In response to injury to body tissue, a complex mechanism is launched to restore the previous functioning and integrity of organ systems. This process is called tissue regeneration. There are three stages in the development of this mechanism. Their duration is individual for each person and directly depends on his age and the state of the immune system.
The prognosis for the healing time of a particular injury is also made based on observations of the nature of the injury and depends on the degree of its severity. All types of wounds are divided into two types according to the depth of damage:
- Simple - the integrity of the skin, adipose tissue, and the structure of adjacent muscles is compromised.
- Complex wounds are characterized by damage to internal organs, large veins and arteries, and bone fractures.
The stages of regeneration are the same for any damage, regardless of its origin and type.
Author of the article / Site experts Shulepin Ivan Vladimirovich, traumatologist-orthopedist, highest qualification category
Total work experience over 25 years. In 1994 he graduated from the Moscow Institute of Medical and Social Rehabilitation, in 1997 he completed a residency in the specialty “Traumatology and Orthopedics” at the Central Research Institute of Traumatology and Orthopedics named after. N.N. Prifova.
Introduction
Treatment of purulent-necrotic lesions of the lower extremities is one of the pressing problems of surgery, diabetology and phlebology. If metabolic disorders can be normalized by appropriate conservative therapy, then anatomical changes can only be corrected surgically. For quite a long time, early, free autodermoplasty was considered the method of choice for treating long-term non-healing wounds and ulcers. However, often such tactics were not successful due to rejection or necrosis of the skin flap. Failures of skin-plastic interventions can be due to numerous reasons, the main of which are considered to be insufficient preparation of the receiving bed, a decrease in the reparative capabilities of the body, including due to diabetes and the elderly age of patients. The state of microcirculation in the affected limb also plays a very significant role, without improving which it is impossible to count on a positive result. In scientific surgical publications in recent years, much attention has been paid to the problem of treating purulent-necrotic complications of diabetic foot syndrome. In this regard, issues of restoring regional hemodynamics, timing and scope of surgical interventions are considered. One of the methods for eliminating wound defects of the lower extremities in patients is autodermoplasty with a split skin flap .
Questions about the timing of autodermoplasty, the validity and duration of preoperative preparation, improvement of regional hemodynamics, preparation for autodermoplasty of the receptive bed and donor skin area remain completely unresolved.
Since 2006, a large amount of material has been accumulated on this problem, which is summarized in the article.
Phases of regeneration of damaged tissues
During the healing process, a wound goes through several stages:
- Inflammation - When epithelial cells are damaged, the body activates a natural mechanism to stop bleeding as quickly as possible. The resulting blood clots clog the damaged vessels, eliminating extensive bleeding. A large number of leukocytes, which have a bactericidal effect, are sent to the wound site.
- Granulation - 5-6 days after the formation of the wound, the granulation mechanism is activated, due to which new epithelial cells are formed. This process takes at least a month, after which the wound is covered with scar tissue.
- Epithelization - granulation tissue gradually dies, and new epithelial cells form under it.
Granulation of wounds occurs in stages and consists of six processes that transform into each other:
- Superficial leukocyte-neocytic layer - consists of light gray or greenish neoplasms located on the surface of the wound.
- The surface layer of vascular loops - new capillaries are formed with it, which will subsequently fill the wound site.
- The vertical vascular layer ensures the restoration of metabolic processes in damaged tissue areas.
- The maturing layer of the epithelium has a light pink color with a characteristic shine.
- A layer of horizontally located fibroblasts provides maximum protection of the wound surface from the penetration of pathogenic microorganisms, as well as from additional injuries.
- The fibrous layer is the densest and precedes the formation of a scar.
The period of granulation lasts individually for each person. In some cases, complete healing takes no more than 3 weeks, while in others it takes about a year.
Material and methods
The work is based on an analysis of the treatment of giant (more than 50 cm²) trophic ulcers of the lower extremities in diabetes mellitus (27 patients), chronic venous (32 patients) and arterial (24 people) insufficiency from 2009 to 2013. The comparison group consisted of 60 patients comparable in age, type of pathology and concomitant pathology, treated using traditional methods. The average age was 69±3.7 years. Microcirculation of the ulcer surface was measured using an Easy-LDI device (Switzerland). Preoperative preparation of the wound bed was carried out using vacuum therapy, ultrasonic cavitation and targeted lymphotropic antibiotic therapy. The autoskin was collected using a disk dermatome, followed by perforation of the flaps. The study of microcirculation of the wound bed in our patients was carried out using laser Doppler imaging using an LDI device from AIMAGO (Switzerland). LDI technology (LaserDoppler Imaging), in Russian literature - laser Doppler visualization, allows for non-contact observation of microblood flow over an area of 100 cm², with a depth of the probed layer of up to 2 mm, instantaneous video recording of the study and the possibility of measurements at several nearby points at once. Moreover, the technical study is so simple that it can be performed by nursing staff, since reproducibility practically does not depend on the qualifications of the researcher. The resulting image was analyzed in real time.
The method of using a diaper for vacuum therapy is as follows. A sterile gauze bandage is applied to the wound surface. A diaper is placed on top of it (Fig. 2). Moreover, the latter is applied entirely, with a hygroscopic surface to the skin, preventing diaper rash and its maceration.
A silicone Nelaton catheter No. 14 is placed between the diaper and the sterile bandage along the plantar part of the foot with a transition to the back of the lower third of the leg. This placement improves the outflow of wound fluid when the patient is in a horizontal position. A bag is placed over the diaper to collect medical waste. In the upper third of the leg it is fixed to the skin with adhesive medical film. The free end of the Nelaton catheter is removed through a puncture in the lower corner of the bag, sealed and connected to the suction (Fig. 3).
The perforation hole in the bag is sealed with adhesive tape. A comparative analysis of the use of foam rubber and a diaper was carried out in groups of patients with purulent wounds in the phase of severe exudation in patients with diabetes mellitus. In all respects, the use of a diaper turned out to be preferable. Having the same absorption capacity, the skin under it is not wet or macerated; the cost of the diaper is 2 times cheaper than foam rubber. These circumstances prompted us to use diapers in the method of using vacuum therapy. The effectiveness of vacuum therapy of a purulent wound was assessed using microcirculation indicators (laser Doppler imaging - LDI) and recording tissue edema by measuring the diameter of the lower leg in the middle third. The results of the study are presented in table. 1.
Table 1. Changes in microcirculation parameters and reduction in swelling of a purulent wound under the influence of vacuum therapy
| Measurement parameters | Before vacuum therapy | After vacuum therapy | R |
| Microcirculation indicators | 4.7±2.5 apu | 10.3±1.7 apu | p ≤ 0.05 |
| Shin circumference in the middle third | 32.4±2.7 cm | 27.1±1.4 cm | p ≤ 0.05 |
It follows from the table that vacuum therapy improves microcirculation of affected tissues by 54.4% and reduces tissue swelling by 25.7% due to the removal of intercellular fluid. This promotes early clearance and development of granulation tissue, which ultimately speeds up wound healing.
The study was conducted on 30 patients (16 men, 14 women). Average age: 64±12.5 years. Microangiopathy of atherosclerotic origin - in 10 patients, diabetic - in 10 patients, phlebological - in 10.
Dynamic monitoring of microcirculation parameters allows for timely correction by selecting a negative pressure mode, using drug therapy, etc. The study showed that the film coating does not distort the results of microcirculation studies when passing a laser beam.
Immediately before applying the perforated autodermal flap, the receptive bed was treated with an antiseptic, taking into account the sensitivity of the flora of the wound surface using ultrasonic cavitation (Fig. 5, 6).
Then, using a disk dermatome under local anesthesia with a solution of novocaine 0.5% (80.0), autoskin was taken (Fig. 7), perforated (Fig. and transplanted onto the granulating tissue of the ulcer surface (Fig. 9)
and transplanted onto the granulating tissue of the ulcer surface (Fig. 9)
The figure shows that with an increase in microcirculation indicators, the proportion of autograft engraftment increases, and in patients with diabetes mellitus it is somewhat slower, apparently, this is due to more pronounced damage to the microvasculature in this pathology. The optimal indicators of microcirculation of granulation tissue guaranteeing the healing of autoskin were values from 14.3±1.17 apu to 16.5±1.5 apu.
Independent closure of giant trophic defects of the lower extremities is very problematic and usually ends in a rough keloid that disfigures the leg and impairs the function of the lower extremities. The use of autodermoplasty greatly simplifies this task. The use of our technique of this surgical aid in the treatment of gross defects of the lower extremities showed a significant advantage over traditional methods (Table 2).
Table 2. Indicators of autoskin engraftment during the closure of ulcerative defects in giant trophic ulcers in the main and control groups, %
| Disease | Main group | Control group |
| Diabetes mellitus n-20 | 93±3,7* | 54±8,3* |
| KHOZANKn-10 | 87±4,1* | 67±4,8* |
| ХВНn-10 | 80,1±2,8* | 71±3,2* |
* — p ≤ 0.005
Granulation of wounds as a protective reaction of the body
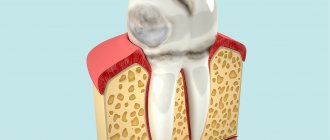
Wound granulation is one of the stages of skin regeneration, as a result of which temporary tissue is formed that protects the boundaries of the wound. When healing is complete, the granulation tissue disappears and the wound becomes covered with scar tissue.
The active process of granulation develops up to 5-6 days, and its duration depends solely on the degree of tissue damage and the individual characteristics of the body.
The following cell types are involved in the granulation process:
- Leukocytes - eliminate pathogens that have entered the surface of the wound.
- Plasmocytes - activate the production of substances and blood clotting factors, which helps accelerate the process of blood clot formation.
- Mast cells - help speed up the regeneration of damaged cells.
- Fibroblasts control the synthesis and transport of collagen cells, through which the process of regeneration of damaged tissue occurs.
What does wound granulation look like?
Externally, granulation looks like a thin layer covering the wound surface. It has a delicate pink color with a characteristic mirror shine. Within a month, granulation ends, after which a thin layer peels off, and dense scar tissue forms underneath it.
Bibliography
- Glukhov A. A., Aralova M. V. Epidemiology of venous trophic ulcers. 2nd international congress dedicated to the 70th anniversary of the Institute of Surgery named after. A. V. Vishnevsky. "Wounds and wound infection." With. 113–114.
- Davydov Yu. A., Larichev A. B. Vacuum therapy and wound process. Yaroslavl. 1995.
- Duvansky V. A., Maraev V. V. Laser Doppler flowmetry as a method for assessing wound microcirculation. II International Congress dedicated to the 70th anniversary of the Institute of Surgery named after. A. V. Vishnevsky. "Wounds and wound infection", p. 130–131.
- Larichev A. B., Antonyuk A. V., Kuzmin V. S. Vacuum therapy in the treatment of chronic wounds. Yaroslavl. 2007.
autodermatoplasty vacuum therapy diabetes surgery
Granulation of wounds: complications
If the granulation process is complicated by other processes, wound healing may take a long time, which will require additional measures. The most dangerous complications include:
- Sepsis is a blood infection that develops as a result of a large amount of pathogenic microflora entering the body, which becomes active when the body’s defenses are low.
- The wound festers, it is necessary to perform a necroectomy, in which the affected areas of the wound are excised.
Wound granulation is complicated by poor hygiene and improper wound care. You can use special ointments and creams that accelerate the regeneration process and allow the wound to heal as quickly as possible along with scar tissue.