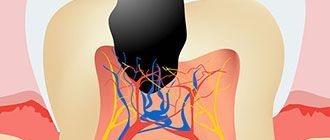
The most severe form of acute pulpitis is diffuse pulpitis
, which occurs if focal pulpitis is not treated.
When it occurs, a focus of inflammation is formed, which after about 48 hours affects the pulp in the crown and root parts of the tooth. Acute diffuse pulpitis
is accompanied by severe pain and can cause inflammation to spread to adjacent teeth.
By its nature, it is similar to a number of other diseases, and therefore requires a full differential diagnosis. It must be distinguished from focal pulpitis in acute form, inflammatory processes of the nerve in chronic form during exacerbation, sinusitis and periodontitis. Only by correctly recognizing this disease can you prescribe adequate treatment. Only an experienced professional dentist can cope with this, and timely seeking help plays an important role in preserving the tooth.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 700
- The cost of an orthodontist consultation is 2,000
Make an appointment
Reasons for the development of diffuse pulpitis
Acute and chronic diffuse pulpitis
develops from focal purulent-serous pulpitis due to the entry of anaerobic bacteria into the pulp. The routes of their penetration can be different:
- deep carious cavity that was not treated;
- incorrect treatment, in which pulpitis developed under the filling material;
- diseases of the body of an infectious nature, in which pathogenic microorganisms enter the dental tissues through the flow of lymph and blood;
- dental tissue injuries;
- violations of the technique of preparing a tooth for a crown;
- periodontitis of adjacent teeth.
Prevention of pulpitis
Some patients ignore toothache that occurs during acute pulpitis (when the necrotic process has not yet developed). This is a big mistake. Consulting a dentist at this stage and carrying out the correct treatment can not only save the tooth, but also prevent dangerous complications. The consequence of pulp necrosis may be:
- inflammation of the periosteum,
- abscess formation
- periodontal tissue infections,
- formation of fistulas, cysts and granulomas,
- the development of systemic diseases caused by bacteria entering the bloodstream: myocarditis, sepsis, brain abscess, glomerulonephritis and rheumatic diseases.
In the prevention of dental pulpitis, the most important thing is oral hygiene. Avoid excessive consumption of sweets and sugar. It is also important to check your teeth every six months by visiting your dentist.
Clinical manifestations
Treatment of diffuse pulpitis
prescribed after the diagnosis has been correctly made, and an important role in this is played by symptoms that make it possible to correctly identify the disease and differentiate it from others. Clinical manifestations of diffuse pulpitis can be divided into two categories: symptoms characteristic of acute pulpitis, and symptoms characteristic of the diffuse form.
| Symptoms of acute pulpitis | Symptoms of diffuse pulpitis |
|
|
In the first 24–48 hours, the patient suffers from pain that occurs without exposure to external stimuli. The “light” intervals between them are quite long, but exposure to cold leads to the development of pain symptoms. As the disease progresses, pain-free intervals become shorter and shorter. Often the pain does not go away completely, but subsides for a while. During such periods, thermal effects cause new attacks, and cold, on the contrary, can calm them down due to the fact that under its influence the blood vessels narrow. The pain radiates to the occipital and temporal region, as well as to the ears. The acute phase can last from 48 hours to 14 days, after which the disease becomes chronic.
Causes of acute pulpitis
Acute dental pulpitis is one of the most common dental diseases, which can lead to morphological changes in the nerve, from minor swelling to complete melting of the cellular elements. The main cause of the development of the inflammatory process is a bacterial infection.
There are several factors that determine the development of pulpitis. All of them are conditionally divided into 2 main groups.
Acute pulpitis resulting from incorrect dental treatment:
- burn of the pulp during preparation of the dental cavity;
- use of potent drugs;
- violation of the marginal seal of the tooth filling.
Acute pulpitis not associated with incorrect dental therapy:
- tooth injury;
- gum disease (periodontitis, gingivitis, periodontal disease);
- pathological abrasion (reduction in the amount of hard tissue) of teeth;
- advanced caries;
- erosive damage to tooth enamel;
- penetration of infection through blood or lymphatic vessels from nearby or distant foci.
Diagnosis of diffuse pulpitis
In order to correctly diagnose, the dentist conducts a visual examination, which reveals the following:
- the presence of a carious cavity;
- painful symptoms on probing;
- painful symptoms (not pronounced) during percussion;
- increased pain when exposed to irritants.
In addition, radiography is prescribed, which reveals the communication of carious and dental cavities, the absence of changes in the periodontium. Electroodontodiagnostics for diffuse pulpitis notes a decrease in electrical excitability along the entire bottom of the carious cavity. As already mentioned, differential diagnosis plays a crucial role, since many symptoms of diffuse pulpitis are similar to the clinical manifestations of other diseases.
| Disease | Similarities with diffuse pulpitis | Differences from diffuse pulpitis | |
| Exacerbation of chronic pulpitis |
| Chronic pulpitis | Diffuse pulpitis |
| recurring pain | pain that lasts from three to fourteen days | ||
| a very deep carious cavity that is separated from the pulp chamber | cavities combined | ||
| pain symptoms along the entire bottom during instrumental examination | intense pain at the point of communication | ||
| X-ray shows no changes | radiography reveals widening of the periodontal fissure | ||
| Acute apical periodontitis |
| Periodontitis | Pulpitis |
| pain increases, intensifies when biting, feeling of an “overgrown tooth”, it is easy to identify the affected tooth | pain occurs in attacks | ||
| the mucous membrane of the gums does not change | swelling and hyperemia of the gums around the affected tooth | ||
| the carious cavity is separated from the pulp chamber | cavities combined | ||
| lymph nodes unchanged | lymph nodes are enlarged | ||
| original tooth color | the crown of the tooth becomes dull or darkened | ||
| painful palpation | palpation does not cause pain | ||
| X-ray shows no changes | radiography reveals widening of the periodontal fissure | ||
| EDI indicators range from 30 to 45 µA | EDI indicators range from 100 μA | ||
| Tapping on a tooth does not produce a strong pain reaction | percussion is very painful | ||
| Trigeminal neuralgia |
| Neuralgia | Pulpitis |
| pain as a reaction to exposure to heat and cold, but without attacks, does not occur at night | pain is paroxysmal and intensifies at night | ||
| absence of vegetative manifestations | redness of the face, dilated pupils, discharge from the nose and mouth | ||
Symptoms of pulpitis
Toothache, typical of reversible, acute inflammation of the pulp, appearing for the first time and lasting less than 2 days, aggravated by eating and drinking (sweet, cold). With chronic inflammation, pain occurs only in the acute phase.
With progressive irreversible inflammatory processes in the pulp with extensive necrotic foci, the following “painful” signs appear:
- The pain occurs on its own, lasts continuously for 2 - 3 days, and has a pulsating character.
- Night toothache (worsening when a person takes a horizontal position).
- discomfort when biting food or tapping.
- The pain radiates to the temple or eye, and when there is a problem tooth in the lower jaw, to the back of the head, neck and ear.
However, it should be remembered that inflammation of the dental pulp can also be asymptomatic. In addition, the symptoms characteristic of pulpitis are also inherent in other diseases, so diagnosing pulp inflammation is not easy. Acute inflammation leads to chronic inflammation of the periapical tissues of the teeth and changes in the alveolar process. Sometimes chronic periapical inflammation occurs asymptomatically, and periapical dental lesions are detected using radiography.
Treatment methods
Treatment of acute diffuse pulpitis
is aimed at eliminating pain symptoms and getting rid of the source of the inflammatory process. It allows you to prevent the spread of the disease, eliminate the development of acute periodontitis and restore tooth function. Treatment methods are surgical, there are two of them:
- Vital extirpation is carried out in one step and consists of removing pulp from the crown and root parts of the tooth under anesthesia. After the extraction, the dentist fills the root canals and places a filling on the tooth.
- Devital extirpation requires two visits to the doctor, on the first of which he applies a special paste to the pulp, which kills it, and on the second, he removes it.
The CELT clinic successfully treats pulpitis of varying complexity, but the sooner the patient seeks professional help, the greater the chance that it will be possible to restore the shape of the tooth and its normal functioning.
Diagnosis of acute pulpitis
Diagnosis of acute pulpitis is not particularly difficult. At the first stage, a dental examination of the oral cavity is carried out, including examination of the teeth and mucous membrane of the gums. The dentist also pays attention to the presence of hyperemia and swelling, as well as changes in the submandibular lymph nodes.
Instrumental diagnosis of pulpitis includes:
- temperature test (tooth irritation with a swab soaked in hot or cold water);
- X-ray of the tooth (allows you to identify a hidden carious cavity);
- electroodontodiagnosis (determining the electrical excitability of teeth with formed roots).
In parallel, special diagnostics are carried out to differentiate acute focal pulpitis from other dental pathologies.
Why does pulpitis develop?
The most common cause is deep caries. As the carious cavity deepens, it causes microbes to penetrate into the pulp tissue. The infection can get directly to the pulp (direct penetration) or through the dental tubules in the thickness of the dentin.
Infection of the pulp and the occurrence of pulpitis can occur: through the dental crown (as a complication of caries), through the open apex of the root (retrograde pulpitis).
- The result of postponing a visit to the doctor may be the transition of pulpitis to periodontitis, and this is a more complex disease.
- Pathogenic microorganisms multiply quickly in carious cavities and under poorly installed fillings. The result of their vital activity is the main cause of pulpitis.
- The onset of the inflammatory process occurs in the infected area, from where pathogenic microflora enters the root pulp.
- For traumatic injuries (fractures and chipped teeth).
- When exposed to chemical and temperature factors.
In many cases, a diseased tooth has to be removed and resulting in displacement of neighboring teeth, malocclusion, and intestinal and stomach diseases.
After prolonged pain caused by pulpitis, gumboil may appear when the nerve dies and pus forms in the canal. In turn, the flux can turn into a fistula.