Reasons for the development of pathology
The formation of an acute purulent process in the subcutaneous fat layer near the lymph nodes can be triggered by a significant decrease in immunity. If there is inflammation of the lymph node itself, then a delay in lymph outflow and increased vascular permeability are observed.
Adenophlegmons develop due to ongoing inflammatory processes of any localization. Often this pathology is diagnosed against the background of malignant tumors, some types of dermatitis, chronic dental pathologies, and inflammation of the tonsils.
Diagnostics is aimed not only at identifying adenophlegmon, but also at establishing the cause of its occurrence - medical tactics for this pathology depend on this.
TOPIC "LYMPHADENITIS, ADENOPHLEGMON, PAROTITIS"
1.
Information on the topic
Lymphadenitis -
inflammation of the lymph node.
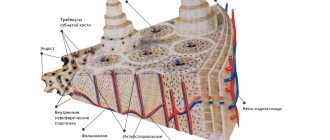
Inflammatory processes in the lymph node usually develop secondary. Primary foci may be infections of the ENT organs, an infected wound, a boil and other inflammatory processes. It should be noted that the frequent development of lymphadenitis in children in the first years of life is due to the functional and anatomical immaturity of the lymphatic system. Most often in childhood, the lateral cervical, submandibular, chin, and occipital nodes become inflamed. On the upper limb - axillary, on the lower - inguinal. When edema and infiltration spread to the perifocal tissue, periadenitis occurs, and in young children, especially newborns, adenophlegmon
(diffuse spread of inflammation beyond the lymph node capsule through tissue spaces).
Mumps -
inflammation of the parotid gland is rare in children. Infection occurs ascending from the oral cavity through the excretory ducts or hematogenously. In the later stages of the disease, abscess formation may occur. It should be emphasized that in infants with this pathology, the inflammatory process rarely remains localized and spreads to surrounding tissues.
Timely diagnosis, correct diagnostic and therapeutic measures at the prehospital stage can prevent the development of severe complications in lymphadenitis, adenophlegmon and mumps.
2.
Educational goal
Mastering techniques for diagnosing lymphadenitis, adenophlegmon and mumps, formulating correct diagnoses, prescribing adequate therapy, timely referral to a specialized department for treatment, including surgery.
3. Specific goals
To fulfill the educational goal, the student must:
| Know | Be able to |
| 1. Classification of lymphadenitis. 2. Clinical picture of lymphadenitis, adenophlegmon and mumps. 3. General principles of diagnosis and formulation of diagnosis. 4. Differential diagnosis with diseases with similar symptoms. 5. General principles of therapy at the prehospital stage. 6. General principles of surgical treatment | 1. Correctly collect an anamnesis of the development of the disease and be able to interpret it. 2. Identify clinical signs of lymphadenitis, adenophlegmon and mumps. 3. Interpret ultrasound data. 4. Diagnose and provide treatment |
Symptoms of adenophlegmon of different types
Symptoms depend on where adenophlegmon developed:
- With submandibular adenophlegmon, body temperature rises, swallowing may be difficult, problems with speech arise, swelling forms in the affected area, redness of the skin and pain when palpated are observed.
- With adenophlegmon of the neck, symptoms appear only when there is a critical accumulation of coccal microflora in the tissues of the anterior or lateral part of the neck. There is an increase in body temperature, pain when feeling the neck, redness of the skin, but swelling may be absent.
- With inguinal adenophlegmon, the clinic develops against the background of an inflammatory process in the genitourinary system. This type of adenophlegmon is characterized by rapid progression, while the patient experiences severe pain, due to which he cannot move freely. There are also signs of general intoxication of the body.
- With adenophlegmon of the axillary region, symptoms more often occur with open wounds of the upper extremities. Signs are pronounced: enlargement of regional lymph nodes, deterioration of general condition (including increased body temperature).
The symptoms for different types of pathology in question are similar, the differences lie only in the location of the lesion. If adenophlegmon occurs in children, then loss of appetite, increased drowsiness, lethargy, and lack of interest in games and others will be noted.
"Phlegmon of the neck"
General information about phlegmon of the neck and its ultrasound diagnosis.
Description of the disease
Diffuse purulent inflammation develops in the subcutaneous fat and is not limited to one area. The inflammatory process can spread rapidly, threatening the patient's life. Severe pathology can ultimately lead to sepsis. Therefore, when you notice the first symptoms, it is important to seek medical help.
Cellulitis most often develops as a complication of another infectious disease. In this case, the pathological microflora enters the fatty tissue from other systems of the body through the blood and lymph flow. Secondary phlegmon often develops if the patient does not adequately treat purulent processes (furunculosis, carbuncles, abscesses). In most cases, the causative agent is Staphylococcus aureus. Less commonly, other pathogenic organisms - E. coli, streptococcus, Proteus - can be detected during the diagnostic process.
Primary phlegmon develops quite rarely due to the introduction of pathogenic microorganisms into the soft tissues through wounds or cuts on the neck.
Cellulitis is severe due to diabetes mellitus. Rotting processes occur at an accelerated pace. In 10% of cases the disease is fatal.
Classification
Inflammation can occur in acute and chronic forms. In the second case, the disease is characterized by a sluggish course and the absence of acute symptoms. There are periods of remission, when any complaints are completely absent, and exacerbations, when all the symptoms characteristic of the acute form of the disease appear.
Depending on the depth of the inflammatory process, the following forms of the disease are distinguished:
- deep phlegmon (inflammation is localized under the connective membrane of the muscles);
- superficial phlegmon (pathogenic microflora develops in the subcutaneous tissue).
Depending on the location of the infection, the following types of disease occur:
- mental phlegmon;
- submandibular phlegmon (often occurs as a complication of diseases of the molars);
- phlegmon of the posterior surface of the esophagus;
- phlegmon of the sternal fossa;
- phlegmon of the anterior surface of the trachea;
Also, all phlegmons are divided into unilateral and bilateral. If we are talking about a unilateral form of the disease, there are:
- phlegmon of the back of the neck;
- phlegmon of the anterior surface of the neck;
- lateral phlegmons.
Cellulitis of the neck is a dangerous pathology that threatens life
Depending on the factors contributing to the development of the disease, the following forms of secondary phlegmon are distinguished:
- tonsillogenic (inflammatory process provoked by throat diseases);
- odontogenic (infection enters the soft tissues of the neck from diseased teeth or gums).
Based on the morphological changes occurring in the infected area, the following types of phlegmon are distinguished:
- Serous. This is the initial stage of the pathological process, which is characterized by the absence of a clear boundary between healthy and affected tissues and the formation of exudate.
- Purulent. A purulent exudate forms, the tissues swell, and a fistula may appear.
- Putrid. There is tissue destruction with the formation of gases and an unpleasant odor.
- Necrotic. In the area of inflammation, necrotic foci are formed, followed by tissue rejection. Ulcers may develop.
- Anaerobic. A secondary anaerobic infection joins the inflammatory process.
Cellulitis of newborns is another form of the disease, which is quite rare and develops at 2-3 weeks of a baby’s life. The inflammatory process is preceded by a persistent decrease in immunity. The risk of developing the disease increases if the mother experiences a bacterial infection in the last months of pregnancy.
Reasons for the development of inflammation in the neck
The disease develops as a result of penetration into the fatty tissue through a wound on the neck or through the flow of blood and lymph from other foci of infection. However, the presence of pathogenic microflora in the body does not mean that you will have to deal with phlegmon. Immunity is of great importance. If the body's defenses are working at full strength, bacteria will not be able to fully reproduce.
The following factors can become a trigger for the development of neck phlegmon:
- Diseases of the lower jaw. Foci of infection such as pulpitis, caries, periodontitis, and gingivitis can provoke infection of the soft tissues of the neck.
- Throat infections. People with chronic tracheitis, tonsillitis, pharyngitis, and laryngitis are at risk.
- Inflammation of the lymph nodes.
- Neck injuries. Through scratches and abrasions, the infection can penetrate into the deep layers of the epidermis, provoking a purulent process.
- Any infectious diseases. Pathogenic microflora enters soft tissues through the blood and lymph flow.
In some cases, phlegmon may develop not due to pathological microflora, but due to exposure to chemicals. Thus, purulent inflammation in the subcutaneous tissue of the neck will develop with the introduction of turpentine, gasoline, etc.
Symptoms
The disease in its acute form begins with a sharp increase in body temperature to 39–40 degrees. In this case, the patient has signs of general intoxication of the body:
- headache;
- reduced blood pressure;
- weakness;
- chills;
- thirst;
- sleep disturbance.
With superficial phlegmon, redness and swelling appear in the affected area. When palpating the inflamed area, the patient feels acute pain, and regional lymph nodes become enlarged. Cellulitis may be hard to the touch, and there is a local increase in body temperature (the inflamed area seems hot).
Pain at the gate of the head is one of the signs of the disease.
In deep forms of phlegmon, general symptoms are more pronounced (weakness, fever, headache, etc.). In the early stages, changes in the area of inflammation may not be noticeable. Severe pain is caused by turning the neck. The patient tries to limit his movements. As deep inflammation develops, symptoms also begin to appear in the upper layers of the epidermis. Swelling develops, the skin begins to become shiny.
If purulent masses are present inside the phlegmon, the tumor becomes loose. Pressing on the inflamed area may leave a dent. The pus forms a fistula and begins to come out or spread to neighboring tissues, aggravating the inflammation. As the affected area grows, the patient develops breathing problems due to swelling of the larynx. Body temperature can rise to 42 degrees. There is a serious risk to the patient's life.
Diagnosis of the disease
A qualified surgeon can detect superficial cellulitis during the initial examination. Deep forms of the disease require more careful differential diagnosis . In addition, it is important to identify what pathogen provokes the inflammation in order to prescribe adequate therapy.
A specialist can use the following techniques:
- Palpation of the inflamed area. Changes in the temperature of the affected area, sharp pain, absence of clear boundaries of the tumor - these symptoms indicate the development of phlegmon.
- Patient interview. The doctor clarifies when the first symptoms appeared and what preceded them. It is possible that phlegmon is a complication of a disease of the throat or oral cavity.
- General blood analysis. A change in blood composition may indicate the development of an inflammatory process.
- General urine analysis.
- Ultrasonography. The technique allows you to determine the localization of inflammation in deep forms of the disease.
- MRI of the affected area. The study also helps determine the volume and nature of inflammation. The technique is not used in all clinics due to the high cost of the equipment.
- Puncture of the inflamed area under ultrasound control. The specialist studies the obtained material and determines what pathogen provoked the inflammatory process. In accordance with the information received, medications are selected for antibacterial therapy.
Ultrasound examination of neck phlegmon.
Ultrasound examination has a number of advantages over other methods. In particular, there is the possibility of dynamic monitoring of the process, the possibility of contact between the specialist and the patient during the examination, allows for monitoring of treatment, and provides the possibility of timely controlled puncture of the object under study for the administration of medications or collection of material for research. Ultrasound does not require much time to perform and has no side effects, which emphasizes the promise of this method. Modern Doppler techniques provide the ability to assess the vascular response in the area of detected changes, while the sensitivity of the method reaches 93%. Ultrasound makes it possible to detect infiltrates and fluid accumulations that do not appear clinically in the early stages before the development of a purulent process. Ultrasound criteria for purulent tissue damage are the presence of characteristic changes in the structure of soft tissues - a decrease in their echo density with disruption of the normal anatomical structure, as well as the presence in the soft tissues of a zone of increased echo density with heterogeneous hypoechoic inclusions, as well as gas inclusions. Ultrasound makes it possible to determine the exact localization of the inflammatory focus, its depth and determination of blood flow parameters.
Ultrasound, along with high accuracy in diagnosing inflammatory changes in soft tissues, has other advantages over alternative imaging methods: it does not expose the patient and the doctor to radiation, allows monitoring the object of interest and the process of needle insertion during puncture in real time, and maintains the doctor’s contact and the patient. Ultrasound examination is most comfortable for the patient. The mobility of ultrasound devices makes it possible to use them in an operating room or intensive care unit, when it is impossible to transport the patient, for example, when performing artificial ventilation.
Intern doctor Badyukova A.A.
Treatment of anderophlegmon
The solution to the problem is to carry out complex treatment:
- The purulent focus is opened under local anesthesia or general anesthesia;
- it is being sanitized;
- install drainage without suturing the wound;
- apply a sterile bandage with a mandatory change once a day.
When treating adenophlegmon, antibiotics are used - not only in the form of tablets or injections, but also topically, to wash the abscess cavity. If you seek qualified medical help in a timely manner, the prognosis is favorable. But we must not forget that there is a high risk of developing sepsis.
Information about in what cases adenophlegmon of the floor of the mouth develops and what features of treatment of the disease you need to know is contained on our website https://www.dobrobut.com/.