Granulating periodontitis is an inflammatory process in the periodontium, which has a chronic form and periodically worsens. This type of disease is characterized by the formation of granulation tissue. The main symptom is severe pain when chewing food. Acute pain occurs when eating hot food and drinks. Gradually, the gums in the affected area swell, fistulas form, from which pus enters the oral cavity.
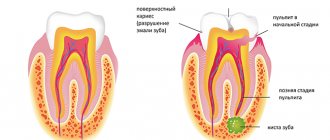
Fact: Granulomatous, fibrous and granulating forms of periodontitis often occur when deep caries is left untreated. Therefore, specialists cannot save the tooth and must be removed if treatment began too late and did not lead to a positive result.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 700
- The cost of an orthodontist consultation is 2,000
Make an appointment
Chronic apical periodontitis
Chronic apical periodontitis is most often an asymptomatic inflammation in the tissues of the apical periodontium, which is manifested by radiological changes at the apex of the tooth roots.
Many dentists use the clinically convenient classification of I. G. Lukomsky. It simplifies the diagnosis.
Chronic fibrous periodontitis
Occurs as an outcome of acute periodontitis or treatment of granulating and granulomatous periodontitis. Traumatic etiology is also important due to overload, which occurs with the loss of a large number of teeth or non-physiological articulation.
Chronic fibrous periodontitis is detected on an x-ray as an expansion of the periodontal fissure in the apex area and is almost never accompanied by destruction of the adjacent bone.
Chronic granulating periodontitis
It is the most active form among all chronic periodontitis and is the outcome of an acute process.
The patient complains of unpleasant, slightly painful sensations when biting on the causative tooth.
Externally, the patient looks as usual, sometimes there is an increase in the submandibular lymph nodes. In the oral cavity we see hyperemic mucosa in the tooth area, painful on palpation. A distinctive feature of this type of periodontitis is the presence of a fistula in the projection of the root apex. It may ooze pus or bulge granulations. Young granulation tissue grows through damaged cement or even dentin into the bone marrow spaces, often growing along the walls of the fistula tract. The tooth is destroyed or intact. Percussion is weakly positive.
On the x-ray we see a clearing area due to bone destruction in the area of the root apex. The lesion has unclear contours and comes in different sizes.
Chronic granulomatous periodontitis
This type of periodontitis is asymptomatic and manifests itself clinically only during exacerbations. These manifestations can be of the type of granulating periodontitis in the form of fistulas and hyperemia of the mucous membrane.
The difference between granulomatous periodontitis and granulating periodontitis is the presence on the radiograph of a clearing focus at the apexes of the roots with a clear round shape (apical granuloma).
Currently, doctors are moving away from grading the size of the lesion (0.5 cm - granuloma, 0.6-0.8 cm - cystogranuloma, more than 0.8 cm - radicular cyst.
Recommendations after treatment
After the operation, it is possible to save the affected tooth if it was performed in a timely manner. But you need to take into account that the disease may reappear if you do not follow the dentist’s recommendations and do not monitor the health of your teeth. To avoid relapse of granulating periodontitis after treatment, follow 4 rules:
- Never allow caries and pulpitis to progress. Severe stages of the disease can provoke the development of periodontitis.
- See your healthcare provider every 6 months for a diagnosis and professional cleaning. Professional oral hygiene eliminates soft and hard plaque, as well as all pathogenic bacteria.
- Use dental floss and a toothpick to remove food debris from hard-to-reach areas. Brush your teeth at least 2 times a day.
- Strengthen your immune system, take a vitamin-mineral complex and lead a healthy lifestyle.
Following these recommendations will help you maintain healthy teeth and gums for many years.
Have you encountered this unpleasant disease? Do not delay treatment - contact the dentistry of the CELT clinic!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Cyst - what is it and why?
A cyst is a cavity that has an epithelial lining and cystic contents. There are two types of cysts - true and pocket.
The true one is completely covered by the epithelial lining, and the pocket one communicates with the root canal, it seems to grow from it.
Cyst formation occurs in 3 stages.
At the first stage, the epithelial cells of the islets of Malasse most likely proliferate under the influence of growth factors.
During the second stage, an epithelial cavity is formed.
These epithelial cells are directed away from their source of nutrition, die, and neutrophils drag their remains into the area of necrosis. Microcavities are formed, which then merge into one and become limited by stratified squamous epithelium.
There is another theory - the theory that the epithelium covers all open connective tissue areas, resulting in necrosis.
At the third stage of cyst formation after the death of neutrophils, there are reserves of prostaglandins, as well as cytokines produced by macrophages and T lymphocytes. Together they activate osteoclasts and trigger bone resorption.
Pocket cysts have a different mechanism of development. There is a large accumulation of neutrophils near the apical foramen in response to root canal infection. The cells die, as before, and this microabscess is closed by proliferating epithelium. A so-called epithelial ring is formed. Neutrophils that remain outside the channel die and form a microcavity. The presence of infection outside the canal further attracts neutrophils, expanding the microcavity to larger sizes. A pocket cyst is called such because the enlargement of the root canal resembles an enlargement of the periodontal pocket.
Removal of tooth granuloma
Treatment through surgery must be used if conservative treatment is ineffective, which often occurs with serious destructive processes in the periodontium and bone tissue. All surgical procedures are performed only under local or general anesthesia.
There are several techniques for performing the operation, but at stage 1, surgical opening of the gums is required to drain the purulent contents. Then drainage is introduced into the lesion, leaving it for up to 3 days for the gradual release of pus.
At the same time, treatment with antibiotics, anti-inflammatory and painkillers is prescribed.
Next, the granuloma is removed using one of the selected techniques:
- Cystectomy.
Cystectomy involves resection (excision) of the root apex. First, a piece of gum tissue is peeled off, providing access to the top of the tooth, after which the granuloma is removed along with part of the root.
After resection of the root apex, the resulting cavity is filled with synthetic tissue substitutes, and the tooth is filled. The operation lasts about an hour.
- Cystotomy.
This method is suitable for removing large granulomas and involves gradual removal of the lesion. First, an artificial channel is created between the source of suppuration and the oral cavity, through which all the pus comes out and is absorbed into cotton swabs. After complete cleansing, active antibacterial treatment of the cavity is carried out, and sutures are applied. Bone tissue gradually grows, filling the cavity freed from pus. The procedure is lengthy, but is tolerated quite easily by patients.
- Hemisection.
The procedure is performed only on multi-rooted teeth. With this surgical technique, the granuloma is eliminated along with the removal of the root and crown fragment. The operation is considered uncomplicated and allows partial preservation of the tooth and its functions, which makes it possible to further carry out full aesthetic prosthetics.
The method is indicated only if the remaining roots and crown are able to withstand the intended load.
- Removal of a tooth
They try to remove a tooth with a granuloma in extreme cases, and only if other measures are ineffective, in the following conditions:
- destruction or cracks in the root;
- pronounced destruction of the pulp and crown;
- dense filling of root canals.
After the tooth is extracted, all the contents from the source of suppuration exit through the hole in the socket, that is, the resulting granuloma is completely eliminated after tooth extraction and antiseptic treatment. At the site of the removed root and tooth, the wound heals and the periodontal tissues are completely restored. After a few months (you should wait for complete healing to occur), you can put a pin for the new tooth.
Surgical treatment is accompanied by the simultaneous use of:
- antibacterial and painkillers in tablets or injections;
- local anti-inflammatory and painkillers: dental gels Metrogyl Denta, Cholisal, Oralcept spray;
- rinsing with antiseptic solutions (Romazulan, Chlorhexidine).
Traumatic periodontitis
Periodontal trauma is one of the initiating factors in the occurrence of hemorrhage and the development of ischemia, which directly leads to the formation of pulp necrosis. The focus of necrosis attracts bacteria, colonizes them and infects the periodontium. With an increase in the number of microorganisms, acute inflammation begins. Traumatic periodontitis develops.
With chronic long-term trauma, periodontal restructuring occurs gradually, first due to its adaptation, then as chronic inflammation with lacunar resorption of the compact lamina.
The main reason for the development of pathology is the inflammatory response. As a result of occlusal trauma, inflammatory mediators are produced in the pulp; they are considered a protective reaction to mechanical aggression. They disrupt microcirculation and increase vascular permeability. The pulp dies.
When pulp necrosis reaches the apical periodontium, due to its cytotoxic effect, interleukins activate osteoclasts and bone resorption.
Medicinal periodontitis
Drug-induced periodontitis develops when aggressive liquids or drugs, such as arsenic paste, formalin, tri-cresol formalin, and phenol, enter the periodontium. Penetration into the periodontium occurs through the root canal.
This also includes periodontitis, which develops in response to the removal of phosphate cement, resorcinol-formalin paste, pins and other filling materials into the periodontium during the treatment of pulpitis. Drug-induced periodontitis also includes periodontitis due to allergies as a result of the use of drugs that can cause a local immune response (antibiotics, eugenol, etc.).
Complications
Abnormal root formation of a tooth is an active source of infection, therefore (if left untreated) serious consequences are possible. Among the common pathological conditions that untreated granuloma leads to:
- further progression of periodontitis and fistula formation;
- inflammation of the tissue of the tooth socket (alveolitis);
- transition of the process to the periosteum with the development of a purulent abscess of flux (periostitis);
- destruction and death of the bone marrow base of the tooth - osteomyelitis;
- resorption (resorption) of periodontal and bone tissue, leading to tooth loss;
- abscess, phlegmon (spread suppuration of the perimaxillary tissue in the oral cavity);
- damage to organs remote from the tooth due to the penetration of infection from the source of suppuration into the lymph nodes (lymphadenitis), heart (endocarditis), liver, kidneys, brain tissue;
- migratory granuloma of the tooth root, in which the process of inflammation migrates (spreads) to the subcutaneous tissue of the face with the formation of an abscess and the formation of new foci;
- septic damage to the body when bacteria enter the bloodstream.
Removal of dental granuloma must be carried out as early as possible to avoid consequences. Therefore, at the first symptoms you need to consult a specialist.
Can a tooth granuloma resolve under the influence of rinses and lotions? By itself (without treatment) or only with the use of rinses, dental granuloma will not disappear, as many believe.
A professional dentist is able to completely remove an abnormal formation and save a tooth at different stages of the pathology, but this can be done without surgery and with the least adverse reactions only at an early stage.
Treatment of granuloma on the tooth root is carried out therapeutically and surgically. The choice of treatment method is determined by the size of the inflammatory focus, the degree of spread of infection and periodontal destruction, and the presence of complications.
To prevent exacerbation of the inflammatory-purulent process, any types of thermal effects on the granuloma are unacceptable (including compresses, heating pads, hot rinses and even eating hot food).
Foreign bodies
Gutta-percha, paper pins, calcium residues and a wide variety of other things can be found in the periapical tissues.
The apical periodontium always reacts to foreign bodies. They can enter through the root canal, through an injured mucous membrane or periodontal pocket.
In the case of paper pin penetration, it should be remembered that the human body does not know how to process cellulose, so the foreign body is surrounded by a bacterial plaque, which maintains inflammation.
Gutta-percha is a biocompatible material. However, at the same time it can give a reaction from the apical periodontium. Studies in guinea pigs have shown that large particles of gutta-percha are encapsulated and surrounded by collagen fibers, while small particles support a local tissue reaction. And magnesium and silicon, which are contained in excess gutta-percha, can cause resorption.
Conservative therapy
Unlike a dental cyst, a granuloma on the root of a tooth is more easily amenable to conservative therapy aimed at suppressing the infectious focus and preserving the crown. Therapeutically, the formation is treated at the initial stage of inflammation, until suppuration develops.
Treatment of granuloma through therapeutic methods includes complex measures: correct filling technique, active disinfection, parallel administration of antibiotic drugs to eliminate pathogenic flora.
Very rarely, the formation disappears only through treatment with antibiotics (usually through injection). However, such a treatment program is only possible for small and non-festering formations.
Filling canals is not permissible without x-rays. The first image before treatment is mandatory and is diagnostic. The second radiograph - control - is performed to assess the correctness of the performed medical manipulations.
How is an abnormal formation removed using dental procedures? The treatment process consists of several stages:
- Removing a previously placed filling or opening an unfilled tooth.
- Mechanical cleaning of the dental canal with access to the granulomatous lesion (which creates conditions for the release of pus), elimination of abnormal tissue.
- Sterilization of the canal by washing with disinfecting solutions, ultrasonic treatment or laser radiation.
- Placing a medicinal substance with calcium hydroxide inside the canal and cavity of the granuloma, which suppresses bacterial activity, causing the growth of bone tissue behind the root apex, which is visible during radiovisiography approximately 20 days after administration.
- Placement of a temporary filling.
After the doctor is convinced that the inflammatory process is suppressed and active tissue healing is occurring (confirmed by x-ray):
- The medicinal paste is removed and the canals are re-treated with antibiotic drugs.
- The final dense filling of the tooth is carried out. The best option is to use the modern method of vertical condensation. It consists in the fact that medical gutta-percha is heated and compacted in the root canal, filling all lateral (side) branches and precisely taking their shape.
When all stages have been completed, you can begin to restore the tooth crown.
Diagnosis of chronic apical periodontitis
Diagnosis of chronic apical periodontitis is similar to that in the case of acute apical periodontitis. This means we use basic and additional diagnostic methods.
The main ones include clarifying the patient’s complaints, medical history, probing, percussion, palpation and determining tooth mobility.
The patient’s complaints are most often absent, but they may complain of discomfort while eating when biting.
Probing is painless, palpation of the mucous membrane in the apical area is also painless. Percussion is weakly positive.
Additional special methods include determining the electrical excitability of the pulp (reduced to 200 μA), determining occlusion (the presence or absence of a traumatic factor), fistula tract, and temperature tests.
NB! We definitely do an X-ray examination.
Symptoms of the disease
During the first stage, which can last up to several years, the patient may not experience serious discomfort or pain, so detecting symptoms may be problematic. Symptoms appear when immunity decreases, caused by the above factors, such as being under stress and overwork.
Symptoms usually begin to appear over time, but the time lag can be up to several years. Among the first signs of the disease, which can appear within a couple of months, it is customary to highlight:
- increased sensitivity when chewing food or biting it,
- a darker shade of the tooth in relation to the neighboring ones,
- short-term pain.
In the later stages, cystogranuloma manifests itself differently:
- acute pain that intensifies when the affected area comes into contact with food,
- sensation as if the tooth has increased in size,
- swelling of the side of the face opposite the infected area.
If procedures are not started at this stage, the spread of infection may cause symptoms:
- sharp throbbing pain that can be felt in the face, ear or neck,
- gum pain, redness and swelling,
- festering gum pocket,
- facial tumor,
- inflammation of the lymph nodes,
- high temperature,
- headache, general malaise, weakness.
In a patient's blood test, accelerated erythrocyte sedimentation and an increased concentration of leukocytes can be detected.