Fibrous pulpitis is one of the types of chronic pulpitis. Its characteristic feature is the excessive growth of connective tissue fibers in the tooth cavity, which ultimately leads to impaired blood supply to the pulp and its death.
Seeking professional help for chronic fibrous pulpitis on time is the key to restoring the appearance and functional characteristics of the tooth. At the same time, an advanced disease can lead to the death of the pulp and the spread of the inflammatory process to the periodontium.
It is worth noting that chronic fibrous pulpitis can develop as a result of the lack of treatment for acute pulpitis, and it can also be a primary process without an acute stage. It can appear and develop on both primary and permanent teeth. Treatment of fibrous pulpitis involves surgery.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 700
- The cost of an orthodontist consultation is 2,000
Make an appointment
Etiology of fibrous pulpitis
The reason for the development of the chronic form of the disease is the opening of the coronal dental cavity during acute fibrous pulpitis
. It is accompanied by the outflow of exudate and some relief for the patient, since the pain that arose during its accumulation will subside. This type of pulpitis is called secondary. As for the primary one, it is an independent form of this pathological condition and develops in a closed tooth cavity. The reasons are a violation of the technique for treating advanced caries (namely, incorrect treatment of the dental cavity, application of a medicinal lining, or mechanical damage to the tooth when opening the pulp chamber).
What can happen if pulpitis is not treated?
Since in some cases the disease occurs without pain, many people put off going to the dentist until the last minute. Do not forget that while you are inactive, the disease progresses. Refusal to treat pulpitis can cause serious complications:
- Flux
- periostitis, a pathological inflammatory process developing from the periosteum.
- Periodontitis
- inflammation of the tissue around the root of the tooth with the possible formation of purulent pockets and destruction of the periapical bone tissue.
- Pulp gangrene
(necrosis) is the death of cells in the internal tissue of the tooth.
- Sepsis
- blood poisoning that develops when microorganisms enter the general bloodstream (usually occurs with reduced immunity).
To avoid such dangerous complications, you need to visit the dentist once every six months. Patients at risk should be examined more frequently (once every three months). The risk group includes patients with diabetes, oncology and other diseases that reduce immunity. If you notice symptoms of caries, go to the doctor immediately.
Forms of fibrous pulpitis
There are two forms of fibrous pulpitis: acute and chronic. Most often, the second occurs as a result of the first; in addition, exacerbations of chronic fibrous pulpitis
.
The chronic form can be called compensation, in which fibrous transformation of the nerve of the tooth occurs with a minimal amount of exudate. The process is characterized by the proliferation of connective tissue fibers in the dental canal and a decrease in the sensitivity of the dental nerve. It arises as a result of the reactivity of the body, which tries to adapt to the ongoing processes by changes in the structure of the pulp. The latter does not disintegrate.
Inflammatory processes of the pulp during this period eliminate acute pain. Most often, this is facilitated by tooth destruction under the influence of carious processes, which creates an outflow of fluid through the hole. Despite the fact that the pain symptoms in the chronic form are not severe, the tooth requires immediate treatment. Very little time will pass - and part of the pulp will die, its necrosis will begin, and purulent inflammatory processes will spread to the tissue around the tooth root. Result? Envelopment of the periosteum, development of flux and (often) tooth extraction.
THE ESSENCE OF THIS PATHOLOGY
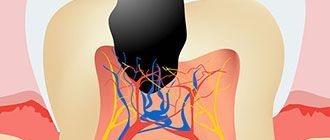
Carious destruction of enamel leads to damage to the underlying dentin - hard tissue penetrated by a system of tubules that are connected to the soft “core” of the tooth. This is the pulp, and it consists of:
- nerves;
- blood vessels;
- lymph nodes;
- connective tissue.
The more enamel and dentin are destroyed, the higher the likelihood of the pathological process transferring to soft tissue. Therefore, the best prevention of caries complications is timely visits to the doctor.
Sluggish chronic inflammation, in which granules form in the tooth cavity, followed by sclerosis and proliferation of connective tissue, is called fibrous pulpitis.
Clinical manifestations
Often this type of pulpitis is practically asymptomatic, which is why the patient does not immediately turn to the dentist. But for most cases the following is typical:
- heaviness in a sore tooth;
- pain reactions in response to irritants;
- nagging pain that intensifies when exposed to irritants and does not go away for a long time;
- bad breath due to poor hygiene;
- the presence of a deep carious cavity with softened dentin inside.
With an exacerbation of the chronic form, pain occurs spontaneously, intensifies at night and spreads to the entire jaw.
It is important to understand that fibrous pulpitis is often detected by a dentist during an examination. This happens when carious cavities are “hidden”: for example, located under the gum. In such places they are inaccessible to irritants, so the patient does not feel severe pain that would force him to seek professional help. One more point must be taken into account: if the carious cavity is combined with the tooth cavity, the patient does not feel such a specific symptom as heaviness in the tooth. Moreover: he does not feel any discomfort at all, and therefore does not seek treatment. And this is very bad, since the lack of treatment will lead to destruction of dental tissue, damage to the periosteum and the development of gumboil, the treatment of which often involves tooth extraction.
Symptoms of chronic pulpitis
Chronic pulpitis affects the dental pulp tissue and is much more common than acute pulpitis (approximately 75 to 25 percent). It can be either an independent (primary) disease or the next stage of an acute one (on average, the transition is noted after 10–12 weeks from the onset of the acute form). There is chronic pulpitis of permanent and primary teeth, and in childhood, if possible, it is recommended to carry out tooth-preserving manipulations in order to minimize the risk of disruption of the development of permanent teeth.
The disease can be almost asymptomatic, therefore, with chronic pulpitis, patients often have no complaints: pain is dull and occurs quite rarely. In contrast to the acute form, in which the pain is usually sharp and pronounced. However, the symptoms of chronic pulpitis are not limited to pain. Therefore, with due attention to the reactions of your body, noticing the problem is not so difficult.
Complaints with chronic pulpitis
- Painful sensations.
If pain manifests itself, it is almost always dull and uniform (has no peak or decline). Exacerbation of chronic pulpitis is characterized by more severe attacks. - Reaction to stimuli.
In most cases, a reaction to a stimulus (for example, cold or hot) occurs only after some time. - Bleeding while eating.
It appears only if granulation formations appear in the pulp.
Diagnostics
Fibrous pulpitis must be differentiated from the following diseases:
- deep caries;
- acute focal pulpitis;
- chronic gangrenous pulpitis.
It is necessary to understand that only a qualified, experienced dentist can make a correct diagnosis after an examination and a series of diagnostic studies. Here are just a few signs that help distinguish one disease from another:
| Symptom | Caries | Focal pulpitis | Gangrenous pulpitis | Fibrous pulpitis |
| Pain | Short-term pain when exposed to irritants of different nature | Severe pain that lasts a long time even after the irritant is eliminated | Long-term painful symptoms of aching nature from irritants of different nature | Aching pain that is mild, moderate pain when exposed to irritants |
| Type of defect | Carious cavity with food fragments and softened dentin inside | Large and deep carious cavity with a large amount of dead dentin | Large and deep carious cavity with a large amount of dead dentin | A large carious cavity filled with destroyed dentin. Violation of the tightness of the dental cavity |
In order to correctly make a diagnosis, the dentist conducts a visual examination of the oral cavity, prescribes radiography and electroodontodiagnostics. The inspection reveals the following:
- severe pain when probing the tooth cavity;
- pulp bleeding;
- severe pain when percussing the tooth;
- reaction to a thermal test.
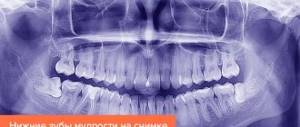
X-ray examination reveals the presence of communication between the carious and dental cavities, and sometimes the expansion of the periodontal gap.
CAUSES AND SYMPTOMS
In most cases, the precursor to this form is acute inflammation of the “nerve” of the tooth, which is accompanied by severe pain. This happens after opening the canal in patients with high body resistance, when pathways appear for the normal outflow of inflammatory exudate.
In young children and patients with low body reactivity, this disease may initially become chronic, without clinical manifestations of the acute stage.
TYPICAL SYMPTOMS:
- aching pain, worse in the evening and at night;
- sharp prolonged reaction to a temperature stimulus;
- feeling of fullness and heaviness in the tooth;
- acute pain when probing the canal.
ACCURATE DIAGNOSTICS
The most important thing is to clearly differentiate fibrous pulpitis from other diseases. In particular, it is distinguished from deep caries by a prolonged pain reaction to external irritation, as well as the absence of spontaneous acute pain radiating to the temple or jaw.
The gangrenous form is characterized by a grayish color of the enamel, a putrid odor, and pain when probing the mouth of the canals. With pathological hypertrophy of the soft tissues of the tooth (another disease in the classification of pulpitis), the patient complains of prolonged pain not associated with irritating factors, and during the examination the doctor sees an overgrown bleeding pulp.
If you use the services of our dentistry, we will perform an accurate differential diagnosis using special research methods. After this, we will select the optimal method of therapy.
Treatment of fibrous pulpitis
As already mentioned, treatment of chronic fibrous pulpitis is carried out using surgical methods. It is aimed at eliminating the source of inflammation, preventing the spread of the disease and restoring the appearance and functionality of the tooth.
One of the methods of treating chronic fibrous pulpitis is vital extirpation, which is performed under local anesthesia. The procedure consists of several stages:
- removal of carious cavity tissues;
- carrying out treatment using antiseptic drugs;
- removal of pulp first from the coronal and then from the root part of the tooth;
- root canal filling;
- tooth filling.
All these manipulations require one visit to the dentist and are considered gentle and physiological. But if the patient has allergic reactions to local anesthetics or root canal obstruction, devital extirpation is required. It is carried out in two steps, in the first of which the pulp is opened and a special paste is applied to it, followed by the installation of a temporary filling. The second measures are carried out after 1–10 days and consist of removing dead pulp, filling canals and teeth. Experienced dentists at the CELT clinic treat fibrous pulpitis, achieving excellent results.
Diagnosis of chronic pulpitis
The disease most often occurs as a complication of caries, when bacteria enter the pulp and cause an inflammatory process in it. However, the penetration of microorganisms is possible with dental injuries, gum disease (through periodontal pockets), as well as with sinusitis and osteomyelitis (much less often). Diagnosis of chronic pulpitis is carried out using a number of techniques that make it possible to accurately determine the form and stage of the disease.
- Visual inspection.
With the help of a dental probe and a mirror, you can almost always notice damage to the teeth and the development of the disease (the exception is chronic pulpitis under a filling). - Radiography.
The most common way to diagnose most dental diseases. - EDI (electroodontodiagnosis).
Use of electrical current to assess the viability of pulpal nerve endings. - Thermometry.
Exposure of the pulp to temperatures to assess its condition.
Clinical researches
Clinical studies have shown that for the effective treatment of chronic localized periodontal disease of traumatic etiology in young patients, a complex of treatment and preventive measures is required, which includes products for individual oral hygiene in the form of treatment and preventive toothpaste "ASEPTA PARODONTAL SENSITIVE" (JSC "VERTEX" , Russia) and mouth rinses "ASEPTA PARODONTAL ACTIVE" and "ASEPTA PARODONTAL FRESH", (JSC "VERTEX", Russia), which allows, within 6 months after completion of complex treatment, not only to improve oral hygiene and 55.37 % reduce inflammatory processes in the gums, but also reduce the number of relapses of localized periodontitis by 21.36%.
Sources:
- Prevention of recurrence of localized periodontitis in young A.K. YORDANISHVILI, Doctor of Medical Sciences, Professor, North-Western State Medical University named after. I.I. Mechnikov, Military Medical Academy named after. CM. Kirov, International Academy of Sciences of Ecology, Human Safety and Nature.
- Clinical studies of antisensitive toothpaste “Asepta Sensitive” (A.A. Leontyev, O.V. Kalinina, S.B. Ulitovsky) A.A. LEONTIEV, dentist O.V. KALININA, dentist S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry, St. Petersburg State Medical University named after. acad. I.P. Pavlova
- Report on clinical trials to determine/confirm the preventive properties of commercially produced personal oral hygiene products: mouth rinse "ASEPTA PARODONTAL" - Solution for irrigator." Doctor of Medical Sciences Professor, Honored Doctor of the Russian Federation, Head. Department of Preventive Dentistry S.B. Ulitovsky, doctor-researcher A.A. Leontiev First St. Petersburg State Medical University named after academician I.P. Pavlova, Department of Preventive Dentistry.
PATHOGENESIS OF THE DISEASE
Hypertrophic pulpitis is a fairly rare type of disease, most often found in young people. As a rule, it occurs in teeth with an open carious cavity. Under the influence of external irritating factors, the process of proliferation—cell multiplication—begins in the pulp (neurovascular bundle). As a result, the pulp chamber is filled with bleeding granulation tissue.
In the absence of timely medical intervention, the disease becomes chronic - a polyp is formed, tightly fused to the underlying tissue.
Acute pulpitis –
Signs of acute pulpitis are reduced to the appearance of acute, paroxysmal pain, spontaneous in nature (i.e., occurring spontaneously, without any irritants). As inflammation transitions from serous-focal to purulent-diffuse, the pain acquires a pulsating, shooting, tearing character, and pain-free intervals disappear until they disappear completely.
According to Platonov’s classification, acute pulpitis should be divided into focal and diffuse forms (Fig. 1-2). Acute focal pulpitis is characteristic of the very beginning of inflammation, when inflammatory changes are present only, for example, in the area of one pulp horn. The rest of the pulp is not yet engulfed in inflammation. Acute diffuse pulpitis - in this case, inflammation covers the entire pulp, both in the coronal part of the tooth and in the root canals (Fig. 2).
Focal and diffuse forms of acute pulpitis –
However, it should be noted here that this division does not have great clinical significance, and it is much more important to subdivide the acute form - not into focal and diffuse, but into acute serous and acute purulent forms. By the way, this is precisely the division proposed by the classification developed by WHO (World Health Organization) specialists.
EXAMINATION OF THE PATIENT
Visual inspection:
The skin of the face and visible part of the neck is of natural color, there is no pronounced asymmetry of the face, there are no scars or sinus tracts on the skin.
Regional lymph nodes (occipital, postauricular, submandibular, submental, facial, cervical, subclavian) are not palpable.
The red border of the lips is bright pink, moisturized, there are no scales, crusts and other lesions, swelling, abrasions, or tears.
Examination of the vestibule of the oral cavity:
The mucous membrane of the vestibule of the oral cavity is pale pink, moist, edema, there are no morphological elements of the lesion.
The depth of the vestibule of the oral cavity is average (7 mm).
The condition and level of attachment of the labial frenulum is within the physiological norm, there are no vestibule cords, there is no blanching or separation of the gums from the necks of the teeth when the lower and upper lips, cheeks, and tongue are abducted.
The bite is orthognathic, there is no crowding or dystopic teeth.
Examination of the oral cavity itself:
The mucous membrane of the hard palate is dark red, moderately moist, and there are no pathological elements. The level of attachment and length of the frenulum of the tongue are within the physiological norm.
| P | |||||||||||||||
| 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| P | P | P | P |
The shape of the dental arches, the shape and size of the teeth correspond to the physiological norm: the position of the teeth in the dentition is not changed, the lateral teeth are pale yellow, the front teeth are dark yellow, there are no changes in the thickness of the enamel, the shine of the enamel is preserved. Mobility of teeth I degree. On the oral surfaces of teeth 12, 11, 21, 22, 34, 33, 32, 31, 41, 42 and 43 there is supragingival and subgingival calculus.