Modern dentistry is one of the most highly developed areas of medicine. Unfortunately, many people are afraid to visit dental offices, fearing the pain they will experience during the procedures.
This stereotype should be dispelled as quickly as possible, since medicine has long stepped forward. Currently, doctors use modern and high-quality equipment, which reduces the risk of pain during dental treatment.
Additive Manufacturing Magazine
Dentistry is perhaps one of the most conservative areas in medicine in terms of the use of new technologies. Especially when it comes to the use of additive technologies (AM).
Where can new technologies be used?
Medicine and dentistry together account for 17% of the total AM market. Projected revenues from the use of AM in medicine will be more than $3.1 billion by 2020 and more than $5.0 billion in 2021, mainly due to investments in the United States and Western Europe. At the same time, one third comes from dentistry, and the rest of the income is in approximately equal shares for the production of prosthetics and medical devices, for the creation of new products and printing prototypes. The greatest growth in AM, by approximately 20% per year, is expected in orthopedics (creation of individual templates for surgeons, implants for the knee joint and for the spine). With the creation of new 3D printers and materials for them, as well as the reduction in prices for printing services, many new applications of AM in medicine are expected to emerge. Therefore, medicine is seen as one of the fastest growing applications for AM with high growth potential. In this article we will discuss 3D printing equipment, biocompatible materials, software for dental laboratories, training issues and surgical planning. Let us give examples of successful applications of AM in dentistry and existing limitations on materials for restorations. Several important factors (referred to as the “four M's”, Figure 1)—market and technology, materials, and metrology—must also be considered to achieve the desired functionality through the selection of predictable and repeatable AM technology. In this case, materials and metrology are decisive.
Rice. 1. Determining factors for AM - 4 M
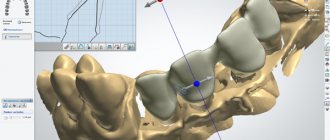
With the advent of AM, it became possible to use them for various applications: directly for the manufacture of restorations, models for casting, for the manufacture of auxiliary elements such as templates and surgical guides, for maxillofacial prosthetics, the manufacture of removable dentures and implants, for planning operations, widespread use in orthodontics . Naturally, dentistry has long used digital methods in the form of CAD/CAM systems. The most complete solutions for the problems of traditional practical dentistry are offered by several well-known companies: - Dentsply Sirona [1] with a set of equipment for scanning individual teeth, preparing a working file and manufacturing finished restorations from zirconium dioxide, ceramics, metal-ceramics using Cerec installations (CNC equipment), metal alloys with their installation during one patient visit. In the Russian Federation and the CIS, almost the entire market belonged to the company's products: scanners, processing programs and CEREC processing centers. A small share was accounted for by scanners and systems for preparing solutions for dentists from 3Shape (Denmark) and DentalWings (Canada): - 3Shape: scanners and software for dentistry, including intraoral scanners. — Dental Wings (Canada): approximately the same set of equipment and software.
AM technologies have added new capabilities: - printing wax models on a Solidscape 3D printer (Prod-ways, France - USA) with subsequent metal casting of individual restorations or bridges; — production of plastic high-precision templates for implant installation; — production of transparent overlay bracket systems in orthodontics, including as a service (Invisalign company, USA); — production of templates for modeling and training.
Basic requirements: - biocompatibility of materials that have contact with the human body (metal alloys, ceramics, plastics); — long-term resistance of materials to aggressive environments in the oral cavity; — high mechanical properties of prosthetic materials, not inferior to natural tooth material; — manufacturability and high speed of production of restorations.
Global healthcare costs will reach $8.7 trillion
The share of people over 65 years of age (the main population for medicine) will increase to 11.5%. In the United States alone, dental and orthodontic laboratories provide services to more than 190,000 dentists. And almost all hospitals have centralized AM departments. The growth in the use of AM in medicine in 2021 was 21%, the share of AM in annual income was 11%. In 2021, the FDA (Food and Drug Administration, USA) issued guidance on the use of medical devices manufactured using AM (Technical Consi-derations for Additive Manufactured Medical Devices December 5, 2017). In addition, the FDA has issued several regulatory documents on the use of AM in regenerative medicine (including human tissues, cells, etc.), as well as on the requirements for the operation of AM departments in hospitals [2]. Materialize and Form-lab have agreed to collaborate to provide hospitals with a complete, cost-effective and easy-to-use solution for running their 3D laboratory. It is considered as a kind of basic standard and includes Mimics inPrint software, which allows you to work with visual information, and the Form 2 3D printer from Formlab [3] for printing surgical templates. The source information can be obtained using the 3Shape TRIOS intraoral scanner, processed in the 3Shape Implant Studio software and then printed on a Form 2 3D printer using biocompatible Dental SG resin [4] within one day. Materialize and Siemens Healthineers have signed a partnership agreement under which Materialize Mimics inPrint software will be included in the open Siemens Healthineers syngo platform. The new product, using virtual 3D models, will allow for closer collaboration in surgical planning between teams of radiologists and surgeons [5]. Philips announced a collaboration with 3D Systems and Stratasys to develop clinical 3D models using the IntelliSpace Portal 10 program, followed by printing on partner 3D printers [6]. The concept of digital workflow (digital workflow) includes three phases: - obtaining information using various scanning technologies; — data processing using CAD programs; — production of a product using CAM systems or AM from a selected material.
About 3D scanning in dentistry [7]
3D scanning technologies are needed to convert physical models into CAD files for subsequent modeling and manufacturing of individual elements (teeth, crowns, braces, gums, veneers and templates) using AM (Table 1). Their advantages: - quick acquisition of information and its processing, - comfort for the patient, - minimum expenditure of time and money, - effective planning of the procedure and its simplification, - better communications, - in-depth training, - overview of the structure of teeth from different angles. Of the many existing scanning methods in dentistry (17% share), methods based on: - X-ray radiation, - optical, - computed tomography, - laser scanning, - ultrasound, - magnetic resonance imaging (MRI) are used.
The main players in the market for the production of equipment and materials for dentistry
Printing from light-curing polymers: Carbon3D (USA), FormLab (USA), Envisiontec (Germany - USA), Prodways (France), Planmeca Oy (Finland), Shining 3D (China), Stratasys (USA), Digital Wax System (Italy) , Roland DGA (USA), Invisalign (USA), 3D Systems; 1. Metal printing: EOS (Germany), Concept Laser (Germany - USA), Renishaw and Bio-Horizons (UK). 2. Ceramic printing: Porimy 3D Printing Technology Co (China). 3. Printing of biomaterials: En-visiontec (Germany - USA). 4. Printing (FDM) from thermoplastics: Arfona (USA). Carbon is engaging major manufacturers of dental materials to jointly develop and further produce materials for mass AM production of products on Carbon 3D printers. Thus, the Whip Mix company (USA) has developed a biocompatible material for AM production of surgical templates for drilling (Fig. 2). Transparent resin is an ideal material for the rapid production of high-precision surgical guides.
Rice. 2. Surgical template for implant installation made from biocompatible material Whip Mix
Two other photopolymer materials from DENTCA: DENTCA Denture Base II and DENTCA Denture Teeth are biocompatible materials with strength characteristics close to traditional acrylic.
FotoDent material (DREVE company) is used to create a gum mask. The opaque pink material remains soft and flexible. For example, dental resin type DPR10 allows Carbon 3D printers to produce accurate, high-quality models for dentists 10 times faster than existing methods. To do this, it was necessary to solve several problems: a long product manufacturing cycle, the complexity of equipment, software and their use (users need ease of launching work and an intuitive interface), poor service and technical support. Carbon successfully solves all these problems (Fig. 3, 4): — maintaining equipment and software in an updated state by supplying equipment by subscription (on an “all-inclusive” basis), providing support via the Internet and from technical partners; — due to the integration of the software with existing programs for dentists, minimal user training is required; — the speed of manufacturing products for laboratories will be 10 times higher, which means the cost will be lower.
Rice. 3. Samples of printed products - templates, braces a) b)
Rice. 4. Models were printed on an M2 carbon printer [11]
Additional options: - high resolution; — color close to natural; - excellent surface quality with minimal roughness, which is ideal for thermoforming templates. In Fig. Figure 4 shows an example of the successful use of Carbon technology at Byrnes Dental Lab (UK). After installing the first M2 machine in Europe and receiving results, the owner of Ashley Byrne ordered a second same machine a day later to provide products not only for himself, but also for other dental clinics, Ashley Byrne said in an interview with TCT. In Fig. Figure 5 shows production boards with finished products printed on Formlab's Form 2 printer.
Rice. 5. Working boards with printed finished products (Form 2 printer) a) b)
Materials
Materials for AM technologies in dentistry can be divided into several groups depending on the material (polymers, including resins and thermoplastics; ceramics and metals), as well as on the state of the material (powder, thread, liquid). 1. Thermoplastic polymers for FDM machines, where a thermoplastic filament is heated and extruded through a die, creating a precise structure layer by layer. Examples of plastics: ABS, PLA (suitable for intraoral use). Sometimes biodegradable polyester with a bioactive additive (tricalcium phosphate) is added to thermoplastic and used as building structures (scaffolds) in dentistry. Wax materials are used as models for subsequent lost wax casting. Photopolymer resins are used in equipment where curing occurs due to exposure to UV radiation or laser radiation. Photopolymers provide a wide choice in color, hardness, and additives of various components. They add biocompatible and bioactive additives, such as bioactive glass. Photopolymers can also be used instead of wax models for precision casting. 2. Ceramics Used for the production of building templates or for ceramic prostheses. AM technologies: - SLS, including cement powders, makes it possible to obtain a structure similar to ceramics and comparable in properties [12]; — extrusion of ceramic powders with a binder followed by sintering to obtain the required strength; - sintering of aluminum oxide powders to obtain a structure of high density and acceptable strength - Inkjet 3D printing technology [13]. It is also possible to make prostheses from zirconium oxide powder with a binder followed by sintering [14]. Unfortunately, ceramic products made by sintering (AM) have a number of disadvantages, such as anisotropy of shrinkage during sintering and visible layers of construction on the surface of products. Therefore, they can only be used as construction templates (scaffolds). 3. Combination of binder and powder Used in injection technology (InkJet): a binder is applied in liquid form with high precision into a bath of powder using a matrix with multiple nozzles. The construction process is layer-by-layer. After completion of construction, the product is subjected to heat treatment, as a result of which the binder is removed and the material of the product is sintered. A wide range of ceramics and metal ceramics are used. 4. Metals We are mainly talking about alloys based on titanium and CoCr. Nickel alloys are now practically not used in prosthetics in dentistry due to the risk of nickel allergy. Titanium alloys of the Ti6Al4V type are ideal for the manufacture of prostheses using the SLS method: they are biocompatible, have high mechanical properties and good ability for osseointegration of implants. Prostheses based on precious metals, which were popular in the past, have now given way to CoCr alloys, which are cheaper, have good compatibility with cement, higher hardness, lower specific gravity, and greater corrosion resistance [15].
Technologies
The article [16] provides a comparative analysis of the microstructure and mechanical properties of prostheses when manufactured using the classical casting method, using AM (SLS) and processing using CAD/CAM technology. When choosing a technology, it is necessary to take into account the shrinkage of the material when cooling the melt during casting, which can lead to disruption of the geometry of the product. Correcting them with post-processing will not be easy due to the high hardness of the alloy. Metalworking (CNC) produces a lot of waste, stresses may occur when supports are removed, and shrinkage during processing must also be taken into account. AM technology eliminates most of these problems. At the same time, direct laser sintering (DMLS) technology is more preferable compared to SLS. Comparative tests were performed on three types of metal 3D printers: PM 100/PXM (Phoenix Systems, Riom, France, now 3D Systems), Eosint M270/M280 (EOS GmbH, Munich, Germany) and Bego (Bego Medical, Bremen, Germany) ). AM technologies are most widely used in the creation of biomodels for diagnostics, in training in planning and performing surgical operations with the subsequent manufacture and use of implants. In Fig. 6–13 show examples of performing individual work using AM.
Rice. 6. Surgical template for implant placement
Rice. 7. Final restoration (material - Dentca)
Rice. 8. Orthodontic model of the lower jaw (material - FotoDent)
Rice. 9. Surgical template
Rice. 10. Base (material - Dentca)
Rice. 11. Drilling template (material - FotoDent)
Rice. 12. Container for impressions
Rice. 13. Final model and model elements for implant installation
The number of operations using AM to manufacture corresponding maxillofacial prostheses and prostheses for cranial reconstructions is also increasing. Before the surgical operation itself, it is possible to test and adjust the future finished reconstruction using a prosthesis model and reduce the operation time by 1–1.5 hours [17]. In implantology, it is strongly recommended to use surgical templates, which greatly reduce the risk of possible surgical complications. The accuracy of the templates is very high: angular deviation is no more than 2 degrees, linear deviation is within 1.1 mm. Another application of AM is the production of scaffolds (building porous structures) for subsequent osseointegration; the choice of material here is decisive. Because it is necessary not only to ensure high manufacturing precision and biocompatibility of the prosthesis, but also its dissolution over time after tissue has grown inside the porous structure of the prosthesis. AM makes it possible to obtain a fine-mesh pore structure (pore size from 300 µm) with their correct distribution and size, which is impossible with traditional methods [18]. Intraoral AM applications: production of ceramic models using intraoral scanning with subsequent production of dental prostheses and caps (wax-up); manufacturing using SLA technology a full arch of teeth in the upper and lower jaws, including for training purposes. In general, the prospects for the use of AM in dentistry, taking into account the reduction in prices for AM equipment and materials, as well as taking into account the rapid and dramatic improvement of technology, look quite optimistic.
On the issue of accuracy of AM equipment
SLA equipment can create structures with a layer thickness of 25 microns, InkJet prints with a minimum thickness of 12 microns, FDM provides a layer thickness of 127 microns. A comparison of different technologies in terms of the accuracy of manufacturing prostheses and their elements was carried out in [19]. The discrepancy in the gap along the marginal line is considered acceptable within the range of 70–102 microns.
Advantages of AM - Flexibility in the use of a wide range of machines and materials for both research and practical use; — the emergence of new inexpensive, higher quality machines and materials is expected due to the expiration of patents in the field of AM; — possibility of simultaneous printing with several materials; — the passive nature of printing (without changing the phase state of the material) avoids problems associated with warping when heating and cooling a CoCr product; — minimum waste of material (40% lower than in metalworking). At the same time, 95–98% of AM waste can be returned to work [20]; — product dimensions are determined by the dimensions of the working chamber of AM equipment; usually they significantly exceed the capabilities of CNC equipment in terms of product dimensions.
AM limitations (to date) - Layered effect (steps) on the side surfaces of the product; — inability to use ceramic products for printing due to high porosity; — reproducibility or repeatability of products is still at a low level; — the need to build supporting structures; — there are still few companies producing AM equipment that produce machines specifically for dentistry.
What do we expect in the future from AM?
— Creation of new materials; — the emergence of new, client-oriented tools; — development of local AM services in hospitals; — development of AM technologies towards faster printing and increased production volumes; — increasing integration between visualization, software, and 3D printing equipment; — improving communications between the medical community and regulatory government agencies; — growth in bioprinting, including printing electronics into medical devices; - for local service centers at hospitals, greater use for training and planning of surgical operations, improved prediction and confirmation of results.
Application Expectations
In 2021, the Non-Profit Medical Association (SME, USA) conducted a survey of medical specialists on forecasts for the use of AM technologies in medicine. Some answers for dentistry are shown in Fig. 14–16.
Rice. 14. Forecast for materials use (SME, USA)
Rice. 15. Forecast for the use of AM technologies (SME, USA)
Rice. 16. Forecast for AM application areas (SME, USA)
Rice. 17. Comparison of the cost of a part using injection molding and AM technology
From Carbon CEO J. DeSimone on the dramatic price cuts for consumables: “This simple price cut by Carbon marks the beginning of the 3D world's transition from a current $10 billion market to a multi-hundred billion dollar digital manufacturing industry. Let's compare the mass production of products using classical technology of casting into molds and using AM (Fig. 17). The cost of casting decreases with increasing production volume, while for AM it does not change. For a long time, prices for AM consumables were too high and did not allow for a significant increase in production. Therefore, the volume of production using AM today is a modest $10 billion.”
Conclusion
Digital manufacturing - AM - is now dominant over traditional CNC-based technology. For now, AM is quite expensive for dentistry, but in the future, a significant reduction in the cost of equipment and materials is expected, mainly due to the expiration of patents on AM technologies.
The CoCr alloy is most suitable for the manufacture of dentures using AM technology due to its unique properties: low cost, good mechanical properties. Due to its high hardness and low toughness, the alloy is not used for casting or CNC machining. The minimal waste of AM and the passive nature of AM eliminates many of the problems associated with post-processing of printed products. ■
References 1. www.dentsplysirona.com 2. www.sme.org/globalassets/sme.org/media/white-papers-and-reports/2018‑sme-medical-am3dp-annual-report.pdf 3. www.materialise .com/en/medical/mimics-inprint-formlabs 4. https://formlabs.com/blog/new-formlabs‑3shape-integration-to-simplify-dental-surgical-guide-workflow/ 5. https:// www.materialise.com/en/press-releases/materialise-and-siemens-healthineers-syngovia-partner-to-bring‑3d-printing-to 6. www.usa.philips.com/a‑w/about/news /archive/standard/news/press/2017/20171127‑philips-teams-with‑3d-printing-industry-leaders‑3d-systems-and-stratasys.html 7. Current status and applications of 3D scanning in dentistry Mohd Javaid, Abid Haleem, Lalit Kumar, “Clinical Epidemiology and Global Health”, www.elsevier.com/locate/cegh 8. Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health. 2017; 17:2–11. 9. Kumar L, Shuaib M, Tanveer Q, Kumar V, Javaid M, Haleem A. 3 D scanner integration with product development. Int J Eng Technol. 2018; 7 (2): 220–225. 10. Nedelcu RG, Persson AS. Scanning accuracy and precision in 4 intraoral scanners: an in vitro comparison based on 3‑dimensional analysis. J Prosthet Dent. 2014; 112(6):1461–1471. 11. www.tctmagazine.com/3d-printing-news/tct-talks-to-byrnes-dental-lab/ 12. Tian X, Gu nster J, Melcher J, et al: Process parameters analysis of direct laser sintering and post treatment of porcelain components using Taguchi's method. J Eur Cera Soc 2009; 29: 1903–1915. 13. Maleksaeedi S, Eng H, Wiria FE, et al: Property enhancement of 3D-printed aluminum ceramics using vacuum infiltration. J Mater Proc Tech 2014; 214:1301–1306. 14. Ebert J, Ozkol E, Zeichner A, et al: Direct inkjet printing of dental prostheses made of zirconia. J Dent Res 2009; 88:673–676. 15. Li KC: Microstructure and phase stability of three dental cobalt chromium alloys used for porcelain-fused-to-metal restorations during thermal processing. PhD Thesis, Otago, New Zealand, University of Otago, 2015. 16. Choi YJ, Koak J-Y, Heo S-J, et al: Comparison of the mechanical properties and microstructures of fractured surface for Co-Cr alloy fabricated by conventional cast, 3‑D printing laser-sintered and CAD/CAM milled techniques. J Kor Acad Pros 2014; 52:67. 17. Jardini AL, Larosa MA, de Carvalho Zavaglia CA, et al: Customized titanium implant fabricated in additive manufacturing for craniomaxillofacial surgery. Virt Physi Protot 2014; 9: 115–125. 18. Habibovic P, Gbureck U, Doillon CJ, et al: Osteoconduction and osteoinduction of low-temperature 3D printed bioceramic implants. Biomaterials 2008; 29: 944-953. 19. Tamac E, Toksavul S, Toman M: Clinical marginal and internal adaptation of CAD/CAM milling, laser sintering, and cast metal ceramic crowns. J Prosthet Dent 2014; 112:909–913. 20. AbduoJ, LyonK, BennaniV, etal: Fitofscrew-retainedfixed implant frameworks fabricated by different methods: a systematic review. Int J Prosthodont 2011; 24: 207–220.
N.M. Maksimov, Nika-Rus LLC
Source: magazine “Additive Technologies” No. 1-2019
Indications for treatment with the Vector device
- Periodontitis of varying degrees.
- Periodontal disease (as determined by the doctor).
- Gingivitis, including in pregnant women.
- Prevention and treatment of peri-implantitis.
- Installed braces.
- Supportive treatment for periodontal diseases concomitant with systemic diseases (endocrine, cardiovascular pathologies).
- Planned hygienic oral care for the prevention of periodontal diseases.
- Sanitation of the oral cavity before dental treatment, implantation, in women - when planning pregnancy.
If Vector Fluid Abrasive with abrasive particles of silicon carbide is used instead of Vector Fluid Polish, the Vector device is used for minimally invasive preparation of carious cavities and treatment of artificial teeth.
Orthopedics
Orthopedic dentistry developed on the basis of dental prosthetics and today is an independent branch of dentistry. Today this is a comprehensive diagnosis of the condition of the dental system, correction of irreversible changes in the dentition in order to prevent its further deformation.
Restoration of dental defects is carried out using removable or fixed prosthetics. The choice of prosthetic method and materials for the manufacture of dentures is based on the results of an examination of the patient’s dentition. In modern practice, removable and fixed prostheses are used, which in turn are divided into:
- Temporary;
- Permanent;
- Microprostheses;
- Macroprostheses.
Microprostheses mean artificial crowns that replace one damaged tooth or part of it; macroprostheses include bridges of various modifications for the correction of extensive defects in the dentition.
Orthopedic dentists work closely with dentists of other specializations, in particular, therapists, surgeons and implantologists. The responsibilities of an orthopedist include not only eliminating the existing defect, but also preventing possible diseases, as well as timely diagnosis of possible dental deformations.
The most progressive method of prosthetics is the installation of fixed dentures on implants. Implantation technology is universal; it is suitable for restoring any number of missing teeth, including cases of complete edentia.
General information about the profession
A dentist is a doctor who deals with the diagnosis, treatment and prevention of problems in the maxillofacial area. This specialist is primarily competent in matters of dental therapy and prosthetics.
Why is dentistry considered a very promising field? There are several answers to this question:
- Firstly, throughout the history of human development, people have strived to improve the quality and duration of life. One of the ways to succeed in these endeavors was through scientific research in the field of medicine. The problem of treating dental diseases was mentioned in the works of Hippocrates. These same questions concern our contemporaries.
- Secondly, the deterioration of food quality, the widespread addition of sugar and sugar-containing products, and an excessive amount of chemical compounds in our daily diet accelerates the process of tooth decay, which, in turn, increases the demand for dentists.
- Thirdly, the technological capabilities of modern dentistry expand the range of competencies of the dentist and make it possible to solve more serious problems, for example: changing the bite, replanting bone tissue, modeling, creating and using different types of prostheses.
Every year, medical universities graduate certified dentists, but the demand for these specialists still does not decrease.
Dentistry for pregnant women
Dentistry for pregnant women became a separate area relatively recently. This is due to the peculiarities of the physiology and psychological state of expectant mothers. Patients during this period are very vulnerable, they need more attention from the doctor and more gentle treatment methods. Consultations, preventive examinations and sanitation are carried out more often than usual during this period. You should visit your doctor at the beginning of the first and second trimester, and also around the middle of the third trimester. At a later date, treatment of detected problem teeth will be very difficult.
While carrying a child, the body of the expectant mother is subjected to double stress. The body's need for vitamins and microelements approximately doubles. In this regard, it is necessary to adjust the diet, in particular, increase the proportion of calcium-containing products.
At the same time, it is very important to maintain dental health, since any source of infection poses a potential threat to the child. Just a few decades ago, dental treatment during pregnancy was not a safe procedure. Modern drugs and anesthesia methods have reduced the risk of exposure to the fetus to a minimum.
In addition to the actual treatment of teeth and periodontal diseases, more attention should be paid to oral hygiene during pregnancy. Dentists recommend choosing toothpastes with a high fluoride content, replacing your toothbrush with a softer one, and using dental floss for more thorough cleaning of your teeth. It is recommended to brush your teeth after every meal, as hard tissues become more vulnerable to the effects of waste products of the oral microflora.
How and where can you study to become a dentist?
Admission to a medical school begins with entrance exams. The future doctor must successfully pass the Unified State Exam in chemistry, biology and the Russian language. This stage cannot be treated negligently, since the competition for the Department of Dentistry is usually above average.
The duration of study at the university is 5 years. This is followed by one year of internship and two years of residency. This length of the educational process is associated with a serious responsibility that falls on a doctor who begins to independently see patients.
As for choosing an educational institution, there is a department of dentistry in almost any medical university. The most authoritative medical universities in Moscow are the Moscow State Medical University named after I.M. Sechenov and Moscow State Medical and Dental University named after A.I. Evdokimov.
The northern capital is proud of the graduates of the St. Petersburg State Pediatric Medical University and the Medical University named after. Academician I.P. Pavlov.
It is also worth adding Kazan, Ural and Samara State Medical Universities and the North-Eastern Federal University named after M.K. Ammosova.
Nurses assist dentists. They learn the craft at dental colleges. Medical School No. 1 and MIIT Medical College are currently considered the best.
Employment opportunities and salary levels
After graduating from a medical university, students are required to undergo an internship and residency, so there are no difficulties with getting a job.
If we take the public sector of medical services, then a young specialist has two options:
- Improve your professional skills and grow up the career ladder, the peak of which is the post of chief physician.
- Develop in the field of scientific research and engage in theoretical aspects of solving dental problems. To do this, a doctor needs to enroll in graduate school and then strive for doctoral dissertation and scientific degrees.
In private clinics the situation is different. In addition to the fact that the employee has the opportunity to realize his career aspirations, paid medical centers show the doctor medicine from a commercial point of view and give him a chance to open his own clinic or medical school in the future.
A dentist’s income depends on his place of work, region of residence, work experience and position. Moscow specialists working in state clinics receive from 20,000 rubles. The average is 40-45,000 rubles.
As for medical centers that provide paid services, dentists there earn 60-80,000 rubles per month. The most qualified employees receive up to 100,000 rubles per month.
These are average numbers. Private medical centers are willing to pay more to the most experienced doctors who strive for continuous development.
There are also differences in the salaries of dentists responsible for different areas: a surgeon or, for example, an orthodontist earns more than a dental therapist. But this is not a reason to be upset, because the modern distance education market offers many retraining courses that allow you to learn surgical, therapeutic, orthopedic, general, preventive and even pediatric dentistry on the basis of your existing medical education. Possession of skills in several areas gives a doctor an advantage over his colleagues and is almost certainly the key to higher wages.
Children's dentistry
The rudiments of teeth in a child are formed during intrauterine development. The health of a child’s teeth largely depends on the lifestyle of the expectant mother. The eruption of baby teeth usually begins at 6 months of life, less often it can be shifted to earlier or later dates. The first visit to the dentist should ideally coincide with this important period in the baby's development. The doctor will examine the child, give recommendations for caring for the first teeth, recommend a toothbrush, and later tell you which toothpaste is suitable for the baby. The main task of a pediatric dentist is to help shape the child’s dental culture and prevent possible problems with oral health in general. In the first years of a child’s life, you should visit the dentist at least once every 3 months.
From about 7 years of age, the priority should be the prevention of diseases of permanent teeth. Among the most popular preventive measures, the procedure for deep fluoridation of teeth is in the lead. In order to prevent carious lesions, it is recommended to seal fissures. This procedure is completely painless and does not cause discomfort to the little patient. The period of changing teeth is also one of the most favorable for orthodontic treatment, if necessary.
The fundamental difference between pediatric dentistry and adult dentistry is the use of more gentle treatment methods and anesthesia. When pain relief is required, sedatives or a combination of sedatives and anesthetics are increasingly used.
Orthodontics
Orthodontics is a separate preventive area of orthopedic dentistry.
The task of an orthodontist is to correct dental anomalies, including congenital ones. Alignment of the dentition and correction of the bite are necessary to prevent pathological abrasion of teeth, diseases of the temporomandibular joint, and inflammatory processes in the soft tissues of the gums.
An abnormal bite is accompanied by improper distribution of the load on the bone, which leads to jaw deformation and increases the likelihood of developing periodontitis and periodontal disease. In addition, an incorrect bite distorts the proportions of the oval of the face and entails psychological problems.
To correct malocclusions, removable and non-removable orthodontic devices and devices are used: braces, mouth guards, retainers. In some cases, the patient requires the help of a surgeon.
Treatment tactics are developed individually, based on data from a comprehensive examination of the patient. The choice of device is made taking into account objective indications, the psychological mood and solvency of the patient.
Orthodontic treatment is a long process; depending on the severity of the anomaly and the age of the patient, correction can last from several months to 2.5 years. The bite can be corrected throughout life, but the most effective treatment is in adolescence, during the period of active formation of the skeletal system as a whole.