Tooth root caries is considered the most dangerous. It is difficult to identify due to its unclear clinical picture. The risk that disease will lead to its removal is very high. It is almost impossible to determine pathology during a visual examination; an x-ray is required. Let's consider the features of tooth root caries: its causes, signs and treatment.
In this article
- Dental root caries: causes
- Symptoms of tooth root caries
- Diagnosis of root caries
- Treatment or tooth root extraction
- Drug treatment of tooth root caries
- Surgical treatment of tooth root caries
- Severe root damage
- When is the best time to remove a tooth?
Based on localization, carious lesions are divided into 4 types: crown caries, cervical, basal and root caries. Damage to the root part occurs under the gum; upon examination, it is almost invisible. If the patient has no complaints of pain, the disease is not always detected even during a preventive examination.
As a rule, pain occurs in cases where root caries has spread to the cervical area. However, at this stage it can already be detected during a visual inspection. The likelihood that the tooth will have to be removed at this stage of the disease is quite high. Moreover, tooth root caries can lead to infection of the gums and jaw, which can lead to various complications.
Often, this form of caries develops in older people, which is associated with atrophic periodontal processes, which are a consequence of age-related changes. Atrophy of the gums leads to exposure of the roots of the teeth, as a result of which they become more vulnerable to cariogenic microorganisms - the main “culprits” of caries. But this pathology can also develop in young people who do not take care of their oral hygiene. Tooth root caries affects 35% of pensioners; among young people it is diagnosed in 1.3% of cases.
Types of caries localizations
Caries (lat. caries rotting) is a slow and hidden pathological process occurring in the hard tissues of the tooth. It is characterized first by focal demineralization of the enamel, then by the destruction of hard tooth tissues with the appearance of a cavity in the dentin. If left untreated, the tooth is lost or complications arise - pulpitis and periodontitis.
Cervical (circular)
The structure of a tooth is divided into a root, a neck and a crown - the latter is located above the gum. The neck and root are located in the gum and are protected by soft mucosal tissue.
When the carious process begins to destroy the tooth in the area of contact of the crown with the mucous membrane, we can talk about the cervical form of caries.
This category is the most difficult to diagnose and treat. It most often affects the incisors. When biting food with incisors, the food is not only “cut off”, but also gets clogged into the gum pockets, moving towards the gums.
Crown caries
Caries has the ability to affect not only healthy, but also already treated teeth - under a filling or crown. If there is a crown, it is difficult to detect, because the tooth does not have a nerve and pain is not felt. There are no external signs for a long time.
The causes of this type of caries are:
- defect of the dental crown with the appearance of access to the tooth tissue underneath it
- poorly treated tooth before prosthetics;
- gum disease;
- poor oral hygiene.
The problem is that the process spreads into the deep layers and spreads to the bone structures, as a result of which the tooth is often completely removed. That is why preventive examinations and an orthopantomogram - a panoramic image of the entire jaw - are so important.
Radical caries
Basal and cervical caries are similar. Both incisors and chewing teeth are affected. Destruction begins with the enamel, gradually moving to the nerve in the root canal. When the process touches bone tissue, it threatens with osteomyelitis.
The main reason for the occurrence is a cariogenic situation in the oral cavity, when plaque accumulates especially quickly. The enamel in the root part of the tooth is much thinner and more easily destroyed. It is most often diagnosed between the ages of 30 and 60 years.
Root caries
Root or subgingival caries occurs hidden. It can be with or without a cavity. Along the flow - active, suspended, secondary. It most often affects molars.
Treatment
Treatment tactics are determined by the stage of the carious lesion.
Initial. The structure of hard tissues remains almost unchanged, there are signs of enamel demineralization, and white spots may appear. To stop the destruction of hard tissues, remineralization is performed. Remotherapy will help strengthen the enamel and stop its destruction. Before remotherapy begins, professional hygiene and cleaning of periodontal pockets are performed. Additionally, the doctor may prescribe rinsing with antiseptic solutions.
Dark spot. The dentist removes hard and soft deposits from the surface of the enamel and cleans the periodontal pocket. The affected tissue is removed and a filling is performed. If gum damage has already begun, a focus of inflammation has appeared, additional treatment is carried out: the doctor stops the infection.
Formed cavity. It will be possible to save the tooth provided that the inflammation has been stopped. The doctor removes the affected tissue, strengthens the crown with an inlay, and places an artificial crown.
Root destruction. If the root is destroyed by more than 50%, with severe inflammation or damage to periodontal tissue, the tooth must be removed. After this, implantation and prosthetics or restoration with a dental inlay are performed.
What is the danger of this disease?
Caries is dangerous because there are no symptoms for a number of years. It is detected more often in an advanced stage, when tooth extraction becomes the solution.
Visual diagnosis is difficult because all destructive processes occur inside the tooth. Pronounced plaque or tartar hides any stains on the enamel.
The root is hidden under the gum and external irritants do not affect it until a certain time. On the other hand, the root walls are thin, so they are destroyed quickly and with complications.
Diagnosis and symptoms of tooth root caries
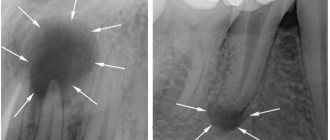
Diagnosis of root caries is complicated by the fact that the disease can be asymptomatic for quite a long period of time. A visual examination of the oral cavity only in 11 - 13% of cases helps to identify the presence of the disease. Therefore, additional examination methods are required for diagnosis:
1) probing;
2) X-ray examination (orthopantomogram, radiography, etc.);
3) electrical odontometry (assessment of nerve response);
4) thermometry (checking the reaction to hot and cold).
It is impossible to identify the presence of dental root caries on your own, but basal or cervical caries, which in most cases accompany root damage, is quite possible. This can be done with a toothpick and a mirror. With clean hands, take a toothpick and pass it between the gum and tooth, pressing lightly. If pain occurs or roughness is found on the enamel, there is a possibility of developing caries of the cementum of the tooth root. This means it's time for you to visit the dentist.
Symptoms of root caries, which, as we noted above, may not always appear:
- pain when exposed to high/low temperatures;
- pain when eating sour and sweet foods;
- increased sensitivity of the periodontium;
- discomfort when chewing;
- aesthetic defect at the border with the gum.
Causes of the disease
There are 3 main provoking factors that must act in a complex manner; none of them acts independently:
- Cariesogenic microflora - this includes Mutans streptococci, actinomycetes and certain types of lactobacilli. They should dominate the oral cavity. Bacteria produce organic acids from food carbohydrates, which cause demineralization of cement.
- Consumption of simple carbohydrates is the most cariogenic. Their breakdown produces glucan, which contributes to the appearance of plaque.
- Reduced caries resistance is a deterioration in the resistance of tooth tissue and the body as a whole. This is facilitated by a decrease in calcium content in hard root tissues, bad habits, and lack of saliva.
In addition, the anatomical features of the mouth can also have an effect - a small vestibule, a short frenulum, and bite pathology.
Gum disease, pocket formation
Gum pocket or otherwise periodontitis is a common occurrence in many patients. Many people do not treat it because it does not bother anyone for a long time.
The first manifestation of pathology is bleeding when brushing teeth, although outwardly they may look healthy. Dental pockets or depressions are normal, but their anatomical size should not exceed 3 mm.
Then the pocket is able to self-clean from food debris and epithelial particles. Reservoirs of bacterial accumulations form in deep gaps. This is accompanied by bad breath. Conventional treatment with antibiotics and brushing teeth with toothpaste have no effect.
Causes of periodontitis:
- insufficient hygiene;
- poor quality fillings;
- abnormal position of the dentition, malocclusion;
- hereditary predisposition;
- deficiency of vitamins and minerals;
- immunosuppression.
Dental root caries: causes
Root caries occurs as a complication of gum disease, in which pathological pockets form between the tooth and gum. They accumulate food debris and pathogenic microbes. They are difficult to remove with a toothbrush and require professional cleaning at the dentist's office.
Without proper oral care, cariogenic bacteria multiply rapidly. They secrete acids that corrode the cement of the tooth root. Gradually, microorganisms penetrate deep into hard tissues down to the pulp, causing pain.
Often this pathological process is caused by osteomyelitis, periodontitis, periodontitis or periostitis, that is, inflammatory diseases of the gums and hard tissues of the oral cavity. Indirect causes of the development of tooth root caries are past infectious diseases and reduced immunity. In addition, the likelihood of carious lesions increases with tobacco smoking, alcohol abuse, poor diet and lack of vitamins and minerals in the body.
If a person rarely brushes his teeth or does it incorrectly, the carious process spreads even faster. As a result, you can lose a tooth without even feeling symptoms of the disease. As a rule, the first signs appear after the pathology has affected most of the tooth root.
Lifestyle
If you have learned about the risk group for root caries (older age), this does not mean that you can relax. Caries has many causes and can occur at any age if basic precautions are not followed.
Those at risk include smokers, diabetics, pregnant women and even children. The provoking factors in this case are:
- smoking and lack of oral hygiene;
- infrequent brushing of teeth and lack of fluoride;
- poor nutrition with preference for desserts;
- frequent stress;
- alternating hot and cold;
- structural features of the oral cavity;
- alcohol abuse - alcohol breaks down into sugars and acids;
- abuse of coffee and strong tea, which creates an acidic environment in the oral cavity;
- lack of water intake, and therefore lack of saliva;
- gum injuries.
Detection techniques
The best option for identifying cement caries is a comprehensive diagnosis , which includes a variety of techniques:
- Visual inspection and recording of patient complaints . At the same time, the general condition of the dentition, gum tissue, and mucous membranes is assessed. The recession of the gums near the affected crown and the degree of its attachment are determined. The presence of deposits and tooth sensitivity are detected.
- Probing .
To do this, use a sharp probe that penetrates under the gum. Healthy tissue can be distinguished from damaged tissue by some roughness of the root surface. The detection of softened areas signals the rapidly progressing development of pathology. Examination of the resulting cavity with a probe reveals uneven chipped edges. - X-ray diagnostics . Allows you to identify in detail even small defects on the root and determine the degree of caries damage. Most often, bite-wing radiographs and orthopantomograms are used for this.
- Diagnostics using a visiograph . This device transmits the image to a computer monitor, where it can be enlarged and viewed in different projections.
- Thermal diagnostics – helps determine the stage of caries.
To do this, the tooth is treated with hot or cold water. If the pain is short-lived, then the pathology has affected only the superficial layers. The presence of severe, persistent pain indicates the spread of the disease to the pulp. - Electroodontometry is the effect on the pulp of an electric current of varying strength.
Depending on the reaction obtained, the degree of pulp damage is diagnosed. This procedure is painless, and with just a little pinching, the dentist can accurately determine the diagnosis.
Photo: caries inside a tooth root on an x-ray
It is difficult to independently diagnose root caries, and in some cases impossible. That is why you should not neglect a routine visit to the dentist, who can detect pathology at an early stage.
Symptoms of the disease
The process usually occurs without symptoms, but pain may occur when brushing a toothbrush, eating sour, salty, sweet, cold or hot foods.
After eliminating the irritant, everything goes away. The patient can see a doctor if a stain is found on the front surface of the incisors, but often it is hidden under plaque or tartar.
The ongoing carious process gradually reaches the dentin junction, penetrating first into its surface layers and then further. The cavity deepens with bacteria and food debris. There is a smell from the mouth. Irritants cause pain more and more frequently.
With cement caries, teeth become mobile and lose their support, and bleeding gums occur. These are already symptoms of periodontitis. Now, even when chewing food or brushing teeth, severe discomfort occurs.
Digestion begins to suffer. Teeth become hypersensitive to hot or cold.
Next, the process follows the Leus classification:
- Active lesion - the edges of the cavity are undermined. The cavity is filled with softened tissues and tends to grow.
- Suspended caries - no increase in the affected area is observed. The cavity is clean, the bottom is shiny and smooth, the edges are even and dense.
- Secondary caries - occurs under a filling.
When is the best time to remove a tooth?
It is more advisable to cure deep root caries, which develops against the background of severe inflammatory processes, by removing the tooth. There are a number of reasons for this:
- A diseased tooth is a source of infection. If caries was on one root, most likely it will develop in another area.
- A person will constantly be accompanied by bad breath, which is impossible to get rid of.
- Pathology makes teeth mobile, which prevents you from chewing food normally. Problems with the gastrointestinal tract may occur.
- There is a risk of infection entering the circulatory system, resulting in the development of general infections, including sepsis.
In each specific case, the doctor selects an individual treatment program based on medical indications, the patient’s age and financial capabilities.
Diagnosis of the disease
The diagnosis is made in stages. Listening to complaints and visual examination make it possible to diagnose caries only in 13% of cases. Classic probing with a sharp probe and inspection with a mirror are informative. This allows you to examine the dentition.
Thermal diagnostics, electroodontometry and x-rays are also performed. If the patient has massive dental plaque, changes in the enamel will not be visible. In this case, professional teeth cleaning is first carried out to remove plaque and stone. All this is possible in a dental clinic.
At the dental clinic
The following types of studies can be performed at the clinic:
- Probing with a thin probe with a curved end - it is inserted under the gum, while the doctor has the opportunity to examine the structure of the tooth, its integrity, the presence of irregularities and chips. With rapidly progressing caries, the edges of the cavity are uneven and sharp. In the remission stage, the surface of the pathological focus is shiny, smooth, hard with smooth edges.
- Electroodontometry - can determine nerve damage and the depth of inflammation. The pulp reacts differently to the current strength.
- Thermal diagnostics - treatment of different areas of the tooth with a stream of water and heated wax. Unpleasant sensations that disappear after removing the irritant indicate caries.
- X-ray - a targeted photograph of one tooth or computed tomography. The presence and localization of obvious or hidden inflammation is determined with millimeter precision.
- Visiography is a special device - a visiograph scans the received data and transfers it to a computer, where the picture is studied from different angles and in detail, revealing the hidden process of inflammation.
Clinical picture
Unlike other forms of caries, the root form does not always have pronounced symptoms , therefore, to determine the clinical picture and classification according to ICD-10, differential diagnosis is of particular importance.
As a rule, the affected areas differ from the healthy surface in their shade, acquiring a brown or chalky color. But the area of their localization is often blocked by the gum, which makes timely diagnosis difficult.
At the same time, the further development of pathology is not always accompanied by the formation of a cavity . The surface of the affected areas is ridged. Probing reveals some softening of the tissue.
Also, when cement caries occurs, general symptoms are noted :
- painful reaction to any irritants: thermal, mechanical, chemical;
- discomfort in the cervical area;
- darkening of the affected areas.
Later, as the disease develops, other symptoms characteristic of a certain stage of the pathology :
- Initial root damage . It is characterized by extensive demineralization of tooth tissue and a change in the color of the affected areas from white to brown. At this stage, the cemento-dentin boundary is preserved.
- Superficial lesion . It is characterized by the destruction of cement and dentin, with the formation of a small pigmented cavity. The depth of the area does not exceed 0.5 mm. The margins are limited by mantle dentin.
- Deep caries . Destruction leads to a deepening of the area by 0.5 mm or more. Often, only a thin layer of dentin separates the cavity from the pulp. The bottom and edges of the area become black.
Treatment or removal - what determines the outcome
The doctor makes a decision on treatment or tooth extraction after determining the depth of spread and the area of localization of the inflammatory process. It is mandatory to first carry out professional cleaning using an ultrasonic scaler, an AirFlow water-abrasive device and hand tools.
Initial caries is treated with conservative retherapy. For hard tissue defects, preparation and filling are performed. In severe cases, the tooth is removed.
Treatment of the initial stage of root caries
Conservative retherapy includes:
- fluoridation of teeth;
- covering teeth with protective agents
- training in proper oral hygiene
Cleaning in dentistry from stone and plaque
1243900247100
Professional teeth cleaning involves removing the accumulation of all pathogenic microflora around the root.
It involves not only removing plaque, but also stones. This elimination of negative factors protects teeth for a long time.
Antiseptic treatment of affected areas
Treatment of root caries involves drilling out all affected areas with a drill and treating the carious cavity with antiseptics and special preparations. A 2% chlorhexidine solution or a gel based on it is used as an antiseptic for the treatment of carious cavities.
Methods of therapy
To treat root caries, depending on the clinic of the process, two methods are used: conservative and surgical:
- Conservative methods are used at the initial stage of the disease, when the process of destruction has not yet begun.
- Surgical treatment is indicated for the formation of cavities and requires mandatory filling of the crown.
Does tooth pain always occur after root canal cleaning? What to do to relieve pain?
In this article we will discuss whether inflammation of the periosteum can occur after tooth extraction.
Read the link https://www.vash-dentist.ru/lechenie/zubyi/karies/effektivnyie-sposobyi-i-sredstva-profilaktiki.html which methods and means of caries prevention are most effective.
Conservative
Conservative treatment takes place without filling and is carried out in several steps:
- professional oral cleaning;
- eliminating the causes of plaque accumulation : correction of dentures, periodontal treatment, etc.;
- treatment of the crown with a remineralizing preparation . For this purpose, products based on fluoride and antiseptics are used; for a deeper effect, a sealant with fluoride crystals and copper or calcium ions is used.
Operational
These treatment methods involve surgical intervention on the tooth and gum tissues.
The whole process consists of the following manipulations:
- the dentist administers local anesthesia , having previously treated the injection site with an anesthetic gel or spray;
- since it is difficult to protect the treated area from moisture using a cofferdam, in the case of root caries, the dentist performs excision of part of the gum using diathermocoagulation;
- further, he performs corrective suturing of the edges with special hemostatic threads;
- after this, the doctor removes the affected dental tissue, forming a cleaned cavity . To determine the degree of cleansing, a special liquid is used - a caries indicator;
- if necessary, removes the nerve and performs root canal treatment ;
- Finally, the cavity is disinfected with an antiseptic and sealed .
The choice of filling material will depend on the nature and size of the cavity, the general condition of the gum tissue, the location of the affected tooth, etc.
Currently, the following materials are used for filling :
- Amalgams .
They are used very rarely, since their application requires the absolute exclusion of moisture content in the cavity and adjacent areas. In addition, Amalgams contain mercury, which requires certain protection when mixing. With these disadvantages, it is worth noting that this material is the most durable of all. - Compomers .
They allow you to create a strong and aesthetic filling that can withstand heavy mechanical loads. Compomers are recommended for small cavities. The disadvantage of the material is that the fixation in the tooth is not always reliable. - Glass ionomer .
This option is ideal for the restoration of extensive and deep caries lesions. The material is well fixed in a humid environment. In addition, it contains a remineralizing complex that restores tooth structure.
What to do to protect your gums
If the gum is not treated, inflammation will remain and all treatment will become meaningless. The gums are protected by diathermocoagulation and retraction.
Diathermocoagulation
Diathermocoagulation – excision of excess areas of periodontitis with a coagulation knife. The knife immediately cauterizes the bleeding edges. The procedure is performed when there are severe changes in the gums. In such cases, filling is postponed until the soft tissue is completely regenerated.
Retraction
If the condition of the gums is advanced, treatment of caries becomes impossible - the mucous membrane bleeds and interferes with tooth treatment. This gum is excised or a special device is applied to move the gum back. But more often, retraction is performed - lowering the gingival contour or moving apart the overhanging edges of the gums using special hemostatic threads. A temporary filling is placed until complete healing.
Cost of procedures
The cost of treating cement caries consists of several factors: the area of damage, the treatment methods used and materials for restoring the crown.
Treatment of superficial caries can cost 1,500–3,000 rubles. Surgical intervention for deep cement caries will cost significantly more.
On average, the cost of this procedure using light-composite material varies between 3,000–6,000 rubles.
Timely treatment of cement caries is the main factor influencing tooth preservation. The use of a laser allows this procedure to be carried out as accurately and painlessly as possible.
You should not engage in independent diagnosis and treatment of this pathology , as you may waste time. Trust your dental health to a highly qualified dentist.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags diagnostics caries treatment tooth decay
Did you like the article? stay tuned
Previous article
Advantages of CBW prosthetics technology
Next article
Caries between the front teeth: development features and therapy
What preventative measures are there?
To keep your teeth healthy for many years, you need to brush your teeth twice a day, use floss and a tongue scraper. After sweets, you should rinse your mouth and chew gum for 5-10 minutes.
Prevention also includes the removal of tartar. A sufficient amount of saliva is also important, so it is necessary to maintain a water regime.
Like any other pathology, caries is better prevented than treated. Therefore, it is important to visit the dentist twice a year for preventive examinations. People at risk should approach this especially responsibly.