successful indirect pulp capping. At the same time, analysis of the information allows us to conclude that direct coating, especially in mature teeth, cannot achieve the same success without endodontic therapy. There are also situations where dentists prefer to perform indirect plating and then re-enter the cavity to remove any remaining carious tissue.
This article shows that a step-by-step dentin removal technique is not always necessary. New calcium silicate cements may be particularly useful in such cases. For general acceptance of such a concept, continued clinical research is of course necessary. Dentists should also be aware that in some cases, the material covering the pulp should not be completely removed and left for a permanent restoration.
Posted by Robert E. Rada, DDS, MBA
Biological method of treating pulpitis
If the disease has become chronic, a biological method or conservative treatment of pulpitis with calcium is used. The process involves applying therapeutic pads containing calcium preparations. The technique is also used in the following cases:
- if the pulp was accidentally exposed during the caries treatment procedure;
- when you need to strengthen the bone partition between tooth enamel and pulp.
The specialist applies a drug for the treatment of pulpitis to the site of thinning bone tissue and thereby strengthens it. Next, the tooth is filled and monitored over time, conducting X-ray examinations at certain time intervals. The method is suitable:
- children with baby teeth;
- patients under 30 years of age during the treatment of reversible pulpitis;
- everyone who takes special care of their oral cavity.
If, after treatment of pulpitis, the tooth aches, hurts when pressed or bitten, and the pain remains for a long time, intensifies at night, and becomes long-lasting, you must return to the clinic. Aching pain during the treatment of pulpitis indicates that more radical, that is, surgical, methods are needed.
Chronic pulpitis
In the chronic course of pulpitis, there are no obvious symptoms. Sometimes a slight aching pain may occur, especially after cold or hot drinks or meals. Exacerbations, which are similar in their symptoms to acute pulpitis, are also possible.
When pus accumulates, flux appears. If a person is not provided with proper medical care, this can lead to phlegmon and related complications:
- damage to the jaw bones and facial nerve;
- abscess;
- apical periodontitis;
- sepsis;
- chronic hyperplastic pulpitis (occurs in childhood and adolescence).
How is pulpitis treated surgically?
As we have already noted, there are two possible options for surgical intervention:
- treatment of pulpitis using the amputation method with partial preservation of the pulp;
- treatment with complete removal of soft tissues, blood vessels, and nerves.
If there is an objective possibility, the doctor will remove only the top of the pulp - from the crown, leaving the root part. The blood supply and sensitivity (innervation) of the tooth will be preserved. The technique is used in the treatment of children - for milk or permanent teeth that have not yet fully grown. This allows them to form normally in the future. Treatment for pulpitis can be carried out in one visit.
Vital amputation
This procedure involves preserving the pulp in the dental canals, but at the same time it is removed from the crown area. Vital amputation is done in cases where a multi-rooted tooth is affected. It is not used on single-rooted plants due to the lack of a boundary between the root and the coronal pulp zone.
Treatment proceeds as follows:
- Anesthesia (local) is performed.
- The doctor drills out carious lesions.
- The pulp is removed.
- Tissues are treated with drugs.
- The dentist makes an insulating pad.
- A temporary filling is placed.
Subsequently, the specialist may recommend physical therapy and medication.
Treatment of acute pulpitis
The above methods are ineffective in treating exacerbations of chronic pulpitis, an acute disease when the tooth becomes a source of unbearable pain radiating to the ear, temple, and back of the head. With these symptoms, endodontic treatment of pulpitis is carried out - with cleaning of the root canals and complete removal of the pulp.
In dentistry, two modern methods of treating tooth canals for pulpitis are used: devital and vital.
- Treatment of pulpitis using the vital amputation method is carried out by removing the nerve, washing, cleaning and filling the canal.
- Devital treatment of pulpitis involves the use of medicinal pastes and requires several sessions.
These treatment methods are most often used for pulpitis on permanent teeth.
Why is it so important to keep the tooth alive?
The thing is that the pulp performs trophic (nourishes the tooth tissue from the inside) and protective functions. After its death, the hard tissues of the tooth become more fragile, in addition, removal of the pulp is tied to the need to remove a sufficiently large volume of hard tissues of the tooth. Also, very often after pulp removal, inflammatory foci appear in the area of the apex of the tooth roots, associated with poor-quality filling of the canals after pulp removal.
Of course, to avoid all this, it is better to try to leave the pulp alive. However, this is also not always possible, because Patients very rarely come at the very beginning of the development of pulpitis, when the use of conservative treatment methods brings good results. More often, patients come with diffuse purulent inflammation of the pulp, when only its complete removal is indicated - followed by filling the root canals.
Read more about the treatment method with complete removal of the pulp in the article: → “Traditional methods of treating pulpitis”
Stages and stages of tooth treatment for pulpitis using the devital method
- Stage I.
The tooth is anesthetized and the carious cavity is cleaned. The pulp cavity is opened. - Stage II.
A devitalizing paste is placed into the exposed pulp and the tooth is filled for 3 to 7 days. People still call the paste “arsenic,” although it has nothing to do with this substance. - Stage III.
During your next visit, your dentist will clean the root canals according to medical protocol. - Stage IV.
If there is a risk that the tooth will crack, it is covered with a crown. If the hard tissues are well preserved or only slightly damaged, they are restored. The tooth is strengthened with a fiberglass or metal anchor pin and securely filled with photopolymer material.
The treatment time for pulpitis depends on how damaged the tooth is, the age of the patient, whether there are complications, and how many root canals should be treated.
Types of pulpitis
In many ways, the choice of treatment strategy depends on the type of pathology. Acute pulpitis
characterized by severe pain, reaction to cold and heat, but these are periodic outbreaks of pain.
Chronic fibrous pulpitis
may not be accompanied by pain at all.
Hypertrophic pulpitis
is a consequence of untreated fibrous pulpitis. It is distinguished by the presence of a polyp and more severe pain.
Gangrenous pulpitis is a more severe pain syndrome and a sharp reaction to hot, but not to cold. Acute chronic pulpitis
The same thing happens and is characterized by severe pain, not due to any reasons or irritants.
Is it painful to treat pulpitis?
Many patients believe that treatment for pulpitis is painful. In fact, pain accompanies the disease itself, and not the procedure for its treatment. The pulp tissue and nerves become inflamed, which causes unbearable painful sensations comparable to an electric shock. Pulp removal is absolutely comfortable, because high-quality anesthetics completely relieve the patient of pain while the doctor prepares the canals. During treatment or after treatment of pulpitis, the tooth hurts when the internal tissues are severely inflamed. Then safe painkillers are prescribed while healing occurs (1 - 3 days).
Causes of pulpitis
The main reason causing the development of pulpitis is caries, the treatment of which was not carried out on time. If a person delays treatment of caries until the last minute and does not go to the dentist, his risk of encountering pulpitis is extremely high, because caries is a constantly progressive disease that destroys tooth tissue. And sooner or later the destructive process reaches the pulp. Therefore, one of the basic principles of pulpitis prevention can be formulated as follows: if you don’t want to encounter pulpitis, don’t delay caries treatment!
Treatment of pulpitis will be much more complex and expensive than treatment of caries. Moreover, when treating advanced pulpitis, it is not always possible to save a tooth. Therefore, you need to forget about the fear of dentists and always consult a doctor in a timely manner for the treatment of caries! Nowadays, there are technologies that make it possible to successfully treat caries without pain and discomfort for the patient - for example, dental treatment under sedation, treatment without drilling a tooth.
Less commonly, pulpitis and the need for its treatment may arise for the following reasons:
1. Low quality of dental treatment. If, when treating caries, the dentist incorrectly treats the carious cavity or makes other mistakes and inaccuracies, tooth pulpitis may develop under the installed permanent filling.
2. Low quality of teeth preparation for prosthetics. Before prosthetics, the teeth are ground for the future prosthesis, and if, while working with a living tooth, the dentist overheats its tissues, pulpitis may develop. This will not happen immediately, but after some time, but pulpitis under the crown is almost always a sign of poor quality work by the orthopedic doctor. To treat pulpitis, the crown will have to be removed.
If you do not want to encounter pulpitis and other complications after poor-quality dental treatment, you must remember one simple rule: for dental treatment, you should not choose a clinic at the lowest price, but find out all the available information on its equipment and the level of qualifications of the doctors working there!
3. The cause of the development of pulpitis can also be gum disease. For example, periodontal disease causes exposure of tooth roots, and at the same time, a deep periodontal pocket is formed in the area of contact between the gum and tooth, in which pathogenic microorganisms will actively develop, causing the appearance of caries and then pulpitis. Therefore, treatment of gum inflammation also does not need to be postponed; if you see that your gums are inflamed, be sure to visit the dentist’s office!
Very rarely, pulpitis occurs due to injuries leading to tooth fracture. If the injury damaged not only the pulp, but also the root of the tooth, the only treatment that can be done is to remove the tooth.
For whatever reasons, pulpitis appears, its treatment must be carried out as urgently as possible. Timely and high-quality treatment of pulpitis makes it possible to keep the tooth alive, and, as you know, your natural teeth are better than any dentures!
Possible complications
If you delay visiting the dentist, inflammation can spread to the bone tissue of the tooth - periodontium. This is how one of the most common and dangerous complications of this disease begins - periodontitis, which can lead to tooth extraction. Periodontitis also occurs due to an unskilled approach to cleaning root canals.
If you are concerned about an elevated temperature after treatment for pulpitis, urgently contact a more reputable dentist, as the inflammation is progressing. Professional clinics use modern methods of canal treatment using microscopes, binoculars, visiographs, endomotors, and apex locators. These instruments prevent the risk of complications.
Unfortunately, pulpitis remains a common occurrence after caries treatment. The reason for its appearance is the same - the unprofessional actions of a doctor who violated medical protocols and made mistakes when filling. Perhaps he accidentally opened the pulp and gave bacteria access to it.
What is pulpitis in children
Tooth pulpitis in a child is a protective reaction of the body to potentially dangerous irritants that arise inside the chamber and canals of the tooth. Dental pulpitis is most often caused by bacteria entering the chamber through carious cavities. The inflammatory response begins when substances produced by microorganisms are recognized. Numerous cells of the immune system enter the tooth chamber, which act in two ways.
If pulpitis is detected at an early stage and the cavity is treated properly, the changes can be reversible. However, with prolonged development of the disease, the tissue filling the tooth cavity is significantly damaged. Increasing pressure can push infected masses onto surrounding tissue, causing infection and inflammation to spread.
How much does tooth treatment for pulpitis cost?
The final cost of pulpitis treatment is influenced by many factors: the degree of destruction of hard tissue, the number of canals in the tooth, the presence of complications, concomitant diseases, and the chosen treatment method. If the tooth is permanent and has one canal, then the procedure in Moscow clinics will cost from 5,000 rubles. This amount includes a full range of services: x-ray diagnostics, application of anesthetic, installation of a rubber dam, treatment of caries, treatment of dental canals with cleaning, installation of a filling. Price may change if multiple sessions are required.
Pulpitis in children: classification
Depending on the degree of the process, partial or complete gangrene of the tooth is distinguished:
- When the caries process affects only part of the pulp of a given tooth, it is called partial gangrene. The rest of the living tissue is in constant contact with necrotic masses and toxic bacterial products. It is subject to constant destruction and chronic inflammation.
- If the entire pulp inside the chamber and the canals of the tooth are necrotic and also infected with anaerobic bacteria, this condition allows a diagnosis of complete gangrene.
Symptoms of pulpitis
Symptoms characteristic of pulpitis, regardless of the tissue in which the process develops:
- pain,
- redness of the gums,
- edema,
- increased heat,
- chewing dysfunction.
Pain during pulpitis can be provoked or spontaneous, depending on the presence of an irritating factor. The pain response to irritants that damage the pulp is normal. The discomfort goes away as soon as the cause is eliminated. However, if in this case the pain continues, even if the pulp is not irritated, this indicates the development of an inflammatory process and is called prolonged provoked pain. Patients often complain of discomfort when eating and drinking, especially hot or cold temperatures.
In case of complete necrosis and gangrene of the tooth, the patient experiences virtually no pain. The damaged endings of the nerve fibers of the rotted tissue do not transmit any impulses. Tooth gangrene is also indicated by an unpleasant odor from the mouth and an aftertaste in it, the source of which is decaying pulp cells.
On the outside, a tooth with pulpopathy (pulp disease) usually has numerous discolorations, dullness, or carious lesions at various stages of development. If the tooth reacts with pain to percussion, this means that the inflammation has progressed and spread to the periapical tissue. In difficult cases, the doctor may use a spot x-ray to assess the severity of the inflammation and serve as a guide to monitor treatment.
Complications of dental pulpitis
If pulpitis in children is not treated, inflammation continues to spread to neighboring tissues. It spreads from the chamber of the tooth to the canals and periapical region. A periapical abscess causes acute spontaneous toothache, swelling, redness and increased warmth over the inflamed part of the face.
Pus, rich in bacteria and immune system cells, is a thick fluid that collects in a confined space, pressing on adjacent structures and eventually developing into a subperiosteal abscess. At this stage of the disease, symptoms are even more severe. There may also be general symptoms such as fever, lack of appetite, chills or lethargy.
In some cases, the protective layer breaks through and the contents spill into the free space around it. This is how a submucosal abscess is formed. This is usually accompanied by a decrease in pain, but there is a high probability of infection spreading to adjacent teeth.
When infectious inflammation affects the labrum, which shares the bloodstream with the blood vessels of the brain, the dangerous result of cavernous sinus thrombosis can occur. In some cases, the consequence of pulpitis is the penetration of microorganisms into the chest through the parapharyngeal or retropharyngeal space and the formation of anterior or posterior mediastinitis.