Pulpitis of the wisdom tooth - symptoms and treatment features. Is it worth treating wisdom tooth pulpitis or is it better to remove the figure eight? It is not surprising that debates about the need for early removal of problem teeth still do not subside. However, you should not cut from the shoulder. You can always delete it. In this article, we will discuss the indications for clear removal of a wisdom tooth and its indispensable preservation, if possible.
Wisdom teeth, despite the telling name, do not at all add peace to a person and do not contribute to the development of contemplation. On the contrary, they are nothing but anxiety. At first, they erupt for a long time and painfully, and then they turn out to be incorrectly located, become inflamed and provoke multiple dental complications, even as a result of successful treatment.
What is special about wisdom teeth?
The maximum set of molars for an adult is 32. In this case, it is considered normal to have 28 teeth, since four teeth are the so-called eighth molars or wisdom teeth. For some, they do not erupt at all, for others, when “eights” appear, complications and pathologies arise, but in other cases, wisdom teeth occupy the correct position in the dentition and do not bother their owner. “Eights” usually appear between the ages of 17 and 27, that is, during the period when a person has already formed an attitude towards hygiene and his own dental health. Why is it important? Due to the remote position of wisdom teeth, it is quite difficult to carry out high-quality cleaning, so only very good hygiene can reduce the risk of dental damage. In reality, it is the third molars that are in the top in terms of the number of cases of caries and its common complication - pulpitis.
Prevention of pulpitis
The following rules will help to significantly reduce the risk of pulpitis, but they must be followed carefully:
- Treat all oral diseases in a timely manner, especially caries and gum disease.
- Pay close attention to your overall health and treat any infections as soon as they are identified.
- Brush your teeth well every day, and have your teeth professionally scaled by your dentist as needed.
- Attend routine preventive examinations at the dentist every six months. By the way, such examinations once every 6 months are free of charge.
- Treat your teeth in a reliable, trusted place to minimize medical errors and complications after treatment.
Pulpitis of the wisdom tooth: symptoms and treatment
Pulpitis affects the connective tissue of the tooth - the pulp. It has a crown and a root part: depending on the shape and degree of the disease, one or both parts may be affected. The symptoms of wisdom tooth pulpitis are exactly the same as in the case of other teeth.
- Painful sensations.
In acute pulpitis, the pain is acute and paroxysmal, and can be felt in the temples, ears and other parts of the jaw. The pain intensifies at night and when exposed to irritants (temperature, chemical or mechanical). With chronic pulpitis, the pain is dull and less pronounced, which makes it difficult to diagnose the disease, given the location of the wisdom tooth;
- Bleeding.
It appears only in chronic hypertrophic pulpitis, when granulation tissue grows;
- Change in tooth color.
Observed in the case of tissue necrosis with gangrenous pulpitis.
When a wisdom tooth hurts, pulpitis is just one of the options that could be the cause. To diagnose pulpitis, a visual examination, x-ray or EDI (electrodynamic diagnostics) is required. Of course, such procedures are carried out only by professionals, so if you suspect pulpitis, you should immediately make an appointment with a doctor. Most patients who face a similar problem have two questions: is wisdom tooth pulpitis treated and is it worth treating wisdom tooth pulpitis. The answer to the first question is yes, but to answer the second, you need to consider each clinical case separately.
Causes of inflammation of the dental nerve
Infection in the pulp.
Most often this happens as a result of complications of untreated caries. The carious cavity expands, bacteria penetrate into the pulp and infect it. The infection can also enter the pulp through the apex of the tooth root from deep periodontal pockets with gum disease or through blood from other foci of infection.
Tooth trauma with damage to the pulp chamber, bruxism.
Even a small crack in the tooth enamel can allow bacteria from the oral cavity to penetrate into the pulp and cause inflammation. Therefore, any, even minor, tooth injury requires consultation with a dentist and subsequent observation if there is a suspicion of opening of the pulp chamber. If there is an open pulp, the tooth requires urgent endodontic treatment.
Doctor's mistakes.
Incorrect actions by the dentist can also damage the pulp and provoke inflammation. This may happen if:
- the tooth was treated with too aggressive alcohol or alkaline solutions during treatment,
- the pulp was overheated during the preparation of tooth tissue without sufficient cooling,
- the pulp chamber was damaged due to negligence during the treatment of caries,
- a filling material was used that caused an allergic reaction in the patient.
Pulpitis of the wisdom tooth: treat or remove?
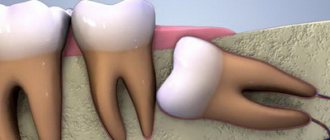
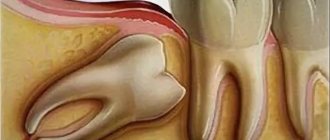
In most cases, a wisdom tooth with pulpitis is removed. The main indications for removing a diseased “eight” are developmental pathologies, as well as being outside the bite (in this case, the tooth has no function). We are talking, first of all, about retention and dystopia. An impacted wisdom tooth is completely or partially hidden in the jaw, and a dystopic wisdom tooth has an incorrect position relative to the rest of the dentition. These pathologies in themselves are a good reason for removing the “eight”, however, if pulpitis occurs due to the impossibility of full treatment, such teeth are definitely removed.
Complications of pulpitis
Untimely treatment of acute pulpitis leads to a chronic process. A hidden infectious focus is formed in the body, which can provoke the appearance of both new dental diseases and general ailments, such as:
- flux - periostitis, purulent inflammation of the periosteum,
- osteomyelitis - inflammation of the bone tissue of the jaw,
- purulent inflammatory processes of intraoral tissues and soft tissues of the face,
- dental cyst - a benign neoplasm near the tips of the roots,
- sepsis - blood poisoning,
- The infection spreads to other organs through the bloodstream, with the heart and kidneys most often affected.
These diseases will require surgical or general systemic treatment - in no case should they be allowed to appear.
Treatment of wisdom tooth pulpitis
Treatment of wisdom tooth pulpitis is carried out in the same way as on other teeth. In 90% of cases, the doctor performs complete removal of the pulp: only in the initial stages of chronic fibrous pulpitis is it possible to save part of the pulp. However, even if the wisdom tooth is positioned correctly and has completely erupted, very often the doctor suggests extraction rather than treatment. This is due to some features of wisdom teeth that reduce the likelihood of a successful treatment outcome.
- Location of position. Wisdom teeth are difficult to reach, and treatment of pulpitis requires almost pinpoint precision.
- Wisdom teeth have curved roots, which sometimes makes the depulpation procedure extremely difficult.
Despite the difficulty of treatment, sometimes preserving wisdom teeth is advisable. First of all, this applies to situations where, of all the molars, only “eights” remain (in the future, a prosthesis can be attached to them), as well as in the initial stages of the disease, when the chances of a successful and predictable result are higher.
Pulpitis in children
Treatment of pulpitis in children follows the same scheme, but there are a number of difficulties here. Firstly, the inflammatory process in the tooth itself occurs very quickly, so it is important to prevent it from spreading to the bone tissue around the tooth. Secondly, a child may experience an allergic reaction to anesthesia during treatment.
Therefore, in the case of children, it will be much easier to initially monitor the condition of the teeth and prevent the occurrence of caries. If your child complains of toothache, you should not put off visiting the dentist. After all, the health of permanent teeth depends on the speed of treatment.
Probably no one wants to get such dental problems. To avoid them, you need to visit the dentist once every six months, have an examination and professional cleaning, eat right, give up bad habits and keep your mouth clean. After all, dental health is only in your hands.
Diagnosis of pulpitis
Correct diagnosis of pulpitis is a primary task for any dentist, since this disease can be confused with caries, trigeminal neuralgia and exacerbation of chronic periodontitis. Each of these diseases is characterized by pain symptoms, so in order for the diagnosis to be correct, it is necessary:
- identify the causes of pain;
- determine the frequency of pain;
- determine the intensity of attacks;
- conduct a visual inspection;
- carry out x-ray diagnostics.
Forms of pulpitis
Speaking about chronic pulpitis, its symptoms have their own characteristics, which depend on the type of disease:
- chronic pulpitis of a simple type is characterized by prolonged painful attacks, regardless of the presence of an irritant;
- gangrenous type The peculiarity of the symptoms of this stage is manifested in the sensitivity of the damaged tooth to temperature changes. Another characteristic feature of this type is pulp bleeding;
- pulpitis of the hypertrophic type. The manifestation of painful sensations in this case is not paroxysmal in nature. However, the affected tooth still reacts to irritants in the form of particulate matter as well as temperature. This type differs from the others in the presence of an overgrown pulp, which occupies almost the entire cavity formed as a result of caries.
Diagnosis of pulpitis is not difficult; this is facilitated by the patient’s description of the problem and visual changes in the tooth. The results of the anamnesis, the results of a visible examination and the reaction to the electrical pulse help significantly. It is advisable to use a comprehensive examination picture, since sometimes even doctors find it difficult to distinguish pulpitis from caries during a visual examination.
Forms of pulpitis are acute and chronic. The difference between the stages is a small amount of time. Acute - a process lasting at least 3 weeks. Chronic forms may not make themselves felt for several months. The main stages of pulpitis can be characterized based on the classification:
- Acute serous - complaints of periodic pain in the tooth. The pain is not regular, but appears in the form of attacks.
- Acute purulent - severe pain. To alleviate the condition, patients often rinse their mouths with cold water.
- Chronic downtime - even a normal meal or elevated temperature can trigger an attack of pain.
- Chronic hypertrophic - often the connective tissue grows, protruding beyond the tooth area. When small pieces of food get in, aching pain occurs.
- Chronic gangrenous - pain is very rare.
Treatment of reversible pulpitis of primary teeth
O. S. Sarysheva pediatric dentist at the Denta Area clinic (Krasnodar)
In practice, pediatric dentists more often encounter not caries, but its complication - reversible or irreversible pulpitis. Reversible pulpitis implies the presence of a pathological process only in the coronal part of the pulp, while the root part remains unchanged.
This article will discuss an algorithm for the treatment of reversible pulpitis of primary teeth using the vital amputation method using mineral trioxide aggregate (MTA).
In the last decade, MTA has been recognized as the best material for the treatment of reversible pulpitis. Preparations based on it are biocompatible, have bactericidal properties (Ph = 12.5), stimulate the formation of a cement-like substance and its adhesion to odontoblasts, and have mineralizing, dentinogenic and osteogenic effects. It must be remembered that some MTA-based preparations stain the tooth crown gray.
Treatment of temporary teeth should be performed efficiently and preferably in one visit. The main goal is to eliminate the risk of complications and the need for re-intervention, so it is important to correctly carry out differential diagnosis.
The following are symptoms characteristic of reversible inflammation of the pulp of primary teeth:
- The patient complains of short-term pain in the area of the causative tooth. Pain occurs only from the action of irritants and has no aftereffect. Sometimes there may be no pain, but parents pay attention to the presence of a carious cavity.
- Upon external examination, there is no change in the configuration of the face, the skin is without pathological changes.
- The gums in the area of the causative tooth are without pathological changes. But when the carious cavity is localized on the approximal surface of the tooth, inflammation of the interdental papilla is possible.
- There are no fistula tracts or scars (signs of fistulous tracts that were previously present).
- There is no mobility of the causative tooth. If physiological root resorption is not expressed, then mobility is a sign of inflammation of the fibers of the periodontal ligament of the tooth, in which case reversible inflammation of the pulp is excluded.
A mandatory research method is visiography. When assessing the resulting image, it is important to determine the location and size of the carious cavity, the presence/absence of communication with the pulp chamber and pathological changes in the periodontium. Determining the stage of physiological root resorption plays a major role in deciding whether to preserve a tooth.
The most indicative sign of reversible pulp inflammation is the presence of spontaneous hemostasis within 4–5 minutes after amputation of the coronal pulp. If hemostasis does not occur within the specified period, this is a sign of inflammation of the root pulp, in which case it should be extirpated.
Methodology for vital amputation of the pulp of temporary teeth:
- Pain relief, isolation of the working field with a rubber dam system.
- Necrectomy with mandatory water cooling, creation of endodontic access.
- Amputation of the pulp with a carbide bur at low speeds to the level of the root canal orifices.
- Medical treatment of the cavity and pulp stump with chlorhexidine bigluconate 2% (a number of authors use sodium hypochlorite for this purpose).
- Spontaneous hemostasis within 4–5 minutes.
- Applying a portion of MTA to the mouths of the canals. In my practice, I use fast-hardening MTA (Rutdent). The hardening time is 10 minutes, so treatment can be carried out in one visit.
- After the MTA has hardened, an insulating gasket of GIC (light-curing ionositol) is applied.
- Restoration with photopolymer composite. In case of a significant defect in the coronal part, the tooth is covered with a standard crown for temporary teeth.
- Grinding, polishing, final correction of the bite after removing the rubber dam system.
Clinical case: treatment of reversible pulpitis of tooth 7.5 in a 7-year-old child with subsequent restoration with composite material
Rice. 1. Tooth 7.5, the carious cavity is located on the occlusal surface. At first glance, the cavity is insignificant in size.
Rice. 2. On the visiogram, you can evaluate the volume of the carious process, the absence of communication between the carious cavity and the pulp chamber, and the absence of pathological changes in periodontal tissues.
Rice. 3. This photo shows the initial stage of preparation. Infected carious dentin is exposed.
Rice. 4. Necrectomy has been performed, the points of opening of the pulp chamber are visible. There is no bleeding from the opening points, which is typical for reversible pulpitis of primary teeth.
Rice. 5. Amputation of the coronal part of the pulp was carried out, treatment with a solution of chlorhexidine bigluconate 2%, spontaneous hemostasis was observed.
Rice. 6. A therapeutic MTA pad is applied to the orifice. A fast-hardening preparation was used, which allows the tooth restoration to be completed during the same visit (hardening time 8–10 minutes).
Rice. 7. The tooth is restored with light-curing material.
- Sarysheva Oksana Sergeevna,pediatric dentist, orthodontist, Russia, Krasnodar
- “Treatment and restoration of primary teeth” M. S. Duggal, M. E. J. Curzon, S. A. Fail, K. J. Toumba, A. J. Robertson.
- "Pediatric Endodontics" Anna B. Fuks, Benjamin Peretz.
Sarysheva OS, Pediatric dentist, orthodontist, Russia, Krasnodar
350088, Krasnodar region, Krasnodar, st. Sormovskaya, 218
Tel.
e-mail:
Treatment of reversible pulpitis of deciduous teeth
Annotation. The article covers the treatment of reversible pulpitis of primary teeth using the method of vital amputation. The information will be useful for novice pediatric dentists.
Annotation. The article covers the treatment of reversible pulpitis of temporary teeth by the method of vital amputation. Information will be useful to beginner dentists.
Key words: reversible pulpitis of primary teeth; vital amputation method; MTA. Key words: reversible pulpitis of temporary teeth; vital amputation method; MTA.
Literature:
Are folk remedies effective?
Out of fear of dentists, some patients make the serious mistake of trying to cure pulpitis on their own and use all kinds of remedies from the collection of folk recipes, all kinds of decoctions, compresses, and tinctures. Let’s say right away that traditional medicine is absolutely useless in the treatment of pulpitis. And in some cases, its use can provoke severe complications.
Inflammation of the pulp is almost always observed against the background of advanced caries. From the tissues affected by it, bacteria gradually penetrate into the pulp chamber and in order to cure pulpitis qualitatively, all layers of enamel and dentin with carious damage should be eliminated. This can be done only in one way - by drilling with a special tool, which is in the arsenal of modern dentistry.
Even worse are those patients who, having read “grandmother’s recipes,” begin to warm up the area of inflammation. Apply warm compresses or even just heating pads to the tooth. But you should know that heating in the case of an active inflammatory process can worsen the situation, but in no way alleviate the patient’s condition! Warming up catalyzes the spread of inflammation and can cause the onset of purulent pulpitis.
In addition, one should take into account the fact that bacteria that provoke inflammation of the pulp are extremely resistant to even the most potent antibiotics. The drugs will not help either slow down the inflammatory process or relieve acute and painful pain. From here we can draw a simple conclusion: it is possible to cure pulpitis only in the dentist’s office. And the sooner you contact a specialist, the higher the chances will be that you can do without pulp removal and preserve the dental nerve.