Implantation immediately after removal of a tooth with a cyst
Installing an artificial root immediately after removing a natural tooth with a cyst is considered an experimental technology. Surgery with a guarantee does not provide for the possibility of conducting such experiments. Installation of an implant after removal of a tooth with a cyst is only available if there are verified and confirmed positive long-term results of therapy.
Classic technology provides for implantation only after a certain period, when the specialist is confident that there is no source of infection. The process of bone restoration and healing of the injured area in most cases takes about 60-90 days. The duration of the period depends on the size of the cyst and the characteristics of the specific defect.
How can you insert implants instead of extracted teeth?
At the initial appointment, the doctor examines the patient, collects anamnesis, and issues a referral for laboratory and instrumental diagnostics. It is necessary to take blood tests, urine tests, x-rays or computed tomography. The second method is more informative, as it allows you to consider the structural features of the dental system in a 3D image.
After eliminating contraindications, the dentist sets a day for surgery. Pain relief is carried out using local anesthetics. If the patient has a panicky fear of dental procedures, treatment during sleep and other methods of anesthesia are possible.
During the operation, the doctor removes the diseased dental unit, drills a bed into the bone and screws in the implant.
Several techniques are used:
- Placement of a two-piece implant into the bone followed by suturing of the gums. After engraftment, the procedure for forming the gum margin and prosthetics is carried out.
- A healing abutment can be placed along with the screw. Sutures are also placed on soft tissues. When the gingival margin becomes smooth, the crown is fixed.
- Immediately after removal, an abutment is installed and a temporary plastic prosthesis is placed on it. No suturing of gum tissue is required.
During prosthetics, the crown is screwed, secured with cement, or snapped onto the structure's rod, depending on the type of abutment. The entire procedure can take up to three hours. On the day of the operation, the patient needs rest, so you must first arrange a day off from work.
In what cases is simultaneous implantation possible?
The method of express installation of implants is available to adult patients. Indications for such implantation are:
- mechanical damage to the root;
- chronic periodontitis, which provoked complete or partial destruction of the crown;
- different stages of periodontitis;
- broken tooth;
- lack of results with conservative treatment of chronic periodontitis;
- tooth extraction before installing a prosthesis.
The final decision on the possibility of express implantation is made by a specialist, taking into account the clinical picture and features of the removal procedure. The level of tissue damage, the method of tooth extraction and the presence of complications after surgery are of great importance.
Implantation after removal of a tooth with a cyst is possible after complete restoration of bone tissue.
Experienced implant surgeon Svetlana Stepanovna Fr.
Treatment of pathology
Treatment of the cyst must begin immediately after its discovery. The only high-quality treatment method is surgical removal of the cyst.
Modern dentistry offers the possibility of treating cysts using therapeutic methods. However, this technique can only be used in the early stages of the disease. The method is rarely used, since the cyst is more often found in severe forms.
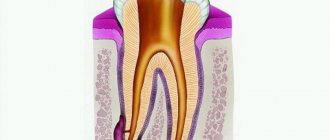
The essence of surgical treatment is to cleanse the cyst cavity and introduce absorbable drugs into it. This method is quite complicated to perform, so during education, dentists often perform removal in the following ways:
- Hemisection is a procedure when, along with cleansing the cyst cavity, the tooth root and damaged part of the soft tissue are removed.
- Cystotomy is a procedure that involves separating a partial cyst membrane. In this case, the contents of the cavity are removed, and the remaining part resolves on its own.
- Cystectomy is the simultaneous removal of the entire cyst and part of the damaged tooth.
Procedures for removing a cyst without damaging the integrity of the tooth are carried out only when the size of the cyst is insignificant and there are no complications. In other cases, dentists resort to removing the entire tooth.
Restoring a tooth with an implant is possible only after a full course of jaw therapy and elimination of the infectious process in the soft tissues. In severe cases, treatment of the cyst lasts up to six months.
Implant installation and the presence of a cyst on an adjacent tooth
Implantation of an artificial root in the presence of any inflammation in the oral cavity is unacceptable. The presence of a cyst on the root of a nearby tooth significantly increases the likelihood of an exacerbation, which negatively affects the stability of the implant.
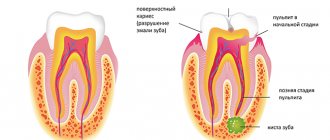
This dental pathology is the result of the body’s reaction to damage or infection. A cyst is a round formation with purulent contents or liquid inside. The boundaries of the focus of the inflammatory process are quite clear, so nearby tissues are not affected.
The cyst forms at the top of the root; its diameter can be several centimeters. Such formations are divided into several varieties, differing in the reasons for their appearance:
- Eruption cyst - appears when milk teeth are replaced by molars.
- Odontogenic or radicular - occurs most often as a result of the appearance of serious defects and untimely consultation with a doctor.
- Keratocyst is the result of a violation of the formation of an element of the dentition with preservation of the os-forming tissue at the stage of intrauterine development.
- Residual - appears inside the bone as a result of problematic tooth extraction.
Installation of an implant is possible after treatment, as well as bone growth or improvement of its quality.
General overview
The root cause of cyst formation is the negative impact of the inflammatory process to which the human body reacts. The capsule, formed from connective tissue, prevents the rapid spread of infection to adjacent areas. At the same time, an infected mass containing purulent discharge and dead cells accumulates inside the cavity.
In situations where the size of the cyst does not provoke pain, the only sign of pathology is inflammation and redness of the gums in the affected area. However, over time, the symptoms become more pronounced, characterized not only by discomfort and pain during loads on the jaw, but also by an increase in body temperature.
A timely visit to the dentist allows you to avoid a number of complications that can be caused by a dental cyst:
- Formation of a purulent fistula caused by a breakthrough of the cavity;
- Spread of the inflammatory process to the paranasal sinuses;
- Development of periostitis or osteomyelitis;
- Formation of pathological cavities in the mucous membranes;
- Formation of phlegmon due to inflammation of fatty tissue;
- With significant damage to bone tissue - jaw fracture;
- When an infection enters the circulatory system, it becomes a general infection of the body.
A comprehensive clinical examination helps to identify pathology and draw up a competent treatment plan that eliminates negative consequences for the patient’s body.
Treatment is performed in one of the following ways:
- complete cleaning of the dental canal with further cementation;
- cystectomy (removal of a large cyst along with the affected upper part of the root);
- tooth extraction (used for complete destruction of tooth tissue);
- depophoresis (allows you to stop the source of the problem in the root canals);
- hemisection (used in case of root destruction).
Opinion of implantologist Ivan Arkadyevich: “A significant lack of bone tissue as a result of the development of a periodontal or root cyst makes the use of express technologies impossible. This problem requires a responsible attitude even after the formation is removed. Otherwise, implantation will not be effective. Installation of an artificial root is possible only after complete healing of the wound and removal of the sutures.”
Content:
- Why does retention occur?
- Classification of impacted teeth
- Is it necessary to remove an impacted tooth?
- How impacted units are removed
- Recovery after removal of an impacted tooth
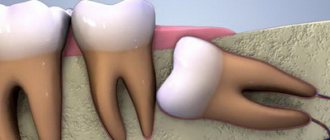
Retained are units that cannot independently erupt and take the place allocated for them.
They remain inside the jaw bone or are located directly under the soft tissues, mucous membranes of the oral cavity. Removing an impacted tooth is a complex operation for which doctors always prepare in advance. It is not carried out on an emergency basis.
Cyst in the area of implanted titanium root
The development of a neoplasm occurs as a result of damage or an inflammatory process in the area of the natural tooth root. The implant is an artificial element made of a special alloy. Medical titanium is biocompatible with jaw tissue and does not provoke allergic reactions. The procedure is carried out in complete sterility, and therefore the likelihood of infection is almost eliminated. The formation of a cyst in the artificial root area is considered impossible.
Treatment of cysts and other defects of the bone tissue of the jaws is a pressing problem in surgical dentistry and maxillofacial surgery (maxillofacial surgery). The frequency of cyst development corresponds to a high level of dental caries damage (in the adult population - up to 90%). X-ray examination of patients very often reveals cysts and destructive apical processes that occur without clinical symptoms or inflammatory processes, the causes of which are odontogenic cysts of the jaws [4].
A unique feature of the clinical case considered in the article is that the retention of the 21st tooth was caused by 3 supernumerary teeth located on the eruption path of the 21st tooth, incorrect horizontal anlage of the 21st tooth in the jaw and subsequently the development of a follicular cyst of the alveolar process of the upper jaw ( HF). The cyst, increasing in size, caused significant deformation of the HF and a cosmetic defect on the face of patient O.
The cause of impaired growth and formation of the dentoalveolar arch is a delay in the eruption of permanent teeth, which is most often observed in the anterior section of the HF. Delayed tooth eruption is called retention, and a formed tooth located in the jaw and not erupted within 2 years after the normal eruption period is called impacted [1-3].
Supernumerary teeth, localized in the area of the upper central incisors, can cause retention of permanent teeth, as well as displacement of adjacent teeth, curvature of their roots, and the formation of a follicular cyst. Tooth retention can be caused by endocrine disorders, supernumerary teeth located on the path of tooth eruption, improper placement in the jaw, atypical tooth structure, delayed replacement of primary teeth, underdevelopment of the alveolar process, inflammatory processes and jaw trauma [1].
We give an example of surgical treatment of a follicular cyst of the HF, the cause of which was supernumerary teeth and the horizontal position of the 21st tooth, its complete retention.
Patient O., born in 1993, conscript soldier of military unit 30616-23, was admitted to the Department of Maxillary Surgery and Dentistry of Branch No. 4 of the Main Military Clinical Hospital (GVKG) named after. N.N. Burdenko with complaints of a cosmetic defect and asymmetry of the face on the left, a tumor-like formation in the area of the alveolar process of the HF on the left and the absence of the 21st tooth. From the anamnesis: the disease was asymptomatic; before being called up for service in the RF Armed Forces, he was treated by a dentist in a clinic at his place of residence, where in the winter of 2011 the primary left central incisor was removed, since this tooth, according to the patient, “was loose and began to hurt when biting." The dentist did not conduct an X-ray examination of the alveolar process of the HF in patient O. After being called up to serve in the RF Armed Forces in February 2013, colleagues drew attention to the facial asymmetry of patient O. With the above complaints, he was admitted as planned for examination, clarification of the diagnosis and surgical treatment at the Department of Maxillary Surgery and Dentistry of Branch No. 4 of the State Military Clinical Hospital named after. N.N. Burdenko. When examining the patient O. objectively: the face is sharply asymmetrical due to a formation measuring 3.5×3.0 cm, dense and painless on palpation, in the area of the alveolar process of the left maxillary sinus and the anterior wall of the left maxillary sinus, spreading upward to the left lacrimal bone. The skin over the formation is not changed in color, easily folds, without signs of inflammation. The nasolabial fold on the left is smoothed (Fig. 1).
Figure 1. Appearance of patient O. before surgery.
The formation bulges into the oral cavity in the area of the socket of the removed primary central incisor and is identified by palpation above the crown of the right permanent central incisor. The mucous membrane of the oral cavity above the formation is not changed in color, without signs of inflammation. The 12, 11, 22, 23rd teeth are intact, their percussion is painless, motionless on palpation (Fig. 2).
Figure 2. View of the alveolar process of the HF before surgery.
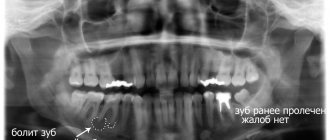
In the hospital, patient O. underwent examination: orthopantomography (OPMG), high-frequency computed tomography (CT), radiography of the paranasal sinuses, consultation with an ENT doctor. On the OPMG of patient O., in the area of the alveolar process of the HF on the left, under the bottom of the left maxillary sinus, the 21st tooth is located horizontally, below it there are 3 supernumerary tooth germs, around which a cystic cavity measuring 2.3 × 3.6 cm with clear contours is formed . The roots of the 11th and 22nd teeth border the cyst shell. There is an inclination of the root of the 22nd tooth along the axis with a deviation of the upper third laterally, the angle of deviation is 70° (Fig. 3).
Figure 3. OPMG of patient O. On a series of computed tomograms performed according to a standard program, in the HF projection on the left, the presence of retention of the 21st tooth and the formation of an oval-shaped follicular cyst with clear, even contours, measuring 36.9 × 22.4 × 16, are noted. 5 mm. The cyst has a thin bone shell and heterogeneous contents of liquid density (4-18 HU units). The cyst is located in the area of the anterior wall of the left maxillary sinus. CT conclusion: signs of a follicular cyst of the left HF.
An X-ray of the paranasal sinuses revealed no pathological changes. Patient O. was examined by an ENT doctor, the conclusion was that the ENT organs were without visible pathology. Based on complaints, anamnesis, clinical manifestations and objective examination data, patient O. was diagnosed with follicular cyst of the alveolar process of the left HF; retention of the 21st tooth. Patient O. was offered the following treatment plan: 1) surgery - cystectomy and removal of supernumerary teeth, impacted 21st tooth; 2) filling the bone defect with artificial bone in an amount of 2 g.
As preoperative preparation, depulpation of the 11th and 22nd teeth was performed on the day of surgery, followed by filling the root canals with phosphate cement. The operation was performed under general anesthesia with a 2% ultracaine solution using the Parch II method.
During the operation, a cyst with a shell, 3 rudiments of supernumerary teeth and an impacted 21st tooth were removed (Fig. 4, 5).
Figure 4. Stage of surgical treatment of patient O.
Figure 5. Extracted supernumerary teeth of patient O. During the operation it was revealed that the follicular cyst destroyed the anterior wall of the left maxillary sinus and a bone defect measuring 1.0×1.0 cm was formed; the integrity of the sinus mucosa was not compromised. The cyst did not grow into the maxillary sinus. A hemostatic sponge measuring 1.3×1.3 cm was applied to the anterior wall of the left maxillary sinus at the site of the bone defect. The bone defect was filled with artificial bone granules (2 g) with lincomycin. In the postoperative period, the patient received antibacterial and analgesic therapy intramuscularly, and rinsed the mouth with local antiseptic solutions. The early postoperative period proceeded without complications. The sutures were removed on the 10th day. The wound in the mouth healed by primary intention. The case under consideration is interesting in that patient O. developed a complication in the late postoperative period - rejection of artificial bone, associated with the individual characteristics of the reactivity and immunity of the body of a particular patient. Clinically, this was manifested by an increase in swelling of the soft tissues of the face in the area of the upper lip and nasolabial fold on the left. There were no signs of wound suppuration. The general condition and body temperature of patient O. were normal throughout the entire postoperative period, and a clinical blood test showed no pathology or signs of an inflammatory reaction. In this case, it was necessary to make an incision of the mucous membrane up to 1 cm long under local anesthesia along the postoperative scar in the area of the socket of the missing 21st tooth and partially remove the artificial bone with a curettage spoon. Further wound management was carried out under iodoform turunda. The wound healed by secondary intention. Patient O. was discharged to the unit at the place of service with recovery and the following recommendations: 1) dynamic observation of the dentist at the place of service; 2) re-hospitalization to the department of maxillofacial surgery and dentistry after 6 months to check the long-term results of treatment and prosthetics of the frontal part of the mouth.
Our many years of experience in using granules of osteoplastic materials to fill bone defects in the treatment of odontogenic cysts of the jaws still allows us to state that complications in the form of material rejection are rare, in isolated cases, and are associated with the individual characteristics of the patient’s body. In most cases, the postoperative period proceeds favorably. Thus, over the past period of 2013, the department performed 7 operations for odontogenic cysts of the jaws using artificial bone, and only in 1 case, in patient O., a complication arose in the form of material rejection.
Thus, when drawing up a treatment plan for patients with follicular cysts, one should take into account the main reasons for the development of this pathology of the dental system, the position of the impacted tooth, the possibility of its preservation and eruption in the process of self-regulation in childhood and young age, and at a later age - the need for orthodontic treatment. But if it is impossible to save an impacted tooth due to its atypical position in the alveolar process of the jaw, as well as due to the presence of supernumerary tooth rudiments that prevent its eruption, it is necessary to remove the supernumerary teeth and impacted tooth, perform a cystectomy or cystotomy.
Recently, the method of surgical treatment of jaw cysts has not changed. The most widely used in clinical practice is cystectomy with the simultaneous filling of the bone defect of the jaws with osteoplastic materials, providing: prevention of secondary infection associated with the reduction of a blood clot or its resorption, restoration of bone tissue; rapid functional rehabilitation [4]. In our department, Kollapan is used for this purpose. Experience with the use of this drug allows us to recommend it for introduction into widespread clinical practice. The collapan is completely replaced by newly formed bone tissue, retains antimicrobial activity in the wound for up to 20 days, during which the antibiotic is uniformly released and does not cause suppuration.
The presence of antimicrobial agents of different spectrum of action in Kollapan allows you to purposefully select the type of Kollapan that corresponds to the causative agent of the disease, which significantly increases the effectiveness of treatment. The choice of Kollapan in the form of granules, plates or gel is due to the convenience of filling bone defects of various shapes and locations. The cost of this material is significantly lower than the cost of other osteoplastic materials (Russia, Moscow, Varshavskoe shosse, building 125. Certificate of conformity No. ROSS RLME77 H00250. No. 1033891 from December 25, 2012 to December 25, 2015).
On radiographs after 1 month, a homogeneous light area is determined, evenly occupying the entire area of the defect; after 3 months, the bone defect is filled with a network of trabeculae. After 6 months, the bone defect was filled with trabeculae, unevenly occupying the entire bone cavity [4].
Thus, the use of Kollapan in the treatment of follicular cysts of the jaws stimulates the processes of reparative osteogenesis and allows for functional and aesthetic rehabilitation of patients as early as possible.
Classification of impacted teeth
Taking into account how deep the unit is under the gum tissue, retention is usually classified into:
- partial (part of the impacted crown rises above the surface of the gum and is clearly visible to the naked eye);
- complete (the entire crown is covered by gingival tissue or is located deep in the jaw bone).
Doctors also take into account where the tooth is located. If in bone tissue, then they speak of retention with immersion, if above it - without immersion.
Impacted dystopic molars, incisors, and canines are also found. They grow out of place or at the wrong angles. Then there is a significant displacement of the dental axis.
Why does retention occur?
Most often, wisdom teeth cannot fully erupt. This is due to the peculiarities of their location. In the process of evolution, eights have lost their meaning. Some people don't have them at all. In others, they often “sit” under the gum and contribute to the displacement of neighboring units, which causes the bite to change.
Retention is caused by:
- heredity;
- premature removal of baby teeth, which leaves little room for constant sweat;
- excessively thick gum walls (very rare);
- malocclusion, severe crowding.