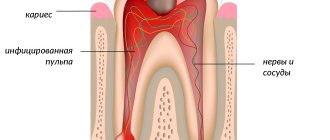
Anatomically, a tooth consists of three parts:
- crown
- neck
- root
There is a cavity inside the crown and root. The pulp is localized in these cavities. The part of the pulp that is in the crown is called coronal, and in the root is called root.
The pulp itself consists of nerve endings, blood vessels and lymphatic vessels.
The pulp is the nerve of the tooth, together with blood and lymphatic vessels, providing the tooth with nutrients.
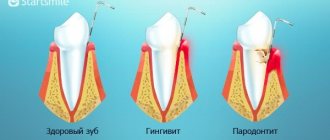
Inflammation of the pulp is called pulpitis.
Causes of pulpitis
The causes of pulpitis are varied. Bacterial infection comes first. Bacteria enter the pulp through carious cavities, through dentinal tubules after preparation, when taking an impression under pressure, as well as microbes entering through the apical foramen (infection of the pulp through the apical foramen), for example, in case of sepsis, osteomyelitis, after curettage of deep periodontal pockets, etc. d.
Irritation and trauma during the treatment of caries and during the preparation of teeth under fixed dentures, the toxic effect of filling material, dental trauma due to a fracture or crack of a tooth.
Results and discussion
We determined the antimicrobial effect of the Biodentin cement extract against E. coli
— the zone of growth retardation was 17 mm
(Fig. 2)
Rice.
2. Determination of the antimicrobial activity of aqueous extracts from materials. , in the control group (0.05% chlorhexidine solution) - 34 mm. No antimicrobial effect was detected in samples 1 (Futurabond NR) and 3 (Rutdent). In the control group (0.05% chlorhexidine solution), antimicrobial activity was determined against all types of microorganisms: E. coli, S. aureus, C. albicans, St.
faecalis .
To confirm the antimicrobial properties of Futurabond HP and Rutdent materials, another series of experiments was carried out using the above-described method. From the listed materials, using a special template, samples were made in the form of tablets with a diameter of 10 mm and a thickness of 2 mm (Fig. 3)
.
Rice. 3. Determination of the antimicrobial activity of tablet sample materials.
All samples submitted for testing had antimicrobial activity (see Fig. 3)
.
In relation to S. aureus,
the highest activity was found in Rutdent cement (22 mm), the lowest in Biodentin cement (18 mm) and Futurabond NR adhesive (17 mm).
For all presented materials, the antimicrobial effect was lower than in the control group (27 mm). The highest activity against E. coli
was observed for the Futurabond NR adhesive (24 mm) and Rutdent cement (22 mm); for the Biodentin material (15.5 mm), this figure was slightly lower compared to the two previous materials.
Antimicrobial activity against C. albicans
was quite high for the Futurabond HP adhesive (24 mm).
Biodentin (15.5 mm) and Rutdent (14 mm) cements have comparable antimicrobial activity indicators and are much lower than the control indicator (22 mm). When determining the degree of antimicrobial effect on the culture of St.
faecalis, high activity was noted for all tested samples, especially for Rutdent cement (25 mm). For Futurabond NR adhesive and Biodentin cement, the results are equivalent (23 mm), these indicators significantly exceed the level of activity in the control group (0.05% chlorhexidine solution) - 15 mm.
When studying the genotoxic properties of materials, we first assessed the level of spontaneous DNA damage in single cells of normal human embryonic fibroblasts (Fig. 4, see color insert)
Rice.
4. Control; digital image from a microslide; human embryonic fibroblasts. Here and in Fig. 5-8: DNA staining with ethidium bromide 2 μg/ml, uv. 300. and when exposed to a pharmacopoeial sample of H2O2 (Fig. 5, see color insert)
Rice.
5. Positive control (H2O2); digital image from a microslide; human embryonic fibroblasts. . The amount of DNA damage in the control group was 0.92±0.16% TDNA. Exposure to hydrogen peroxide at a concentration of 0.3 mmol led to increased DNA damage in cells (13.89±0.77% TDNA). Normally, the damage index should not exceed 2.5. When analyzing the study results, no statistically significant differences were revealed between the groups (Fig. 6-8, see color insert)
.
Rice. 6. Biodentine (“Septodont”); digital image from a microslide; human embryonic fibroblasts.
Rice. 7. Rutdent (“TehnoDent”); digital image from a microslide; human embryonic fibroblasts.
Rice.
8. Futurabond (“Voco”); digital image from a microslide; human embryonic fibroblasts. All studied samples did not have a genotoxic effect on cell DNA, regardless of the concentration and incubation time (Fig. 9, 10)
.
Rice. 9. Genotoxicity of the studied materials on human embryonic fibroblast cell culture (incubation - 3 hours).
Rice. 10. Genotoxicity of the studied materials on human embryonic fibroblast cell culture (incubation - 24 hours).
When studying cytotoxicity, it turned out that when the materials under study are kept in the culture medium DMEM/F12 10% FTS for a day, a change in the acidity of the medium occurs: it is alkalized with the materials Rutdent and Biodentin and acidified with the material Futurabond HP (Fig. 11, see color insert)
.
Rice. 11. Changing the pH of the environment when preparing extracts from materials. 1 - Rudent; 2 - Biodentine; 3 - Futurabont. According to the MTT test, when diluted 1/2, extracts from the materials Rutdent, Biodentin and Futurabond HP have an inhibitory effect on the metabolic activity of cells of the NCTC L929 line, the most pronounced in Biodentin cement, the least - in the Rutdent material. With a dilution of extracts of 1/10, the inhibitory effect is the same as with a dilution of 1/2; it was found only in Rutdent cement. For the materials Biodentin and Futurabond HP, at a dilution of 1/10, the results are equivalent and slightly lower than in the control. At a dilution of 1/50, Biodentin showed the best results in terms of cytotoxicity; for all materials they are comparable to the control group (Fig. 12)
.
Rice.
12. Viability of NCTC L929 cells according to the MTT test when diluting extracts from materials: 1 - 1/2; 2 - 1/10; 3 - 1/50. When studying the adhesion and growth activity of mouse embryonic fibroblasts on the surface of materials, the absence of adhesion and cell growth on the Rutdent sample was revealed (Fig. 13, see color inset)
Figure 13. Fig.
13a. Appearance of primary MH cells growing on the surface of the Rudent material. 1st day of incubation. Figure 13. Fig. 13b. Appearance of primary MH cells growing on the surface of the Rudent material. 5th day of incubation. , low degree of spreading in the absence of cell growth on the surface of Biodentin and Futurabond HP materials on the 1st and 5th days of incubation (Fig. 14, 15, see color insert)
. Figure 14. Fig. 14a. Appearance of primary MH cells growing on the surface of the Biodentin material. 1st day of incubation. Figure 14. Fig. 14b. Appearance of primary MH cells growing on the surface of the Biodentin material. 5th day of incubation. Figure 15. Fig. 15a. Appearance of primary MH cells growing on the surface of the Futurabont material. 1st day of incubation. Figure 15. Fig. 15b. Appearance of primary MH cells growing on the surface of the Futurabont material. 5th day of incubation.
Thus, the cements Biodentin (“Septodont”), Rutdent (“TehnoDent”) and the Futurabond HP adhesive (“Voco”) have antimicrobial activity and do not have a genotoxic effect or an inhibitory effect on metabolic activity when diluted 50 times. Futurabond HP adhesive had the greatest antimicrobial activity against all control strains of microorganisms, and Biodentin cement had the least. All tested samples did not have a genotoxic effect on cell DNA. When assessing the cytotoxicity of materials, Biodentin cement showed the best results, since it caused alkalization of the environment, stimulating the odontotropic effect, and did not have an inhibitory effect on the metabolic activity of cells at lower dilutions. The results of laboratory studies allow the use of Biodentin cements (Septodont), Rutdent (TehnoDent) and Futurabond HP adhesive (Voco) in the treatment of deep carious lesions of dentin and initial forms of pulpitis.
Types (classification) of pulpitis
In 1989, the MMSI proposed the following classification of pulpitis:
1. Acute pulpitis:
- a) acute focal pulpitis;
- b) acute diffuse pulpitis.
2. Chronic pulpitis:
- a) chronic fibrous pulpitis;
- b) chronic hypertrophic (proliferative) pulpitis;
- c) chronic gangrenous pulpitis.
3. Exacerbation of chronic pulpitis.
In Russia, the transition to ICD-10 was carried out in all health authorities and institutions in 1999.
The diagnosis is indicated according to ICD-10. In brackets you can indicate the corresponding form of pulpitis according to MMSI.
Classification of pulpitis according to ICD-10
- K04 – diseases of the pulp and periapical tissues
- K04.0 – pulpitis
- K04.00 – initial (pulp hyperemia), and (according to MMSI deep caries)
- K04.01 – acute (according to MMSI acute focal pulpitis)
- K04.02 – purulent (pulp abscess), (according to MMSI acute diffuse)
- K04.03 – chronic (according to MMSI chronic fibrous pulpitis)
- K04.04 – chronic ulcerative pulpitis (according to MMSI chronic gangrenous pulpitis)
- K04.05 – pulp polyp (according to MMSI – chronic hypertrophic (hyperplastic) pulpitis)
- K04.08 – other specified pulpitis
- K04.09 – pulpitis, unspecified
- K04.1 – pulp necrosis (pulp gangrene)
- K04.2 – pulp degeneration (denticles, pulp petrification)
- K04.3 – improper formation of hard tissues in the pulp (secondary or irregular dentin)
How to prepare a child for treatment?
Treatment of pulpitis of primary teeth in children is a rather complex task, so it’s great if the child is already familiar with the dentist’s chair. The first visit should be preventative - to familiarize yourself with the office environment, the doctor, and the instruments.
Also, the task of parents is to psychologically prepare the child. Required:
- talk to your child about doctors in a positive way - tell them that the dentist treats teeth and makes sure they don’t hurt;
- play dentist with toys and other family members;
- avoid mentioning pain or unclear, scary terms;
- do not deceive the child - explain that dental treatment may not be very pleasant, but it will not last long and the tooth will no longer hurt;
- remain calm, act gently but confidently if the child resists treatment;
- choose a suitable time for visiting - it is better in the morning, when the baby is alert and active;
- take a toy with you to calm the child;
- give the doctor the opportunity to establish contact with the small patient - do not rush him;
- Do not scare the child under any circumstances, do not threaten, do not blackmail.
If the situation cannot be controlled completely, you will have to reschedule the appointment for another day. However, the disease should not be ignored - treatment of pulpitis of baby teeth in children must be carried out one way or another. In special cases, treatment under general anesthesia may be considered, but this should be discussed with your doctor.
Clinical picture of initial K04.00
There is no history of spontaneous pain. When interviewed, it turns out that pain comes from various irritants, which quickly goes away after they are eliminated. A painful attack is provoked by cold and hot stimuli (temperature). Almost always the patient points to the causative tooth.
Pain from temperature stimuli quickly (within a few seconds) goes away. When talking with the patient, it turns out that the tooth has not hurt before.
- The tooth cavity is not opened.
- Percussion is painless.
- Probing is painful at one or more points.
- Electroodontometry - 10-12, and sometimes 20 microns (normally 2-6 microns).
- X-ray – no changes.
Diagnostics
Diagnosis of pulpitis takes place in several stages. The first is an examination of the oral cavity by a dentist. The patient's complaints about acute pain, the presence of injury or a carious cavity are taken into account. All this points to pulpitis. But it is impossible to determine the acute and chronic forms of the disease by one visual examination.
To determine the stage and type of pathology, the patient is prescribed an examination:
- X-ray.
- EDI or electroodontodiagnosis. This method allows us to identify the reaction of the pulp to the influence of electric current.
- Rheodentography. It is carried out to assess the blood supply to the dental pulp.
- Thermal test.
To make an accurate diagnosis, differential diagnosis of acute pulpitis is important. This is important so as not to confuse it with other diseases that have similar manifestations.
Treatment of initial K04.00 (pulp hyperemia),
For initial pulpitis, conservative treatment is carried out.
Mostly preparations containing calcium hydroxide are applied to the bottom of the cavity, and then filled with permanent fillings, it is better to monitor after three months.
Clinical picture of acute K04.01 (according to MMSI acute focal) pulpitis
- Complaints: prolonged pain from all irritants, mainly at night. There are also spontaneous pains.
- The pain is clearly localized, the light intervals can last for several hours, and later these light intervals become shorter.
- When the chewing teeth (molars) are inflamed, pain during an attack can spread (radiate) to the ear, temple, and teeth of the opposite side (antagonist teeth).
- Inspection - deep carious cavity, a lot of softened dentin, which, when removed, can open the pulp chamber.
- Percussion is painless
- EDI – 25-40 or within normal limits
- Probing is painless
When should you visit a dentist?
The sensitivity of the neurovascular bundle of a tooth in a child is lower than in an adult, so the symptoms of its inflammation may be erased or absent altogether. It is important to contact a pediatric dentist when the first symptoms of caries appear - a dark spot on the tooth, or the child complains of pain. You should hurry up with your visit if:
- severe pain;
- increased pain when eating hot or cold food/drinks;
- bad breath;
- elevated body temperature;
- inflammation of the gums around the tooth;
- darkening of the enamel.
Treatment of acute K04.01 (according to MMSI acute focal) PULPTIS
The first thing you need to do is stop the inflammatory process, that is, stop the inflammation.
First, painkillers are prescribed to reduce or relieve pain.
First way.
In young people, at the beginning of the inflammatory process, it is possible to stop the inflammatory processes and preserve the pulp using conservative processes. To do this, the carious cavity is prepared with modern instruments that are available in our clinic, and then
is treated with medication and an anti-inflammatory, regenerating and odonotropic paste is applied, mainly based on calcium hydroxide paste for 4-6 days, and then if there are no complaints, the tooth is filled with permanent fillings.
Second way
When performing this method, first infiltration or conduction anesthesia is carried out, and then the softened tissues of enamel and dentin, as well as the inflammatory pulp at the level of the canal mouth are removed with a diamond bur, then the tooth cavity is cleaned, the bleeding stops and a paste based on calcium hydroxide is applied without any pressure. And ionomer cement is applied to it. The first control after three, and the next controls after 6 months and 1 year.
This method is called vital pulp amputation or pulpotomy .
Clinical picture of acute purulent K04.02 (pulp abscess) (according to MMSI acute diffuse) pulpitis.
- spontaneous pain;
- prolonged pain with short light intervals;
- radiating pain along the branches of the trigeminal nerve;
- intense, unbearable pain;
- increased pain from hot foods;
- short-term relief of pain from cold;
- EDI 30 – 50 mA;
- deep carious cavity with a large amount of softened dentin;
- the tooth cavity is not opened;
- probing is painful;
- percussion is painless;
- palpation of the transitional fold at the level of the inflammatory tooth is painless, but may be sensitive;
- with unformed root apices, percussion and palpation are painful;
- Severe swelling and disturbances in the general condition of the whole body may be observed.
- X-ray – no changes;
Material and methods
The study of antimicrobial activity was carried out in a microbiological laboratory. Two series of experiments were carried out. Aqueous extracts and samples in the form of tablets made according to a special template were studied. Control strains of microorganisms Escherichia coli, Staphilococcus aureus, Candida albiсans, Streptococcus faecalis
.
The results were recorded after 24 hours, measuring the zone of growth inhibition around the hole (Fig. 1, see color insert)
.
Rice.
1. Zones of growth inhibition (mm) around the hole when studying the antimicrobial activity of materials. An aqueous solution of 0.05% chlorhexidine solution served as the control. To assess genotoxic properties using the DNA comet method, a culture of human embryonic fibroblasts was used as a test object. Testing of the test samples was carried out at 37 °C and 5% CO2 after 3 hours and 24 hours. The test samples were tested at 2 concentrations: 2.0 and 5.0 mg/ml. Pharmacopoeial hydrogen peroxide (Galeno Pharm, Russia) at a concentration of 0.3 mmol was used as a positive control. The percentage of comet tail DNA (CTDNA) was used to determine the DNA damage index. Statistical analysis was performed using Student's t test ( p
<0,05).
Cytotoxicity was assessed using aqueous extracts from the materials and the materials themselves. Mouse fibroblasts of the NCTC L929 line were used in the experiment; the seeding cell concentration was 10 thousand/cm2. Extracts were added 1 hour after cell attachment in dilutions of 1/2, 1/10, 1/50, 4 wells per dose, followed by cultivation in DMEM/F12 10% FBS at 37°C for 1 day. To study the adhesive characteristics of materials and their ability to support the proliferative activity of cells, we used a primary culture of mouse fibroblasts (MF), obtained from the skin-muscle tissue of 13-day embryos of mice of the C57BL/6-Tg(ACTbEGFP)1Osb/J line, transgenic mice with the gene reporter encoding the synthesis of enhanced green fluorescent protein (EGFP) under the control of the chicken beta-actin promoter. On the 1st and 5th day of incubation, the morphology of cells cultured on the surface of the materials under study was assessed using an Axiovert 200 fluorescence microscope.