What does dental pulp consist of?
Anatomical structure of the dental pulp
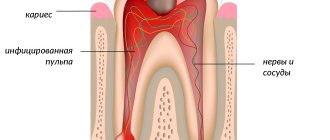
From an anatomical point of view, the tissue is divided into two zones. The coronal dental pulp has a loose structure and is involved in dentinogenesis; all layers of the dental pulp in this part are penetrated by an extensive network of capillaries and nerve cells. The root pulp of a tooth is denser because it does not contain a large number of cellular elements, but is saturated with collagen fibers. Through the apical foramen, the canals communicate with the periodontal tissues and allow minerals and nutrients to reach the tooth walls.
The pulp and dentin of the tooth form a strong complex - the hard tissue protects the tooth pulp from external irritants, and it, in turn, helps the formation of dentin.
The pulp of the front tooth smoothly passes from the crown to the root part, the dental pulp of the molars has clear boundaries - the mouths of the dental canals.
Histological structure of dental pulp
The pulp contains a large number of different elements:
- Elastin and collagen fibers supply the organ with hyaluronic acid, reducing susceptibility to toxins and bacteria.
- Odontoblasts and stellate cells are responsible for the regeneration of dental pulp.
- Leukocytes, lymphocytes and fibroblasts support the vital activity of the epithelium and organize communication between cells.
- A branched network of nerve processes forms Rashkov's plexus and provokes the occurrence of pain sensitivity when exposed to stimuli - the innervation of the dental pulp occurs due to the trigeminal nerve.
- Vessels and capillaries provide the blood supply to the dental pulp, which is necessary to nourish the tissues.
Composition of dental pulp
The fabric is 74% water, the remainder being organic and inorganic layers. Pulp cells include protein compounds, acids, lipids, glucose and various enzymes, which allows the epithelium to actively consume and process oxygen.
Many people mistakenly believe that the pulp is a nerve. The opinion is incorrect, since in addition to nerve plexuses, the tissue contains blood vessels and collagen fibers. |
Innervation of the pulp -
The common sensory or afferent nerve for the maxillary and mandibular teeth are the II and III branches of the trigeminal nerve (i.e., the maxillary nerve and the mandibular nerve). In turn, nerves depart from them, which form plexuses - the superior dental plexus in the upper jaw and the inferior dental plexus in the lower jaw. In turn, bundles of myelinated nerve fibers branch off from these plexuses, which penetrate into the tooth cavity along with blood vessels - through the apical openings at the apexes of the roots. And, accordingly, forming a neurovascular bundle (tooth pulp) there.
The nerve fibers form a subodontoblastic nerve plexus, which is located under the layer of odontoblasts (also called Rashkov's plexus). Unmyelinated nerve fibers depart from this plexus, which are directed to the peripheral areas of the pulp, where they seem to entwine the odontoblasts, forming the so-called “nadodontoblastic plexus” between the odontoblasts and predentin. Some of the nerve fibers end in this plexus, but the rest of them penetrate into the dentinal tubules.
Age-related changes in dental pulp
The pulp of temporary and permanent teeth has a similar structure and only becomes thinner over time. Before the roots are formed, the pulp of a baby tooth is concentrated in the coronal part. Later, the tissue begins to spread into the dental canals through the apical foramen and grow into a wide network. The dental pulp in a child has a massive and dense structure, as well as a large fiber size.
The development of dental pulp continues throughout life, but with age, regeneration processes slow down: the number of active cells decreases, which leads to vascular fragility, insufficient tissue nutrition, the tooth suffers from odontoblast atrophy, that is, the impossibility of dentin formation. The described changes apply to older people.
Chapter 1
TOOTH PULP. ANATOMICAL AND HISTOLOGICAL STRUCTURE, FUNCTIONAL FEATURES
The pulp, or pulp of the tooth (pulpae dentis), is a complex connective tissue organ with various cellular structures, blood vessels, rich in nerve fibers and receptor apparatus, which together perform its functions and ensure the vital activity of the tooth. The pulp completely fills the tooth cavity, gradually passing into the periodontal tissue in the area of the apical foramen. The general outlines of the pulp to a certain extent repeat the shape and external relief of the tooth. The pulp contained in the cavity of the tooth crown is called coronal; in root canals it is called root pulp. The names “coronal pulp” and “root pulp” reflect not only the anatomical distribution nature, they have certain differences depending on the location, shape, structure and function of these anatomical formations. These differences between the coronal and root pulp are especially significant in multi-rooted teeth, where the anatomically pronounced border in the form of the mouths of the root canals appears quite clearly, especially with the development of pathological processes in it.
According to the morphological structure, the pulp is represented by loose connective tissue, which contains many cells, intercellular substance, blood vessels and nerve fibers. Its peculiarity is that, along with cellular elements, it contains a large amount of gelatinous ground substance. The fibers are represented by collagen and reticular (argyrophilic), elastic fibers were not detected in the pulp. The main cellular elements of the pulp are odontoblasts, fibroblasts, poorly differentiated cells (stellate, pericytes), sedentary macrophagocytes and others. These cells are distributed unevenly in the pulp, forming a certain pattern. Conventionally, this allows us to distinguish three layers in it: the odontoblast layer, or peripheral, subodontoblastic, or cambial, central. Each of them performs a specific physiological function or exhibits one or another reaction during the development of various processes.
In the peripheral layer
The pulp, which is directly adjacent to the dentin, contains odontoblasts in several rows. These are highly specialized pear-shaped cells with dark, basophilic cytoplasm. Each of these cells has a dentinal process (Toms fiber), which penetrates the dentinal tubule and branches in it according to the branching of the latter. The cell body is rich in cellular organelles: a well-developed intracellular mesh apparatus, a lamellar complex - the Golgi apparatus, numerous mitochondria, the nucleus contains a lot of chromatin and several nucleoli. Towards the apex of the tooth root, the size of cells and the number of rows of odontoblasts in the peripheral layer of the pulp decrease.
Subodontoblastic layer
consists of small, poorly differentiated stellate cells, from the body of which numerous processes extend, which are closely intertwined with each other. The cells are located directly under the odontoblasts, connect with their elongated body and processes to the odontoblasts and enter the spaces between them. The cells of this layer have the ability, if necessary, to transform into odontoblasts.
Central layer
The pulp contains cells such as fibroblasts, which have a spindle shape. For pulp cells of the fibroblast type, a characteristic functional feature is their differentiation into specific pulp cells, preodontoblasts and odontoblasts. In addition to fibroblasts, this layer contains a large number of sedentary macrophagocytes (histiocytes). The presence of these reticuloendothelial cells in the pulp provides its protective role. Both in the subodontoblastic and central layers of the pulp there are a large number of adventitial cells (pericytes) located along the vessels. These cells belong to the poorly differentiated cellular elements of the pulp. During inflammation, adventitial cells progressively change and transform into either fibroblasts or free macrophages. Thus, the presence of poorly differentiated cellular elements (stellate and adventitial cells) in the pulp is associated with the ability of the pulp to regenerate. In addition to cellular elements, this layer contains thin reticular and collagen fibers. Reticular fibers predominate in the odontoblastic and pododontoblastic layers, and collagen fibers predominate in the central layer.
Blood supply to the pulp
The pulp has a fairly well-developed blood supply system, the anatomical and topographic structure of which is closely related to the anatomical and topographical features of the tooth cavity. The main arterial vessel, accompanied by 1-2 veins and several nerve branches, penetrates the pulp through the apical foramen and, reaching the mouth of the coronal pulp, breaks up into arterioles and forms a dense network of capillaries. A particularly dense plexus of small precapillary vessels and capillaries is formed in the subodontoblastic layer, from where the capillaries penetrate the odontoblasts, entwining their bodies. The capillaries become veins, which have very thin walls and a much larger diameter than arteries. The veins follow the main course of the arteries and exit through the apical foramen of the root. There are numerous anastomoses between the arterial vessels of both the root and coronal pulp, and deltoid branches in the apical area. The diameter of the apical foramen is greater than the diameter of the vascular foramen around them in both the superficial and deep layers of the pulp. They also exit through the apical foramen, flow into large lymphatic vessels and subsequently into deep lymph nodes.
Innervation of the pulp
The dental pulp of the upper and lower teeth is innervated by the branches of the trigeminal nerve and is a highly sensitive tissue. Bundles of pulpy nerve fibers enter through the apical foramen of the root, forming, together with blood vessels, a neurovascular bundle. At the beginning of the root canal, the nerve bundle is almost unbranched; later it gives off thinner branches and individual nerve fibers, which go in different directions to the periphery of the pulp, forming here the pododontoblastic nerve plexus - Rashkov's plexus. It has a large number of nerve endings, and is most pronounced in the area of the horns of the coronal pulp. A significant portion of the nerve fibers from the central layer of the pulp are directed through the odontoblast layer into the predentine and dentin. Above the layer of odontoblasts, at the border of pulp and dentin, part of the nerve fibers forms a supraodontoblastic nerve plexus, the fibers of which branch in the main substance of predentin. Various receptors are described in the pulp: in the form of branched bushes, brushes, etc. Along the dentinal processes of odontoblasts, nerve fibers can penetrate to a depth of approximately one-third of the dentin thickness. Thus, the pulp has a pronounced sensitive innervation, which allows one to perceive sensations not only from the pulp, but also from the hard tissues of the tooth.
Functions of the pulp
The dental pulp performs a number of diverse functions. One of the most important factors for the development and life of a tooth is dentin formation. This function is directly provided by highly differentiated pulp cells - odontoblasts. The reserve for constant replenishment of odontoblasts is the poorly differentiated cells of the subodontoblastic layer.
The plastic function of the pulp is most actively and clearly manifested during tooth formation and continues after its eruption. When pathological changes occur in the hard tissues of teeth, for example, caries, the pulp responds to them with the formation of secondary irregular (replacement) dentin. Dentinogenesis continues as long as poorly differentiated pulp cells are capable of differentiating into odontoblasts. Under the influence of factors causing the development of the carious process, along with the formation of secondary irregular dentin, restructuring processes are observed in the dentin directly adjacent to the bottom of the carious cavity. They are accompanied by the active flow of mineral salts through Toms fibers into the dentinal tubules. As a result, obliteration occurs, i.e. complete closure of the lumen of some groups of dentinal tubules. This is the so-called transparent, sclerotic dentin, characterized by increased hardness. Increased deposition of lime salts during caries and increased tooth abrasion can be considered as a tooth reaction to the action of various harmful agents, which protects the pulp from irritation and infection.
The trophic function is important for the pulp; it provides nutrition to dentin and supports the vital activity of tooth enamel. The hard tissues of the tooth receive nutrients with transudate from the capillaries, through Toms fibers, which, branching and anastomosing, form a sap-bearing network. Neurohumoral processes in all dental tissues are regulated through the pulp, and their disruption can lead to dystrophic changes in dentin and enamel.
Pulp cells, especially odontoblasts, regulate the trophic function and regenerative capacity of dentin. The presence of elements of reticuloendothelial tissue (sedentary macrophagocytes) in the pulp increases its protective barrier function. It has been established that pulp cells have a high phagocytic ability, which prevents the penetration of microbes into the periapical tissues and inactivates them. This fact is confirmed by the active accumulation of cells in areas located directly at the apical foramina or at a short distance from them. On the one hand, the barrier function of the pulp is enhanced by the presence of hyaluronic acid in it, the astringent properties of which contribute to the retention of bacteria that do not have hyaluronidase-secreting ability. On the other hand, the pulp is rich in a capillary network of blood and lymphatic vessels, which enable the outflow of exudate. One of the features of dental pulp is the high absorption capacity of vascular endothelial cells, as one of the reserve physiological mechanisms of tissue protection, especially during inflammation of the pulp. The rich innervation of the pulp and its receptor apparatus also play an important protective role.
Dental pulp has a significant potential for regeneration as tissue of the vascular-connective tissue type. It contains a significant number of poorly differentiated cells that can quickly transform into highly differentiated protective cells and specific odontoblasts. An equally important role in this process is played by the rich blood supply and innervation of the pulp, and the high activity of metabolic processes in it. This leads to the fact that even with significant trauma, the pulp can remain viable and form a scar at the site of injury. These features of the structure and function of the pulp provide a specific clinical picture for inflammatory processes in it and lie at the forefront of the choice of treatment methods.
Age-related anatomy of the tooth cavity and age-related characteristics of the pulp
The dental pulp, from the tooth germ in a child to old age, undergoes completely natural changes in structure in accordance with a person’s age.
In childhood, when the roots have not yet formed, the entire pulp cavity is located in the crown of the tooth and has no bottom. Only with the growth of the roots does the coronal part of the cavity begin to gradually continue into the roots through the openings (mouths) of the canals.
A feature of the pulp of primary teeth is a clearly defined pattern of pulp horns, significantly larger dimensions of the tooth cavity than in permanent teeth, wider canals and apical foramen in relation to the crown of the tooth. In primary teeth, the branching of the root pulp is more pronounced, both in single-rooted and especially in multi-rooted teeth.
In baby teeth, the pulp is more massive in both the coronal and root parts, especially at the apex of the root, where at this time there is a wide apical foramen. The presence of a wide apical foramen in children’s teeth should be taken into account by clinicians, since this factor facilitates the penetration of infections and certain medications into the periodontium.
In children's teeth, additional root canals are observed that extend into the periodontium not only in the apex area, but also in the middle and in the bifurcation area of the tooth root, which contain vessels. Later they become empty and become obliterated.
With age, the configuration of the tooth cavity changes due to the constant deposition of new layers of dentin on the walls of the pulp cavity and root canals. In children's teeth, the cavity of the tooth crown is large, the root canals are wide. Dental cavities, in old age repeating the configuration of the cavity at a young age, are smaller in size and have narrower canals. The dental pulp in young people is represented by juicy, loose tissue, rich in young, poorly differentiated cells, present in all its layers; well supplied with nerve fibers, has a developed circulatory and lymphatic network.
Consequently, the anatomical and physiological data of the pulp in young people allow us to consider it as a tissue rich in reactive elements, possessing high vital activity and enormous protective and adaptive mechanisms.
With age, the dental pulp undergoes changes, which are manifested in a decrease in the number of cells and an increase in the volume of intercellular substance, which is often subject to sclerosis. Poorly differentiated cells remain in the pododontoblastic layer and are not detected in the central layer. Odontoblasts become vacuolated, and reticular degeneration of the odontoblast layer and then of the entire pulp tissue is observed, caused by the fact that in old age the processes of wear and death of cells are not balanced by the processes of their regeneration.
In the pulp, the level of microcirculation and metabolic processes sharply decreases, the tone and reactivity of the vessel walls decreases, their lumen decreases, the vessel walls become sclerotic, and pulp dehydration develops. Petrificates are often deposited along the vessels. All this leads to a decrease in the protective and regenerative properties of the pulp, which should be taken into account when choosing a treatment method for various forms of pulpitis.
ETIOLOGY AND PATHOGENESIS OF PULPTIS
Among a wide variety of dental diseases, inflammation of the dental pulp occupies from 14 to 25%. Despite the structural features, specificity of localization and function of the pulp, the process of inflammation in it should be considered from a standpoint that corresponds to the general pathophysiological and morphological patterns of the development of pathological processes in other structures of the human body. The nature of inflammation, its course, the dynamics of development are usually closely related, determined by different levels of reactivity of the body and occur predominantly with manifestations in which the processes of exudation, alteration or proliferation prevail.
Considering the physiological and pathophysiological properties of the pulp from a general perspective, characteristic of all connective tissue of the body, it is worth mentioning some of its features that influence the course of the emerging pathological process. Unlike other tissues, it is not covered with epithelium and is located in a closed formation of dentin. At the same time, the pulp has a specific function that is unique to it - dentin formation. This functional anatomy is provided by a complex of protective and adaptive mechanisms of the pulp, which determines the characteristics and nature of the course of inflammatory processes in it. These features become important in assessing the reserve capabilities of the pulp, especially assessing the choice of biological or surgical methods for treating certain forms of pulpitis in its generally accepted classifications.
Etiology of pulpitis
The inflammatory process in the pulp occurs in response to irritants that affect the pulp.
The prevailing etiological factors are usually microorganisms, their metabolic products - toxins, decay of organic matter of dentin, chemical, toxic substances of exogenous origin (acids, alkalis), temperature, mechanical, physical and other irritants.
Microorganisms.
The predominant cause of pulpitis occurrence is microorganisms. They can penetrate from an untreated carious cavity and when the filling does not adhere tightly to the hard tissues of the tooth, through periodontal pockets, as well as hematogenously.
Pulpitis is characterized by a polymorphic microbial flora with a predominance of associations of streptococci and other pyogenic cocci, putrefactive microbes, gram-positive bacilli, fusospirochetous flora and fungi. The most common associations are streptococci and lactobacilli, and less frequently - staphylococci. Typically, staphylococci and streptococci of inflamed pulp are microorganisms of increased virulence with significant sensitizing properties.
As a complication of caries, pulpitis always develops in the form of hyperergic inflammation against the background of previous sensitization of the pulp by decay products of the organic matter of dentin and endotoxins of microorganisms of the carious lesion. Infection can also enter the pulp through the arteries that enter the root canal. Hematogenous infection of the pulp can occur with influenza complicated by capillary toxicosis, osteomyelitis, etc. Inflammation of the pulp can develop in intact teeth due to the penetration of microorganisms from nearby infectious foci, retrogradely through one of the apical foramina.
Functions of the dental pulp
The main role of the pulp is to perform several tasks to support the vital functions of the tooth.
- Plastic function.
Formation of basic dentin, as well as the formation of hard tissue in case of damage. - Protective function.
Preventing infections from entering the periodontium through canals, removing dead cells, maintaining regeneration processes. - Sensory function.
A signal about the presence of an external or internal irritant to preserve tooth health. - Trophic function.
Supply of nutrients to dentin and tooth enamel.
What can cause pulpitis?
Burn of tooth pulp
As a rule, a pulp burn during tooth grinding occurs as a result of medical error or carelessness. Before prosthetics, the crown part is treated at high temperatures. Insufficient cooling during the preparation process can lead to a burn, which will provoke subsequent inflammation of the dental pulp.
Dental pulp hematoma
After a tooth injury, there is a possibility of getting a hematoma, that is, bleeding into the dentin. The crown acquires a reddish tint and painful sensations occur when pressure is applied. However, a bruise that has not turned into pulpitis or necrosis does not need treatment and goes away on its own over time.
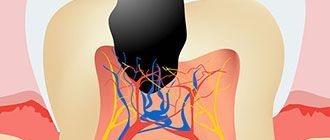
Caries
Through the smallest cracks in the tooth cavity, infection and pathogenic bacteria penetrate into the pulp. Advanced caries is one of the most common causes of pulpitis.
Any damage or complications of diseases can lead to disastrous consequences if left untreated. Dental pulp necrosis is the process of tissue death due to the spread of infected cells. The anomaly can be recognized by the grayish color of the tooth and incessant aching pain. During treatment, the doctor will perform depulpation, clean and seal the canals. |
Therapeutic methods for treating dental pulp
Therapeutic or conservative are methods of treatment that make it possible to do without removing tissue. These methods of preserving dental pulp are not available to all patients; there are certain indications:
- age not older than 40 years;
- deep caries;
- acute serous-purulent or fibrous pulpitis;
- opening of the dental pulp due to trauma;
- lack of medical intervention in the inflammation process to date.
As a rule, the dentist treats the surgical field with antiseptic solutions, removes the affected tissue and places the drug into the cavity. There are two methods for performing this procedure.
- Indirect covering of the dental pulp.
An antibacterial agent is placed at the bottom of the cavity to stimulate the production of bone substance. Regeneration occurs naturally. - Direct covering of the dental pulp.
The medication is applied directly to the soft tissue to preserve the viability of healthy cells, then isolated with a pad.
Next, the tooth is restored with temporary materials, and after a secondary examination, it is finally restored.
Histological analysis of the pulp in correlation with the carious process of varying depth
Determination of the inflammatory process in the pulp of primary teeth, caused by the development of caries, eludes clinical and radiological examination. Establishing an accurate diagnosis and identifying the inflammatory status of the pulp tissues in primary teeth allows us to select the correct treatment and ensure the success of restorative and endodontic therapy. This is especially important when working with young patients, since the limited ability to cooperate with them greatly complicates re-treatment.
Pulp inflammation in carious primary teeth is classified according to clinical signs and symptoms. However, in young children this inflammation cannot be absolutely reliable. Thus, we must rely largely on radiographic data. And the only unambiguous way to determine the status of pulp inflammation is histopathological examination.
Treatment of caries in children is not very simple due to unclear objective data that are necessary to make a correct diagnosis. And all manipulations on baby teeth must be justified and justified. All possible techniques such as indirect pulp capping, pulpotomy, pulpectomy and extraction must be justified by the presence of certain inflammatory changes in the pulp. Currently, there is insufficient literature on the correlation of signs, symptoms and histopathological status of the pulp in caries of primary teeth, which raises the problem of choosing the right treatment method.
Therefore, the present study aims to evaluate data on the histopathological status of the pulp obtained from the study of the second primary molar involved in the caries process. Histological parameters correlate with clinical and radiological data.
Materials and methods
A simple pilot study was conducted on 44 children aged 6 years and younger without serious general health problems. The study was conducted at the University Dental Hospital Sharjah (UDHS). The selected teeth were suitable for restoration and had less than 1/3 root resorption with no radiographic evidence of calcification, internal or external resorption. Upper and lower second primary molars with caries on the occlusal (22 teeth) and contact (22 teeth) surfaces. The study was conducted after obtaining approval from all necessary committees in accordance with the Declaration of Helsinki. The children's parents were informed about the study and gave written consent.
Children found themselves at the pulpit 2 weeks after the first signs of pain. Nine children reported 2-3 days after the onset of pain, and the remaining participants reported persistent pain for more than 10 days. Clinical examination of the selected teeth showed relatively strong hard tissue and healthy surrounding gingiva. Intraoral targeted radiography was performed to determine the percentage of caries involvement, total hard tissue thickness, residual dentin density (RDT), and periapical pathology. All indicated indicators were determined on a scale and then verified by an independent researcher, so all data can be considered accurate and reliable. The depth of caries was assessed as a percentage of the total dentin thickness.
Clinical procedures included local anesthesia, rubber dam isolation, removal of carious tissue, opening of the pulp chamber, and amputation of the coronal pulp with a spoon elevator. The bleeding was stopped by pressing a cotton swab soaked in saline solution for 5 minutes. After which the root pulp was removed using pulp extractors. After the pulpectomy procedure, tooth restoration was performed in one visit. The removed pulp tissue was placed in a 10% buffered formalin solution and sent for histopathological examination.
Pulp tissue samples were embedded in paraffin and then cut. Preparation for painting was carried out in two stages. The cut ran parallel to the longitudinal axis to a thickness of 5 mm. Hematoxylin-eosin was used for staining, which helps determine the type of inflammatory cells, vascular proliferation and fibrosis. To confirm the hematoxylin-eosin staining data, Masson trichrome staining (for fibrosis) and immunohistochemistry for CD (cluster differentiation) 45 leukocyte antigen and CD 34 endothelial marker (DAKO, Denmark) were performed. The degree of pulp inflammation for CD45 was defined as follows: 0=normal, + (mild) 1-50 cells/20 HPF, ++ (moderate) 51-100 cells/20 HPF, +++ (severe) >100 cells/20 HPF . CD34 was defined as + up to 50 blood vessels with inflammatory infiltrate/20 HPF, ++ 51–100 blood vessels with inflammatory infiltrate/20 HPF, and +++ > 100 blood vessels with inflammatory infiltrate/20 HPF. Lymphocyte counting was performed using an Olympus BX51 microscope (Hamburg, Germany). The extent of fibrosis is respectively labeled as mild, moderate, and extensive based on collagen density in Masson trichrome-stained sections. The number of cells/20 HPF was counted by an assistant, and accuracy was checked by repeat counting after a period of time. The obtained data were analyzed by Student's t-test to compare histological types of inflammation with clinical parameters. P<0.05 was accepted as significant.
results
The children were 6 years old or younger. An assessment was made of 22 teeth with occlusal and contact caries. The extracted pulp from the upper and lower primary second molars of 44 children was prepared and sent for histological analysis. A correlation was made between histological data and clinical parameters.
The results showed different histological conditions of the pulp depending on the degree of carious lesions of the occlusal or contact surfaces. All samples were grouped depending on the nature of the inflammatory process. Group A was a focal or diffuse inflammatory infiltrate consisting primarily of neutrophils interspersed with varying numbers of lymphocytes, plasma cells, and occasional eosinophils (Figure 1). The remaining groups (B1, B2 and C) showed mild to severe chronic inflammation represented by lymphocytes, macrophages, plasma cells along with blood vessel proliferation and varying degrees of fibrosis (Figure 2). Groups B1, B2 and C were divided based on the extent of fibrosis and angiogenesis. Histological parameters of the coronal and root pulp were the same in all cases except group A. In group A, severe acute inflammation was detected in the coronal and relatively moderate in the root.
Photo 1: Histological sections from group A showing signs of acute inflammation in the form of infiltration of neutrophils, varying numbers of macrophages, lymphocytes and plasma cells scattered around dilated blood vessels (a: hematoxylin-eosin staining/20 HPF Olympus BX51) and the same section stained CD45 antigen staining (b)
Figure 2: Histological sections from group B with chronic inflammation represented by moderate infiltration of lymphocytes and plasma cells, angiogenesis and fibrosis (a: hematoxylin-eosin/20 HPF Olympus BX51 stain) and the same section stained with leukocyte antigen CD45 (b) stain CD34 of blood vessel endothelium (c) and fibrosis stained with Masson trichrome (d).
In nine cases, when patients were examined 2-3 days after the onset of pain, signs of acute inflammatory changes were found, while in the remaining cases, except one, the pulp passed into the stage of chronic inflammation.
All children who sought help complained of pain, while healthy gum tissue was clinically determined, and tooth mobility in all cases was within physiological limits. Spot radiography revealed minimal changes in the periapical tissues. Carious lesions >80% and residual dentin thickness <1 mm were associated with varying degrees of pulp inflammation. We did not find any significant difference (p>0.05) between the histological type of inflammation and the clinical parameters assessed in this study.
Discussion
Histopathological examination was performed on pulp collected from primary second molars of children less than 6 years of age. The age criterion was chosen in order to completely exclude the influence of physiological resorption on the development of the inflammatory process.
Teeth in which pain was characterized as spontaneous were selected for the study. While the criterion for selection during examination in the oral cavity was healthy gums and dense hard tissues, which could indicate the vitality of the tooth. X-ray examination helped to exclude such pathologies as internal and external resorption, as well as calcification of the pulp chamber.
The pulp of the selected teeth was then sent for histopathological examination. Next, the samples were divided into groups according to the type of inflammation: acute and chronic. We observed histological signs of pulpitis in all cases. In 10 cases it was acute pulpitis, in the rest - varying degrees of chronic inflammation. The nature and severity of inflammation was similar in the coronal and root pulps in 40 cases, however, in 4 cases, acute severe inflammation was recorded in the coronal pulp and only moderate inflammation in the root pulp. For the first time in this study, we report that the histological type of inflammation (acute or chronic) influences the development of certain symptoms and clinical presentation.
All selected teeth exhibited symptoms of pain from irreversible pulpitis, intraoral examination revealed healthy gingiva, and tooth mobility was within physiological parameters. Thus, the children who took part in the study suffered from acute and chronic pulpitis, the form of which depended on the age of onset of the disease. Lack of mobility and swelling of the gums were criteria for excluding non-vital teeth from the study. The presence of periapical changes indicated the transition of infection from the coronal pulp to the furcation zone and the beginning of microscopic root resorption.
X-ray assessment of the extent of the carious process on the occlusal and contact surfaces showed from 80 to 100% of the total dentin thickness, which histologically corresponded to an acute inflammatory process in 10 images and a chronic one in the rest. The data obtained are in agreement with previous studies comparing the response of the pulp to the carious process. RDT was between 0.25 mm and 1 mm in 24 samples; in other cases, the carious process penetrated into the pulp chamber. The RDT score was used as an objective assessment of the likely pulpal response. We noted that the RDT value in this study was associated with inflammatory changes in the pulp tissue.
Correlations of the clinical manifestation of caries in the form of a cavity of 1-5 mm histologically corresponded to acute and chronic changes in the pulp. It should also be noted that caries assessed radiographically in 80% of cases clinically appeared less widespread. Thus, only a clinical assessment of a carious cavity cannot be considered a reliable guide for choosing a treatment method; in addition, it is necessary to evaluate the x-ray picture and clinical manifestations. It is also interesting that a 1 mm defect in the proximal zone in two clinical cases was associated with acute inflammation, which may indicate rapid progression of caries in a very short period of time.
The correlation of histological parameters with clinical manifestations confirmed the validity of the chosen treatment method (pulpectomy in one visit). From the results obtained, we can hypothetically conclude that a temporary molar with a carious cavity of less than 80% of the volume of the entire tooth, with an RDT of more than 1 mm, the absence of periapical changes, pain, dense hard tissues and healthy gums can be effectively treated only by the method of gradual excavation.
Conclusion
Temporary second molars with carious lesions of more than 2/3, with symptoms of pain, histologically show inflammation of the coronal and root pulp in all cases. Considering the clinical and radiological parameters, single-visit pulpectomy is considered the optimal treatment option in this situation.
Authors: Vellore Kannan Gopinath , General and Specialist Dental Practice, College of Dentistry Khurshid Anwar , Basic Medical Sciences, College of Medicine, University of Sharjah, Sharjah, United Arab Emirates
Surgical methods for treating dental pulp
In cases where therapeutic methods are powerless, the only option left is to remove the dental pulp. This option is used in cases where the patient’s immunity is weakened, the disease is at an acute stage, or the tooth will be used in the future as a support for prosthetics. Surgery involves amputation or extirpation of the dental pulp.
- Amputation of the dental pulp
- during the procedure, only the coronal part is removed. Prescribed for acute pulpitis or mechanical damage to the dental pulp. - Extirpation
is the complete removal of the pulp. Used for all forms of pulpitis.
The pulp can be removed vitally, that is, under anesthesia without prior killing. If this method is not possible, the doctor resorts to devitalization of the dental pulp - the toxic substance is left in the cavity for about a day, after which the dead tissue is painlessly removed. Means for devitalizing dental pulp include arsenic or paraformaldehyde paste.