From this article you will learn:
- methods of treating pulpitis in dentistry,
- how to remove a nerve from a tooth - video, stages of therapy,
- Is it painful to remove a nerve from a tooth?
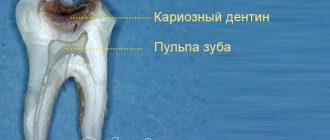
Pulpitis is an inflammation of the neurovascular bundle located inside the tooth, which in dentistry is called the term “dental pulp.” The neurovascular bundle is located in the center of the tooth (in the cavity that dentists call the pulp chamber), as well as in the root canals. Through the tips of the root canals, the vessels and nerves of the pulp anastomose with the vessels and nerves outside the tooth. The name of such a disease as pulpitis arose from a combination of the word “pulp” and the ending “it” (the latter denotes the presence of inflammation).
In an article devoted to the reasons for the development of pulpitis (you can read them at the link above), we have already written that the main reason is long-term dental caries. As a result of the carious process in the hard tissues of the tooth, a carious cavity is formed, the walls of which contain a large amount of infection. When the thickness of healthy tooth tissue separating the pulp from the carious cavity becomes thin, the infection will begin to penetrate into the tooth cavity, causing inflammation of the pulp.
Inflammation of the pulp produces characteristic symptoms – pain. In most cases, treatment will require removal of the inflamed pulp from the tooth cavity and root canals, but in some cases conservative therapy is also possible. The latter is possible only in the early stages of inflammation and in certain groups of patients (we will also discuss this below).
Symptoms of tooth pulpitis -
Pain with pulpitis can be of varying degrees of severity - from minor pain, which is provoked by thermal irritants, to acute paroxysmal spontaneous pain, which makes you want to climb the wall. Given the difference in symptoms, it is customary to distinguish 2 forms of this disease. Below we have described what pulpitis symptoms and treatment will have in each of these cases.
- Acute form of pulpitis – this form is characterized by acute paroxysmal pain that occurs especially at night.
It is typical that the pain increases, while pain-free intervals become shorter and shorter. As a rule, pain occurs spontaneously, i.e. without the participation, for example, of thermal stimuli. However, during the pain-free interval, in some cases it can be provoked by cold or hot water. With pulpitis, it is typical that after the removal of the irritant, the pain persists for about 10-15 minutes (this makes it possible to distinguish pain with pulpitis from pain with deep caries). With the latter, the pain stops immediately after the cessation of exposure to the stimulus. Very often, patients cannot even indicate which tooth exactly hurts, which is due to the irradiation of pain along the nerve trunks. The pain increases due to the gradual transition of inflammation from serous to purulent. With the development of purulent inflammation in the pulp, the pain becomes pulsating, shooting, and pain-free intervals almost completely disappear.
- Chronic form of pulpitis - in this form the inflammation is unexpressed. Patients usually complain of slight aching pain, most often arising from exposure to heat and cold irritants. Sometimes, by the way, with this form of pain there may be no pain at all. Keep in mind that the chronic form of pulpitis can periodically worsen, and during periods of exacerbation of inflammation, the symptoms will be exactly the same as in the acute form.
Symptomatic picture
Symptoms depend on the type of disease. A common feature of all forms is pain. It can be constant or appears mainly during night rest. Depends on temperature stress factors, has an aching or pulsating character. It can be local or spread to the neck, eye, temple, and neighboring units. Chronic inflammation is often painless.
Dentalgia is a nonspecific symptom. It may accompany other dental pathologies. Let's look at how to distinguish pulpitis from caries and periodontitis:
Treatment of tooth pulpitis: methods
Treatment of pulpitis is most often carried out by depulping the tooth. This method involves completely removing the nerve in the tooth, after which the doctor mechanically expands and then fills the root canals. In young patients (provided they apply at an early stage of inflammation), it is possible to carry out treatment while preserving the living pulp of the tooth.
Of course, it is best to leave the nerve alive, because pulpless teeth become more fragile and also change their color to a grayer color. However, in most cases, the use of biological methods for treating pulpitis is impossible, because Patients extremely rarely apply at the very beginning of pulp inflammation (when the first symptoms have just appeared). Age also plays a decisive role in the choice of this method - this method is indicated for use only in people under 25-27 years of age.
Below we will talk in detail about the traditional treatment of pulpitis (read about the conservative method in the link above). By the way, according to official statistics, treatment of pulpitis is carried out poorly in 60-70% of cases, which requires subsequent retreatment of the tooth. This is due to poor-quality root canal filling.
Types of pulpitis and their characteristics
There is no unified classification of the nosological form. Dentists have more than 20 systematizations of this disease. One of the most successful is the typology of E.E. Platonov. What kind of pulpitis happens according to this author:
- Acute focal. The inflammatory process is located inside the coronal zone. Pain occurs after exposure to stressors. Characterized by paroxysmal course. The duration of the attack is no more than 20 minutes. Often occurs during sleep. It is local in nature and does not spread to neighboring structures.
- Acute diffuse. Occurs a few days after the outbreak appears. The process covers the entire coronal zone and proceeds to the root part. The duration of attacks increases to an hour or more. The pain radiates to neighboring areas. The stage lasts about 2 weeks. If you do not start treating the disease during this period, it will become chronic.
- Chronic fibrous. Painful attacks become short-lived and of little intensity. A person feels heaviness and bloating inside the affected segment. Dentalgia appears in response to thermal, chemical, and mechanical stimuli. Percussion of the crown causes pain. The color of the enamel changes. The pulp is replaced by fibrous tissue.
- Chronic gangrenous. Ulcerative-necrotic transformations appear. The process is accompanied by aching pain, the development of halitosis, the unit darkens, the pulp acquires a gray putrid color. The carious cavity is large. The pain is more pronounced if the sinus is closed (due to the accumulation of exudate).
- Exacerbation of chronic inflammation. It is characterized by the appearance of intense pain in the tooth, which can appear spontaneously without the presence of irritants. The attacks are prolonged and cannot be controlled with painkillers.
In the absence of timely consultation with a doctor, inflammation spreads to periodontal structures. In Moscow, periodontitis treatment can be done at the North-Eastern Dental Center on Otradny.
How to remove a nerve from a tooth - video, stages
Removal of the tooth nerve is a classic method of treating pulpitis. Its essence lies in the following steps:
- drilling out all tissues affected by caries (Fig. 2),
- removal of dental pulp (carried out using a special instrument),
- mechanical expansion of channels (Fig. 3),
- filling of tooth root canals (Fig. 4),
- filling the coronal part of the cube (Fig. 5).
Treatment of pulpitis: stages of tooth depulpation
Below we will describe in more detail each stage of treatment for pulpitis; perhaps this information will help you identify a would-be dentist and prevent poor-quality treatment and its complications.
Treatment of pulpitis: video of nerve removal from a tooth
Video 1 clearly shows how the pulp is removed (time - 1 minute 5 seconds), video 2 shows how the canals are mechanically treated with a special endodontic tip, and then they are filled.
Pulpitis in dentistry
Patients in dental clinics are often interested in what pulp is. These are connective tissue fibers that completely fill the natural cavity inside the tooth. It is permeated with sensory receptors and capillaries that support the vital functions of the segment.
At the root apices there are openings through which the neurovascular bundle passes into the periodontium. The pulp tissue located inside the crown is called coronal tissue, the part that is localized in the root canals is called the root tissue.
Algorithm for the treatment of pulpitis using a specific example -
If you have pulpitis, treatment of a single-rooted tooth with one canal is usually carried out in two visits (at the second visit a permanent filling is already placed). In multi-rooted teeth, which have a significantly larger number of canals (from 2 to 4), pulpitis treatment is carried out in 3 visits.
The rule is categorical - a permanent filling on a tooth is not placed in the same visit as the root canal filling, i.e. The filling material in the root canals must first harden (moisture evaporates). Only after this can a permanent filling be placed. But to save time, some dentists neglect this. Below we will look at the algorithm for treating pulpitis of a multi-canal tooth in three visits.
How to diagnose
To diagnose pulpitis, the following manipulations are performed:
- Collecting anamnesis, listening to complaints. The doctor finds out the nature of the pain, the time of its onset, the duration of the attacks, and the connection with irritants.
- Visual inspection (presence of a cavity, filling, change in enamel color, gum condition).
- Percussion. With a limited focus, pain is not felt; other forms are characterized by a pain reaction.
- Probing (always accompanied by unpleasant sensations).
- Testing responses to stressors. The diseased segment responds sharply to cold and heat. The pain does not stop after testing is completed.
- EDI. Indicators for inflammation: 21 - 59 µA.
- X-ray. Allows you to detect hidden caries, dentin destruction, determine the quality of the installed filling, etc.
First visit:
Anesthesia or is it painful to remove a nerve from a tooth?
How painful is it to treat pulpitis: It is definitely very painful if you decide to do it without anesthesia. Fortunately, modern anesthetics can completely solve this problem. If you still feel pain after anesthesia, this may be due to the anesthetic not being strong enough or the anesthesia technique being used incorrectly. The latter usually happens when the doctor tries to anesthetize large molars in the lower jaw (mandibular anesthesia, which is complex in technique, is performed there).
An example of anesthesia (video) –
Drilling out all carious tissues with a drill -
Firstly, at this stage all carious tissue is removed. Secondly, healthy tooth tissues are also partially removed, namely all tooth tissues above the pulp chamber and the mouths of the root canals. This is necessary to ensure visualization of the root canal orifices and ease of their processing with instruments. In Fig. 6-7 you can see the boundaries of excision of hard tooth tissues in the treatment of pulpitis. Figure 8 shows a view of the root canal mouths after they have drilled into the required amount of tooth tissue.
Tooth isolation from saliva –
This is done using a rubber dam. Isolation is necessary to prevent infection from the oral cavity from getting into the root canals along with saliva. This is standard international practice, but in Russia a rubber dam can often be seen only when a doctor fills a tooth.
Removal of pulp from the tooth crown and root canals –
It is carried out with special tools designed to work in canals. In Fig. 9 you can see tooth pulp wound around such a tool. By the way, video 1, which we posted above, shows the process of pulp removal.
Measuring the length of root canals in a tooth –
This is one of the most important stages, because... if the length of each channel is determined incorrectly, it will cause -
- or underfilling of the canals, which will lead to complications after the end of treatment,
- or refilling the canals, which can lead to long-term pain and injury to the mandibular nerve.
Measuring the length of the canals is ideally carried out using a combination of the x-ray method and the use of an “apex locator”. In this case, first, special K-file instruments are introduced into each root canal in turn (Fig. 10), which are connected to the apex locator using a thin electrode (Fig. 12). The K-files are gradually advanced deeper into the root canal until there is a signal on the apex locator screen that the tip of the instrument has reached the apex of the tooth root.
It is necessary to measure each channel in turn, because The length of each channel is unique and there are no exact standards. After the measurements are completed and the data are recorded, K-files are simultaneously inserted into all channels (each to its own depth), and a control x-ray is taken (Fig. 11). The apex locator sometimes makes mistakes, so the x-ray will show how accurately the length of the canal was measured and whether adjustments are needed.
Mechanical processing of channels –
Usually carried out with manual files (K-files or reamers). In Fig. 13 you can see the K-file in the root canal. The dentist rotates this instrument by the handle with his fingertips, and the cutting edges of the instrument excise chips from the walls of the canal, expanding it. The purpose of mechanical treatment is to widen the canal so that later it can be properly filled.
Mechanical processing of each channel is carried out to the depth determined at the previous stage. This is necessary to ensure that each root canal is filled exactly to the root apex. During the expansion process, it is very important to constantly rinse the canals with antiseptics, which is necessary for disinfection, but first of all, to wash out the shavings from the canal (24stoma.ru).
Placing a temporary filling –
After the canals are washed and dried to remove excess moisture, turundas soaked in antiseptic are left in them, and a temporary filling is applied to the tooth. The cost of treatment is calculated based on the number of root canals in the tooth.
Etiology and pathogenesis
Pulpitis is inflammation of the tooth pulp. Pathology accounts for ¼ of all visits to the dentist. The main reason for the development of the pathological process is microbes that penetrate inside through a cavity formed by caries or an incorrectly installed filling. Etiological factors of the disease:
- caries caused by opportunistic microflora of the oral cavity;
- periodontitis (retrograde infection through the opening of the root apex);
- traumatic damage to a segment (crown fracture, root fracture, perforation of the pulp cavity during caries treatment);
- Iatrogenic reasons. Medical errors during treatment: overheating of the pulp, its drying out, prolonged exposure to chemical irritants, etc.;
- idiopathic factors (of unclear etiology).
Second visit:
By the way, it is preferable to fill root canals without anesthesia, but this is not necessary. This is due to the fact that if a slight pain occurs when filling the canals, the doctor immediately understands that he has moved the gutta-percha pin beyond the apex of the root. Accordingly, the doctor can change the filling depth in time.
- Removing a temporary filling.
- Flushing the canals with antiseptics.
- Filling canals using gutta-percha and sealer - after the root canals have been washed and dried, it is necessary to seal them tightly.
This is done using gutta-percha pins of different sizes (Fig. 16) and a sealer (this is something like a paste). The pins are inserted into the root canals and compacted there. In Fig. 14-15 you can see the mouths of the root canals Before and After the canals were filled with gutta-percha. Read more about this stage in our article: → “Mechanical treatment and filling of canals for pulpitis”
- X-ray control of the filling ( required!!! ) if everything is OK on the x-ray, we proceed to the next stage.
But, if we see that the canal is not filled up to the apex, or the gutta-percha pins extend beyond the root into the surrounding tissues, it is necessary to remove all the gutta-percha pins and start filling the canals all over again. In Fig. 17-19 you can see well-sealed root canals (all root canals are sealed to the apex of the root). Unfortunately, it is worth noting that the vast majority of dentists, even if they see that the root canals are filled, do not redo the work. This is precisely what is connected with the percentage of poor-quality treatment of pulpitis that we announced at the beginning of the article (in 60-70% of cases). Type of high-quality filled root canals –
At the end of the visit, a temporary filling is placed, and the patient is warned that the tooth may begin to hurt after undergoing anesthesia. Good tablet analgesics will help relieve pain. A little pain is normal because... during instrumental work in canals, K-files slightly injure the tissue in the area of the root apex.
Table of differences between pulpitis and caries and periodontitis
| Sign | Pulpitis | Caries | Periodontitis |
| Pain during percussion | ++ | — | +++ |
| Pain attacks during night rest | +++ | — | +++ |
| Cold test | +++ | + | — |
| Response to hot stressors | +++ | + | + |
| Unreasonable pain attack | +++ | — | +++ |
| Pain during examination with a probe | +++ | + | — |
| Electroodontodiagnosis, µA | <59 | <21 | >99 |
| Rg diagnostics (presence of changes) | +- | +- | +++ |
“+” - maybe;
“++” - almost always present; “+++” - very strong, always; "-" - absent; “+-” may not exist. The disease can be recognized by its appearance: a darkened tooth indicates the death of the root. When the walls of a segment are destroyed by more than ⅓, a neurovascular formation is almost always involved in the process. In addition to pain, there are: swelling of the mucous membrane, pulp hypertrophy. Prolonged compression of the nerve by tissue leads to its death.
Is it possible not to perform tooth depulpation?
Yes, in the early stages of the development of pulpitis, it is quite possible to treat it without removing the nerve bundle. But to do this, you should go to the doctor at the first signs of the disease, and not wait for it to go away on its own.
If possible, one should try to avoid pulp removal, since teeth without a nerve become more fragile and vulnerable to the action of bacteria and negative external factors. Moreover, in teeth depulped during the treatment of pulpitis, the enamel may lose its natural shine and whiteness.
If a person goes to the clinic for treatment of pulpitis, at a stage when the inflammation has already completely affected the nerve bundle, the nerve of the tooth will have to be removed. The dentist will remove the pulp from the tooth with a special tool, after which he will thoroughly rinse the tooth canals. We will describe in detail how this process works below.
Take a short test and calculate the cost of treatment!
Take a short test
- Which teeth have caries?
- Visual assessment
- Reaction to stimuli
- Cost calculation
×
Manukyan Artavazd Genrikovich
Chief physician of the clinic
Classification of acute pulpitis
Acute pulpitis in modern dentistry is classified according to several criteria. Depending on the cause of development, pulpitis is divided into:
- infectious (bacterial);
- aseptic (chemical, traumatic).
According to clinical and morphological characteristics, acute pulpitis is divided into:
- focal (purulent and serous);
- diffuse (purulent and necrotic).
Depending on the location, root, coronal and total pulpitis are distinguished. According to the possible outcome, acute pulpitis is divided into reversible, in which pulp regeneration is possible, and irreversible.
With the development of acute pulpitis, the exudative stage is of particular importance, which is characterized by increasing swelling, the appearance of serous exudate, transforming into purulent or serous-purulent. With focal purulent pulpitis, inflammation is limited, and with diffuse pulpitis, exudate fills the root and coronal pulp and leads to the development of phlegmon.
How is pulpitis treated?
There are different protocols for eliminating inflammation. The choice of method depends on the form of the pathological process:
- Conservative methods (medication). Characterized by complete preservation of pulp fibers.
- Vital amputation (partial removal). It involves removing the inflamed area of the coronal pulp.
- Vital pulpectomy. Simultaneous invasive total extraction of pulp tissue.
- Devital extirpation. Complete removal of the neurovascular bundle with its preliminary mummification. It is carried out in two stages.
If you consult a dentist in a timely manner, the prognosis for the disease is favorable. Advanced inflammation leads to serious complications. To prevent dental pulpitis, it is necessary to visit a specialist twice a year for a preventive examination and sanitation of the oral cavity.
Recommendations after treatment
To consolidate the result and avoid complications, follow 5 rules:
- Do not eat hard, sweet or sour foods for 2 days. Reduce the chewing load and give preference to soft foods.
- Do not consume tea, coffee, carrots, beets and other coloring foods for 2-3 days. This will lead to staining of the filling.
- Visit a specialist exactly at the time agreed upon during the consultation. You will often need to visit your doctor 2-3 months after surgery to monitor your progress.
- Visit your doctor after 7 days if the pain and burning sensation does not go away. Do not use painkillers - consult a specialist immediately.
- Prevent the development of caries and other diseases. Visit the dentist 2 times a year to eliminate pathologies at an early stage.
The occurrence of pain when eating or brushing teeth within 5-7 days after therapeutic or surgical treatment is normal. If the pain does not go away, visit a specialist.
You can undergo a course of treatment for pulpitis of any form and complexity in the dental department of the CELT clinic!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Why does pulpitis appear: a review of the main reasons
The main causes of pulpitis are:
1. Untreated caries. Carious bacteria little by little destroy first the enamel of the tooth, and then its hard tissues, and over time this process reaches the pulp chamber, where it affects the nerve of the tooth.
2. Low quality of dental treatment. If, when treating caries, the doctor does not properly treat the tooth and its canals, a recurrence of pulpitis is possible. It is for this reason that the choice of dentistry should always be treated with maximum attention!
3. Mistakes made by the doctor when preparing the tooth for prosthetics.
Before prosthetics, the teeth that should support the denture are ground down to the thickness of the future crown. If, when grinding teeth with not removed pulp, the doctor overheats the tissue, pulpitis may develop in the future.
4. Some gum diseases, for example, periodontal disease, can lead to the development of pulpitis. This disease causes tooth roots to become exposed and deep pockets to form where the tooth meets the gum. In such pockets, bacteria actively develop, causing caries and, if left untreated, pulpitis will appear over time.
Another cause of tooth pulpitis can be trauma, which leads to the opening of the pulp and infection.
How to identify pathology in an image
Pulpitis on an x-ray
The parameters by which pulpitis on an x-ray is determined are as follows:
- The presence of an inflammatory process of soft tissue. There will be dark areas visible in the image.
- Deep carious cavity. Destruction that extends beyond the dentin indicates the presence of pulpitis.
- Development of granulomas. Light areas appear in the photo.
- Dental formation. They are neoplasms of dentin or similar tissue, localized in the pulp.