The discomfort that occurs next to an interlocutor who has a problem with bad breath is familiar to everyone. The prevalence of this disease is extremely high: more than half of the world's population. Some clinical studies report a prevalence of 60% and even 80%. It would be a good reason to ignore the problem, because these are the majority! However, independent surveys have shown that almost 50% of respondents claim that bad breath significantly harms the successful career of its owner (especially if the professional activity is related to communication). 20% of respondents consider halitosis one of the most repulsive physiological “manifestations” of a human person (surveys were conducted in the UK). A person who has the problem of halitosis often does not even realize it, because he is adapted to his own smell. Humans, like other living beings, are evolutionarily programmed to pay attention primarily to unfamiliar, pungent and unpleasant odors. The sense of smell allows living beings to find food, find a sexual partner, receive sensory pleasure (for example, the smell of flowers or perfume), and also receive alarm signals (for example, spoiled food, dangerous chemicals). Knowing about the problem of bad breath, patients, as a rule, try to solve the problem on their own, turning to perfume, refreshing rinses, sprays, chewing gum, etc. However, these techniques only mask the unpleasant odor for a short period. A real solution to the problem can be achieved with the help of a specialist who will competently identify the causes of halitosis and select adequate treatment.
Causes
Halitosis can be general or local. In the first case, it is associated with dysfunction of internal organs, in the second - with the condition of the oral cavity. The main causes of local halitosis include:
- violation of oral hygiene rules, accumulation of bacterial plaque and the formation of hard dental deposits;
- single and multiple caries - superficial, medium, deep;
- stomatitis, periodontitis and periodontal disease;
- pulpitis, glossitis, cheilitis, gingivitis;
- alveolitis, peri-implantitis, pericoronitis, etc.
These are the so-called intraoral causes. For example, braces or orthopedic structures must be carefully maintained to prevent the accumulation of pathogenic microflora.
General halitosis can be associated with extraoral causes: diseases of the respiratory tract, digestive tract, intestinal dysbiosis, diseases of the liver, gall bladder, and kidneys. In addition, it occurs in endocrine pathologies - diabetes mellitus, thyrotoxicosis. Many ailments cause changes in the composition and viscosity of saliva and the volume of its production. Insufficient hydration of the mucous membranes contributes to a decrease in protective functions. If there are no obvious symptoms of dental disease, it is important to consult a therapist or specialist to find out the cause of bad breath. A separate category of causes is taking medications that cause changes in the composition of saliva or are accompanied by side effects such as dry mouth. Common medications with this effect are antibiotics, antiviral drugs, chemical dependency treatments, and drugs to normalize heart rate and blood pressure. In this regard, dry mouth and halitosis associated with changes in the composition of saliva are often found in older age groups - older people who constantly take many medications.
Ask a Question
Causes and Treatments for Bad Breath
Pathological halitosis is of two types. Oral develops due to diseases of the oral cavity, extraoral - when internal organs are damaged.
The problem of bad breath is almost always dealt with by a dentist. He diagnoses and determines the type of halitosis. If the oral cavity is healthy, refer the patient to a therapist. It identifies extraoral or non-dental causes of halitosis - diseases of the digestive tract, upper respiratory tract, diabetes mellitus, liver cirrhosis or uremia.
All oral causes are associated with the proliferation of anaerobic flora - bacteria, due to which tissues begin to rot. During the inflammatory process, microbes use proteins of the body's cells for their growth, and not those that come from food. Protein foods can only make your bad breath worse.
The causes of halitosis in adults include the following dental pathologies:
- Tartar and plaque . They are a collection of bacteria that form on the enamel and under the gum. They are removed during professional cleaning by the dentist.
- Caries . Tooth enamel is gradually destroyed, the tooth rots, and putrefactive masses accumulate in the carious cavity and because of them, many by-products with an unpleasant odor are formed. After cleaning the carious cavity or removing a rotten tooth, halitosis disappears.
- Gingivitis . Bad breath can be a sign of gum inflammation, which causes your gums to bleed, become red, and painful. To get rid of all symptoms, antibiotic ointments and physical therapy are used, and in advanced cases they are treated surgically.
- Stomatitis and glossitis . Inflammation of the mucous membrane and tongue develops due to the proliferation of harmful microorganisms - staphylococci, streptococci or fungal flora. Damage is indicated by pain during eating, small ulcers and films on soft tissues. Treatment of pathology is complex using antimicrobial, wound healing and analgesic ointments.
- Infection under an artificial crown . When a crown is placed on a diseased tooth or the root canals are poorly cleaned, inflammation continues underneath it. To eliminate it, the dentist removes the crown, removes the filling and post, cleans the root canal, and after a few days places a new crown.
- Peri-implantitis . If a false tooth does not take root, an inflammatory reaction develops around its shaft. Rejection occurs both in the first month after installation and several years after implantation. In case of purulent infection, the implant is removed, and after treatment, a new one is tried.
- Pericoronitis . If, when a wisdom tooth erupts, a “hood” of inflamed gums forms above it, food particles get underneath it and rot. When the figure eight grows correctly, the dentist cuts the gum and releases the crown of the growing tooth. When the molar is positioned horizontally or obliquely, it is removed along with the inflamed tissue.
- Alveolitis . If, after removing a tooth with its roots, bacteria remain in the hole, purulent inflammation begins in it. To eliminate it, the doctor cuts the gum again, removes the inflamed tissue, cleans the hole with an antiseptic and places a drainage tube for several days.
Bad breath often bothers people who wear removable dentures or braces. If the denture is not firmly fixed on the jaw, pieces of food accumulate between it and the gum. Food can also get stuck between the ligatures that connect the braces.
Symptoms and manifestations
If halitosis occurs exclusively in the morning and goes away after brushing your teeth, we are talking about the physiological nature of the symptom. At night, saliva production decreases and anaerobic microflora actively multiplies. After waking up and performing hygiene procedures, the unpleasant odor disappears, and this condition is the norm.
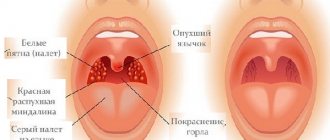
Pathological bad breath is also observed after brushing your teeth. It can be different, the nature of halitosis is determined by the reasons. Thus, a purulent smell can be observed with periodontal disease and pharyngitis, the smell of acetone - with diabetes mellitus, dehydration, the smell of ammonia - with liver dysfunction and diffuse toxic goiter, a sour smell - with fungal infections of the mucous membranes of the oropharynx. In addition, the cause of this symptom can be assumed based on the symptoms that accompany halitosis:
- bleeding gums - with periodontitis, periodontal disease, aphthous stomatitis, etc.;
- tooth mobility, the appearance of periodontal pockets - with periodontal disease;
- white or yellowish coating on the oral mucosa - with candidiasis, stomatitis;
- darkening of areas of enamel in the area of the gum line - with hard dental plaque;
- an increase in the volume of gingival papillae between the teeth, looseness of the gums - with gingivitis;
- pain and swelling of the mucous membrane of the tongue - glossitis, etc.
If there are no other symptoms other than halitosis itself, or nonspecific manifestations are present, there is a possibility of systemic pathologies, gastrointestinal diseases or endocrine disorders. Therefore, it is important to visit not only the dentist, but also the general practitioner.
When does bad breath require treatment?
Halitosis is the term for bad breath.
It affects 30 to 65% of people living in developed countries and is both a medical and psychological problem. Halitosis occurs:
- True, if the unpleasant smell is constantly felt by others;
- Imaginary, when halitosis occurs periodically, but only the patient himself feels it;
- False if there is no objective symptom, but the person is sure that he has bad breath.
On the website Stom-Firms.ru, read why bad breath occurs, how it is treated and prevented.
Principles of treatment of halitosis
Diagnosis of halitosis necessarily includes an examination by a dentist. This is necessary to confirm or exclude dental pathologies. The dentist will conduct a survey and examination of the oral cavity, and recommend sanitation, if necessary. The main principles of treatment are:
- professional cleaning: removal of hard dental deposits and soft plaque;
- elimination of oral diseases: treatment of caries, inflammatory diseases of the mucous membranes and gums, removal of teeth that cannot be restored, etc.;
- dieting: avoidance of specific foods, nutritional correction;
- compliance with personal hygiene recommendations: selection of a toothbrush of the required hardness, suitable toothpaste, rinses, as well as training in the use of dental floss.
Your mouth is under attack from germs!
Where does the unpleasant smell come from? Various microorganisms live in the nasopharynx and oral cavity; the list of them is quite impressive - more than 120 species. These microbes “nest” in pathological gum pockets, carious cavities, interdental spaces, nasopharyngeal mucus, secluded places in the tonsils and other “quiet pools.” This fact alone indicates that only careful and competent hygiene of the oral cavity (and the entire digestive tract along with the respiratory system) can control the situation with microbial “revelry”.
Medicines and folk remedies against halitosis
Drug treatment of local halitosis is based on the causes. If the source of the unpleasant odor were foci of infection or carious cavities, then halitosis goes away on its own after sanitation of the oral cavity. You can also cope with the problem with the help of antiseptics; they help suppress pathogenic microflora and participate in the prevention of relapses of inflammatory diseases. It is better to choose antiseptic rinsing solutions on the recommendation of a specialist.
If the cause of the unpleasant odor was infectious diseases of the gums and mucous membranes, the doctor will prescribe local medications: ointments, gels for application or application. The dentist will find out the nature of the infection and prescribe a drug with antibacterial, antiviral or antifungal action. Combined products also contain other components to relieve itching, burning, pain and eliminate halitosis. With severe inflammation, systemic antibacterial therapy may be required: antibiotics, fungicidal medications, powerful antiviral and immunomodulatory agents.
In cases where halitosis is promoted by orthodontic and orthopedic structures, the dentist will refer you to a specialist. You can discuss the prospects for choosing an alternative method of correcting your bite with your orthodontist. A visit to an orthopedic dentist is necessary for the correction of dentures or structures, as well as their replacement.
For periodontal disease, the course of treatment can be complex and quite complex, including removal of subgingival dental plaque, splinting and other measures. A periodontist can help treat the underlying cause of bad breath and prevent complications.
Many patients are interested in how to cure halitosis at home. It is important to remember that the use of traditional medicine methods must be agreed with a specialist; dentists do not recommend self-medication. One of the relatively safe methods includes rinsing with herbal infusions. Decoctions of chamomile, oak bark, and sage have an antiseptic effect. Remember: the solution must be warm; under no circumstances should you rinse your mouth with a hot solution, as this can cause a burn.
As folk remedies, you can resort to consuming certain foods that promote fresh breath. These include the following:
- apples, carrots, pears;
- watermelon, rosemary;
- fresh herbs - parsley, mint, basil.
Finely grated ginger root can also cope with unpleasant odors. Consider allergic reactions when choosing foods - choose your own diet based on preferences and individual characteristics.
Halitosis – a medical and social problem
Halitosis is a persistent bad breath that cannot be eliminated by traditional means of prevention and hygiene. Currently, this problem in dentistry is posed somewhat differently, and new approaches and possibilities for solving it have emerged.
The problem of halitosis or persistent bad breath, despite its current relevance, is by no means new. Back in the 2nd century BC. Apuleius wrote: “There is nothing more contrary to the appearance of a free and noble man than an unkempt mouth.” And today, bad breath is considered, on the one hand, as a manifestation of the pathology of internal organs, and on the other, as a low level of oral hygiene.
Halitosis (halitosis) - (synonyms of halitosis - ozostomia, stomatodisody, fetor oris or fetor ex ore), according to the apt expression of J. Tonzetich (1977) - one of the experienced researchers in this field, can be classified as a “social disability”, since for For a certain group of the population, it often causes restrictions on the communication of people suffering from this disease.
The problem of halitosis has medical and psychological (social) aspects: firstly, the presence of halitosis can be an indicator of the pathology of various organs and systems of the human body; secondly, halitosis and the fear of halitosis have a huge negative impact on a person’s social and personal life. The well-being of a person in modern society is largely determined by his image and interpersonal connections, and therefore halitosis is considered as a social impairment, which is the cause of social isolation (self-isolation), an obstacle to building a career, family, etc.
The incidence of halitosis in developed countries ranges from 30 to 65%. In recent years, halitosis research has been supervised by the international organization International Society for Breath Odor Research (ISBOR), which unites experts in various fields of knowledge - from molecular biology to sociology.
The dentist is one of the main specialists in charge of the problem of halitosis both in scientific research and in practical healthcare. As a rule, patients with symptoms of halitosis first of all go to see a dentist, who can and should correctly assess the situation (distinguish between imaginary and true, physiological and pathological halitosis), establish the cause of halitosis, eliminate oral sources of halitosis and help the patient minimize the problems of halitosis, not related to dentistry. In addition, the problem of halitosis may serve as an appropriate reason to attract public attention to oral hygiene and the preservation of oral health.
Scheme of the occurrence of halitosis: peptides of food debris + salivary proteins → breakdown to amino acids - aminolysis (putrefactive breakdown of amino acids with the participation of anaerobic microorganisms of the oral cavity) → volatile sulfur-containing compounds and volatile amines. It should be understood that bad breath is not a disease itself, it is only a sign and consequence of certain changes in the human body,
Bad breath is caused by the presence of volatile compounds in the exhaled air that have an unpleasant odor. Odorants that cause halitosis include:
- volatile sulfur compounds: hydrogen sulfide, dimethyl sulfide. methyl mercaptan, dimethyl disulfide, allyl mercaptan, propyl mercaptan, carbon disulfide;
- amines: putrescine, cadaverine, dimethylamine, trimethylamine; ammonia;
- organic acids: butyric, isovaleric.
Gases that have an unpleasant odor are characterized by three main indicators:
a) threshold of perception (gas concentration at which the odor is noticeable, but too weak for identification);
b) threshold of 100% odor recognition (the odor is identified by all researchers);
c) the threshold of rejection (irritation).
From the list presented in Table 1, the most odorous are unsaturated mercaptans (allyl mercaptan in garlic), then, in descending order, saturated mercaptans (propyl mercaptan in onions), methyl mercaptan, sulfides, methylpropyl sulfide in onions and dimethyl sulfide.
Table 1
Characteristics of substances that determine breath odor in halitosis
| Compound | Chemical formula | Associative characteristics of smell | Odor index | 100% recognition threshold |
| Hydrogen sulfide | H2S | rotten egg | 17.000.000 | 1.000 ppb |
| Methyl mercaptan | СН3СН | pungent smell of feces, rotten cabbage | 53.000.000 | 35 ppb |
| Dimethyl sulfide | CH3SCH3 | unpleasantly sweet smell of cabbage, sulfur, gasoline | 2.760.000 | 100 ppb |
| Dimethyl disulfide | CH3SSCH3 | spicy | 7 ppb | |
| Skatol | 3-methyl-N-indole | feces, mothballs | ||
| Cadaverine | С5Н14N2 | corpse, urine | ||
| Putrescine | NН2(СНН7)4NН2 | rotting meat | ||
| Isovaleric acid | sweat, rancid milk, spoiled sire | |||
| Allyl mercaptan | CH2=CHCH2SH | garlic | ||
| Propyl mercaptan | CH3CH2CH2SCH3 | spicy unpleasant | 263.000.000 | 0.7 ppb |
| Trimethylamine | (CH3)3N | fish, ammonia | 280.00 | 6.000 ppb |
| Dimethylamine | (CH3)2NH | fish ammonia | 493.500 | 4.000 ppb |
| Ammonia | NH3 | nice fresh | 1.673.000 | 55.000 ppb |
| Carbon disulfide | CS2 | mild hot | 1.600.000 | 900 ppb |
The sources of these connections may be:
1. Food products (garlic, onions, radishes, cabbage, etc.).
2. Metabolic products of anaerobic bacteria, mainly gram-negative rods, such as fusobacteria and actinomycetes.
3. Products of carbohydrate fermentation.
4. Decaying food scraps.
However, the main etiological factor in the occurrence of bad breath is the production of hydrogen sulfide by anaerobic bacteria, which, as a rule, develop in places that are practically inaccessible to oxygen.
Conventionally, all the reasons contributing to the appearance of halitosis can be divided into 2 groups:
1) local - related to the condition of the oral cavity;
2) general, that is, related to the general condition of the body.
In almost 80-90% of cases, the occurrence of bad breath (halitosis) is associated with local causes in the oral cavity, of which the main ones are:
1. Dental diseases, such as: dental caries and its complications; inflammatory periodontal diseases; diseases of the oral mucosa; tumor-like formations; and etc.
2. Unsatisfactory hygienic condition of the oral cavity, caused by poor care of teeth, tongue, as well as orthopedic and orthodontic structures, has a reliable feedback with the level of volatile sulfur compounds, since neglect of hygiene leads to long-term retention of food particles, which are a substrate for the vital activity of microorganisms , in the interproximal zones, in the gingival region, on the back of the tongue, on the elements of the prosthesis (device). The proliferation of anaerobic microorganisms, as a result of whose vital activity, volatile sulfur compounds are released, giving the breath an unpleasant odor.
3. Xerostomia or dry mouth syndrome is the most common cause of halitosis. As a result of a decrease in the rate of saliva secretion, the processes of natural cleansing of the oral cavity are disrupted, and favorable conditions are created for the proliferation of various microorganisms. Dryness of the mucous membrane provokes compensatory secretion of plasma proteins onto the surface of the mucosa, which are an additional substrate for the production of volatile sulfur compounds. In addition, the cause of the development of xerostomia may be the use of medications, diseases and dysfunctions of the salivary glands, and oral breathing.
The development of halitosis may be due to general factors, that is, related to a person’s standard of living and the presence of systemic diseases of the body.
The nature of nutrition can create conditions in the oral cavity that are favorable or unfavorable for halitosis. A diet rich in protein, sourced from dairy and meat products, provides the oral environment with a substrate for the production of volatile sulfur compounds. Since the end products of protein metabolism are ammonium compounds with alkaline properties (urea, ammonia), the pH of the environment increases, which promotes the growth of anaerobic bacteria and the production of volatile sulfur compounds. A diet rich in carbohydrates, on the contrary, leads to a decrease in the pH of the oral environment and, accordingly, inhibition of the production of these compounds. Coffee, regardless of its caffeine content, reduces the level of oxygenation and changes the level of acidity in the oral cavity, which contributes to the rapid proliferation of microorganisms and, with frequent consumption, the formation of so-called “coffee” breath. Carbonated drinks sweetened with sweeteners may cause oral halitosis. Alcohol consumed in beer, wine or stronger drinks extremely increases the dryness of the oral mucosa, reducing its protective capabilities and promoting the active proliferation of anaerobic microorganisms. Over time, chronic alcohol consumption leads to degeneration, precancerous changes and destruction of the oral mucosa. Dryness of the mucous membrane provokes compensatory secretion of plasma proteins onto the surface of the mucosa, which are an additional substrate for the production of volatile sulfur compounds.
Fasting . When there is a deficiency of nutrients in the body, endogenous reserves are utilized, which can cause an unpleasant odor due to the release of metabolic products, and oral hygiene does not help eliminate the odor. Usually, “hungry breath” lasts until you eat. Rare and poor nutrition, caused in some cases by the unavailability of food, in others by diets for weight loss, leads to hyposalivation and, thus, to oral halitosis.
Tobacco smoking leads to worsening bad breath for several reasons: nicotine, tobacco combustion products themselves have an unpleasant odor; as a result of smoking, the mucous membrane dries out and the natural protective systems of the oral cavity are disrupted; when smoking, the amount of oxygen in the oral cavity decreases, which promotes the activity of anaerobes and protein catabolism; Smoking contributes to the development of inflammatory periodontal diseases and the deposition of tartar.
Hormonal fluctuations during the menstrual cycle in women can cause bad breath (“menstrual breath”) because changes in the concentration and ratio of sex hormones affect the properties of saliva. On days when saliva becomes less abundant and more viscous, its oxygen content decreases, which leads to the initiation of the production of volatile compounds.
Stress or nervous tension . Often, bad breath appears during a stressful situation and disappears immediately after the cessation of emotional stress. Stress causes a significant decrease in salivation and is therefore an important factor in the occurrence of transient oral halitosis.
The use of medications can provoke oral halitosis through changes in the balance of oral microflora, most often such problems are associated with antibiotic therapy and hormonal treatment (corticosteroids). In addition, about 70% of the most commonly prescribed drugs transport sulfur and its compounds across the blood-salivar barrier.
Halitosis associated with the nose, paranasal sinuses, and larynx. According to various sources, ENT organs and the upper respiratory tract cause from 8 to 25% of cases of true halitosis. The main substrate for the formation of volatile sulfur compounds in this zone is secretions produced by the nasal mucosa. With damage to the mucous membrane of the nose and paranasal sinuses, including chronic rhinitis, sinusitis, polyposis, influenza, etc., an increase in the number of anaerobic microorganisms producing light compounds is observed.
Halitosis associated with pathology of the bronchopulmonary system. True halitosis can be a consequence of pathological processes of the lower respiratory tract - bronchitis, bronchiectasis, pneumonia, pulmonary abscess, lung carcinoma. The breath and sputum of patients with anaerobic pulmonary infection have a putrid, fecal odor
Halitosis associated with the direct entry of gases from the gastrointestinal tract into the oral or nasal cavity. Bad odor from the stomach, contrary to popular belief, is a relatively rare cause of halitosis: the esophagus is usually in a collapsed state, so gases from the upper gastrointestinal tract in a calm state cannot rise into the oral cavity and enter the exhaled air. Thus, odors from the stomach can change breathing only during vomiting, belching, coughing, or in severe pathology - gastroesophageal reflux, pyloric stenosis, hiatal hernia.
Somatic diseases as causes of hematogenous halitosis. The cause of the development of low-intensity hematogenous halitosis can be chronic nonspecific diseases of the respiratory system, as well as pulmonary abscess, foreign bodies, necrotizing pneumonia, tuberculosis or lung cancer. Hematogenous halitosis may be associated with dysfunction of the liver (dimethyl sulfide is determined in the exhaled air) and biliary tract (hydrogen sulfide is released). Hematogenous halitosis has been noted in pathologies of the gastrointestinal tract: with non-ulcerative dyspepsia caused by Helicobacter pylori (the content of hydrogen sulfide and dimethyl sulfide in the exhaled air is increased), with reduced absorption syndrome, gastric ulcers, and gastric carcinoma. “Uraemic breathing” is known, characteristic of patients with renal failure: in the air exhaled by patients, a “fishy” smell of dimethylamine trimethylamine or the smell of ammonia is detected. Breath in diabetic ketoacidosis has such a distinct smell of acetone that it can be used to diagnose this pathology. Persistent hypermethionemia as a pathology causing the presence of dimethyl sulfide in the exhaled air
Metabolic disorders as causes of hematogenous halitosis. When the ability to ferment plant (soy) proteins is impaired (trimethylaminuria or “fishy odor syndrome”), putrid breath includes components of sulfur compounds and amines (trimethylenamine). Lactase enzyme deficiency, characteristic of most adults, causes halitosis when consuming dairy products, regardless of their degree of fat content: skim milk, yogurt, cream, ice cream, cheese, etc., since, in such cases, milk proteins are rich sulfur-containing amino acids are broken down by intestinal microorganisms to form light sulfur compounds. Similar problems arise in people who do not have enzymes to break down gluten and, in this case, the cause of hematogenous halitosis is the consumption of grain foods. In older people, digestion problems and associated halitosis are more common than in younger people, as the body's production of digestive enzymes declines over the years. Enzyme deficiency leads to intensified microbial decomposition of food and excessive formation of odorogenic gases, which determine the odor of exhaled air.
Pseudohalitosis occurs in situations where a patient, having bad breath odor at a level close to the threshold of perception, overestimates the severity of the problem, finding false evidence of "horrible" breathing in the behavior of interlocutors, which he misinterprets as avoidance. As a rule, problems with psevohalitosis occur in people with low self-esteem, who have had episodes of true halitosis, have undergone successful treatment, but maintain a high level of anxiety about halitosis. The level of anxiety with pseudohalitosis is supported by the fact that reliable self-diagnosis of halitosis, as well as discussing this topic with other people, is extremely difficult, so a patient who does not have objective evidence of the acceptability of the smell of his breath tends to assume the worst. This indicator can be calculated using the WTC (Winkel Tongue Coating) index
The problem of halitosis is aggravated by the fact that people have limited opportunities for self-diagnosis of this problem, since they poorly distinguish the smell of their own breath due to the adaptation of the olfactory receptors to it. As a result, most people are conscientiously mistaken about the quality of their breath: a significant proportion of people with halitosis are unaware of this, while many people with fresh breath are absolutely sure of the opposite. Without special efforts, a person can only learn about the presence or absence of halitosis from words from those with whom he interacts, or from a doctor. Most methods of self-diagnosis of halitosis allow the patient to judge only the absence/presence of a problem based on an assessment of the smell of air and oral fluid on the “pleasant - neutral - unpleasant” scale, since they indicate the quality of the smell, but not its strength.
Control from family and friends. Although there are many reasons why a patient may not ask a spouse or friends about the freshness of their breath, such cooperation is the best method for home testing. The authorized representative must be aware of what time of day and under what conditions the unpleasant odor is most pronounced. It is advisable that the partner knows what events provoke the deterioration of the patient’s condition and is involved in dynamic monitoring of the quality of his breathing during the treatment of halitosis.
Spoon or napkin test. This easy test is the second most effective method for self-diagnosing halitosis. The patient himself cleans the plaque from the back third of the back of the tongue with a small plastic spoon, after a minute the patient himself or his authorized representative evaluates the smell of the removed plaque. The spoon can be replaced with a simple sanitary napkin. To perform this test, stick out your tongue as much as possible and hold it by the tip with a napkin. The very back of the back of the tongue is wiped twice with a clean white napkin and after 40-45 seconds its smell is assessed. A positive test allows you to diagnose not only the presence of halitosis, but also to recognize the source of light sulfur compounds - plaque on the tongue.
Dental floss test. The interdental spaces in the area of the upper and lower molars are cleaned with white, unwaxed, unscented dental floss, then the coloring of the used area of the floss is assessed (yellow or red color indicates the presence of plaque and bleeding - risk factors for halitosis) and after 30-40 seconds the smell of the floss is assessed.
Hand test. A method that allows a person to preview the smell of their oral fluid and, to some extent, the coating on their tongue is to simply lick their metacarpus, wait 10 seconds and then smell their skin.
Halitox test . The test allows you to carry out at home a qualitative and semi-quantitative determination of the content of substances responsible for halitosis in the plaque on the tongue - light sulfur compounds (hydrogen sulfide, dimethyl sulfide, dimethyl disulfide, methyl mercaptan) and polyamines (putrescine, cadaverine). The test requires simple, commercially available equipment: a test tube with a special medium. The test can be done four hours after your last meal or drink.
To diagnose the presence and severity of halitosis in clinical and laboratory conditions, methods are used that allow assessing the intensity of halitosis based on organoleptic or instrumental determination of the content:
- volatile substances associated with halitosis in exhaled air;
- participating in the catabolism of volatile sulfur compounds found in oral fluid.
Air testing is carried out after eliminating random or controllable causes of halitosis (food, drugs, tobacco, etc.), but preserving native oral biotopes potentially associated with halitosis (plaque on the tongue, teeth, etc.), since in the oral air, random fluctuations in the concentration of light compounds in one person during one day are not uncommon; studies are repeated several times.
Organoleptic measurement of exhaled breath odor. The method involves assessing the smell of the patient's exhaled air by a trained specialist (dentist). Before carrying out a sensory evaluation, both the patient and the researcher must comply with a number of conditions in order to obtain the correct result. On the eve of testing, the patient is advised to refrain from taking antibiotics, consuming onions, garlic, seasonings and spicy foods (for 48 hours), using scented cosmetics (within 24 hours), smoking tobacco (within 12 hours), and not cleaning teeth, do not use oral rinses, chewing gum, or breath fresheners for 12 hours prior to the test. The researcher must have a normal level of smell, which is checked by preliminary testing of his ability to recognize “standard” odors in various concentrations. On the eve of testing, the researcher should refrain from drinking coffee, tea or juice, wearing perfume or smoking.
Nasal breathing. The method involves assessing the smell of the patient's exhaled air through the nose. The air exhaled from each nostril in turn is examined in order to determine the “incubation” of anaerobic microflora of the oral cavity that produces volatile sulfur compounds.
BA N A-test (an abbreviation for the first letters of the name of the synthetic protein - Benzoyl-DL-Arginine-NaphthylAmide), which is broken down under the influence of enzymes produced by microorganisms responsible for the development of periodontitis (Treponema denticola, Porhyromonas gingivalia and Bacteroides forsythus) and halitosis. To perform the test, special plastic strips are used, on which plaque taken from the interdental space is placed. The presence of these microorganisms in the plaque causes the strip to turn dark blue, and the darker it is, the greater the number of microbes contained in the plaque.
Sulfide monitoring is carried out using the “Sulfide Monitor (Halimeter)” device, developed by the American company. This device was first used in the USA, where halitosis treatment centers were subsequently organized under various names: halitosis center, halitosis clinic, fresh breath center, etc. This is how a new direction in dental practice emerged, which was greatly facilitated by the creation of “Halimeter”. The device is an electrochemical gas sensor meter that records the concentration of hydrogen sulfide (mainly) and other volatile substances in the air, supplemented by a recording device that records the results of the study in the form of a graph - a haligram. The concentration of hydrogen sulfide in air taken from the oral cavity of a person without true halitosis ranges from 80-110 μg/kg of air. The advantages of halimetry are objectivity, simplicity and accessibility. The haligram allows you to assess the dynamics of the level of halitosis against the background of treatment and preventive measures. The disadvantages of halimetry are associated with the selective sensitivity of the device to volatile sulfur compounds (hydrogen sulfide is twice as high as methyl mercaptan) and the complete lack of information about the presence in the air of other compounds responsible for halitosis (butyric and propionic acids, putrescine and cadaverine). In addition, the halimeter readings are very dependent on other volatile compounds emanating from the patient (the smell of chewing gum, mouthwash, alcohol, shampoo, lotions, tobacco, and even the concentration of water vapor in the air being tested). Therefore, many researchers tend to regard the results of halimetry as additional to the data of an organoleptic study.
The portable fresh breath indicator (halitometer) air-lift line detects and measures the concentration of malodorous volatile sulfur- and nitrogen-containing compounds in exhaled air on a five-point scale. When used in dental clinics, it allows not only to diagnose the degree of halitosis (as part of an initial examination or a separate service), but also is the first step to planning subsequent manipulations for treatment. The device was created by Japanese electronics specialists specifically and exclusively for the Spanish air-lift “Fresh Breath from Within.”
Gas chromatography and mass spectrometry make it possible to make a complete quantitative analysis of the content of hydrogen sulfide, methyl mercaptan, dimethyl sulfide, and amines in the air, starting from minimal (subthreshold) concentrations.
An artificial nose is a device consisting of several electrochemical sensors and equipped with computer support (“artificial intelligence”), which has high sensitivity to light sulfur compounds in the air, which allows its clinical use for the diagnosis of halitosis.
The study of oral fluid for the content of light sulfur compounds involves an organoleptic or halimetric study of unstimulated saliva - fresh or incubated under anaerobic conditions at a temperature of 37 ° C for 3 or 6 hours. The indirect method, which includes cysteine and methionine in the protocol, allows you to assess the level of volatile sulfur compounds after 20 minutes using a gas analyzer.
Prevention and treatment of halitosis
Bad breath will not go away if you simply mask it with other odors. First of all, it is necessary to find and eliminate the cause of the disease.
To prevent and treat halitosis, the following measures must be taken:
1. If you notice persistent bad breath, you should contact a dentist.
2. Sanitize the oral cavity.
3. Eliminate foci of odontogenic infection, remove decayed teeth that cannot be restored, as well as wisdom teeth with difficulty erupting (partial) retention.
4. Take a course of professional oral hygiene with the removal of supragingival and subgingival dental plaque.
5. With the help of a dentist, undergo training in methods of individual oral hygiene, including brushing your teeth and tongue;
- Brushing your teeth should be done with a toothbrush and floss;
- prescribe special rinses: decoctions of celery, mint, fennel:
- prescribe medications containing menthol and essential oils, for example, non-sugar-containing chewing gum.
If the symptoms of halitosis persist after eliminating possible local causes in the oral cavity, you should consult a general practitioner.
The clinical classification of halitosis is accompanied by a list of the patient’s treatment needs (TN) at each level of pathology (Table 2):
table 2
Treatment protocols for halitosis
| Classification level of halitosis | Need for treatment | Contents of the diagram |
| I. True halitosis: physiological | TN - 1 | Halitosis education, oral hygiene instructions |
| I. True halitosis: pathological 1) oral | TN - 2 | Professional oral hygiene. treatment of oral pathology |
| I. True halitosis: pathological 2) extraoral | TN - 3 | Consultations with a therapist and specialists |
| II. Pseudogalithosis | TN - 4 | Explanation of odor test results, education, follow-up examinations and consultations |
| III. Halitophobia | TN - 1 - 5 | Consultations with a psychologist, psychiatrist |
Educating the patient regarding the causes and conditions for the formation of halitosis, the choice of drugs, items, products for caring for the oral cavity (especially the surface of the tongue), motivation for self-help and training in its basic methods - this is the content of the TN-1 protocol,
Unfortunately, there are few products on the Russian pharmaceutical market that not only “interrupt” the unpleasant odor, but are capable of neutralizing volatile sulfur- and nitrogen-containing compounds that cause bad breath. One of them is the Spanish air-lift line, which includes products to combat both oral halitosis (toothpaste, rinse, spray, drops, chewing gum) and the foul odor formed in the gastrointestinal tract (oral capsules) .
The Biocosmetics SL laboratory (Spain) has developed this line of products, which include a combination of olive, chlorophyll oils, essential oils of parsley seeds and peppermint. Using a combination of these oils helps neutralize unpleasant odors and guarantee fresh breath. The above-described vegetable oils envelop the “smelly” molecules, enclosing them in an impenetrable “sarcophagus”. In addition, olive and chlorophyll oils have a beneficial effect on the mucous membrane of the gastrointestinal tract and oral cavity.
In what cases and in what combination should air-lift products be used (Table 3):
Table 3
Treatment of physiological halitosis with products included in the ir -lift
| Chronic unpleasant odor | Oral origin | Morning and evening air-lift toothpaste, rinse throughout the day with air-lift chewing gum (1-2 products to choose from |
| Extraoral origin | In the morning and evening, toothpaste, air-lift during the day, rinse with air-lift chewing gum (1-2 products to choose from) | |
| Occasional unpleasant odor | Smell of fumes | In the morning, 2-3 capsules of air-lift, washed down with water, air-lift toothpaste, air-lift rinse, air-lift spray, air-lift drops, air-lift chewing gum |
| Smoking | After each cigarette smoked, air-lift spray. air-lift drops | |
| Eating onions, garlic, cabbage, etc. | After meals, 1-2 air-lift capsules with water, or air-lift spray of your choice | |
| Morning bad breath | In the evening, 1-2 capsules of air-lift, washed down with water, + air-lift toothpaste | |
Dental care in the prevention and treatment of pathological oral halitosis (T N -2)
Dental efforts to prevent pathological oral halitosis come down to primary, secondary and tertiary prevention of the main conditions for its occurrence, namely the pathology of salivation, periodontal tissue and teeth.
Activities that complement the TN-1 protocol to help patients suffering from oral pathological halitosis are professional hygiene (reduces the content of methyl mercaptan in the air of the oral cavity by 10-60%), periodontal surgery and removal of decayed teeth (leads to an 85% reduction in the content of methyl mercaptan ), measures to correct xerostomia.
In home oral hygiene, such patients are recommended to use pulsating oral irrigators with special cannula attachments, which allow for more effective removal of infected masses and food debris from the periodontal pockets, as well as improve oxygenation of the oral cavity. Irrigation of the oral cavity (mucosa, periodontium, teeth and surface of the tongue) is carried out using a constant or pulsating stream of warm water under pressure ("jet" and "shower" modes). Irrigation efficiency increases when chlorine dioxide and zinc acetate are used as the working fluid.
Oxygenation of the oral cavity. Today, the most popular methods are those that provide intense oxygenation of the oral cavity, since oxygen inhibits anaerobic microflora. The source of active oxygen, as a rule, is peroxide compounds. In cases where intense bad breath is associated with the gum area, oxygen gel can be applied in specially made trays extending to the surface of the gums.
A study was conducted of the influence of various tongue hygiene products on the functional state of the taste analyzer in patients suffering from halitosis due to periodontitis. It was found that sanitation of the oral cavity, professional hygiene and tongue cleaning (using a tongue brush with gel) significantly improved taste sensitivity, which is associated with the release of the taste buds of the tongue from plaque. Patients suffering from extra-oral halitosis should be referred to appropriate specialists after receiving dental care under the TN-1 protocol.
Help in the prevention and treatment of pseudohalitosis (T N -4).
Since pseudohalitosis is more of a psychological problem, a dentist who has successfully implemented the TN-1 protocol for a patient should make efforts to increase the patient's self-esteem: in particular, reassure the patient that his breathing can no longer cause negative reactions in others, despite to something that contains a certain subliminal or threshold amount of odorigens (TN-4).
V.Yu. Khitrov, A.I. Zabolotny
Kazan State Medical Academy
Zabolotny Alexander Ivanovich - Candidate of Medical Sciences, Associate Professor of the Department of Therapeutic and Pediatric Dentistry
Literature:
1. Fursa V.T. About bad breath. J. "Paramedic and midwife", 1988. No. 6, pp. 61-62
2. Volozhin A.I., Petrovich Yu.A., Filatova E.S., Barer G.M., Fomina O.L., Kreit Kh.N., Volozhina S.A., Dieva S.V. Volatile compounds in the air and saliva of the oral cavity of healthy people, with periodontitis and gingivitis. J. "Dentistry", 2001, No. 1, pp. 9-12.
3. Halitosis is a new problem in dentistry. J. “Dentistry for everyone”, 2004, No. 1, pp. 18-20.
4. Poleva N., Eliseeva N. Halitosis: diagnosis, treatment, prevention. J. "Dentist", 2005, No. 3, pp. 33-37.
5. Mitronin A.V., Dmitrieva N.G. The influence of hygiene products on the taste sensitivity of the tongue of patients with periodontitis and halitosis. J. “Dentistry for everyone”, 2006, No. 4, pp. 20-22.
6. Kodola N.A., Kozlovsky S.I. Bad breath - its causes, prevention and treatment. J. “Dentistry for everyone”, 2006, pp. 126-129.
7. Study of the manifestations of halitosis. J. "Dental Journal", 2006, volume 4, pp. 310-313.
8. Means for the treatment and prevention of halitosis. J. “Dentistry Today”, 2007, No. 9 (69) pp. 65-66.
9. Mitronin A.V., Tsareva V.N., Dmitrieva N.G. Halitosis problem. J. "Dentist", 2007, No. 1, pp. 48-52.
10. Pakhomova G.N., Solovyov A.A., Kravchenko V.V., Zakariev Z.Z., Pavlova N.A., Sorokoumov G.L. Halitosis problem. J. "Russian Dental Journal", 2007, No. 5, pp. 46-48.
11. Yanushovich O.O., Krikheli N.I., Dmitrieva N.G., Nikolaeva E.N.. Experience of using whitening toothpaste containing 10% carbamide peroxide in the complex treatment of halitosis. J. "Dentist", 2008, No. 6, pp. 22-26.
12. Means for the treatment and prevention of halitosis. J. "Dentist Practitioner", 2008, No. 1, pp. 42-46.
13. A disease that few people know about. J. "Wrigley Dental Programs" pp. 6-9.
14. Popruzhenko T.V., Shakovets N.V. Halitosis: issues of diagnosis, treatment and prevention of persistent bad breath. Educational and methodological manual. Moscow, 2006.
Prevention measures
Prevention can help prevent the development of halitosis: it is important to visit the dentist regularly, promptly treat oral diseases, and undergo professional teeth cleaning twice a year.
Prevention of halitosis also includes following individual oral hygiene recommendations. These include the following:
- selection of a toothbrush with a suitable degree of bristle stiffness. People with periodontal diseases - with soft ones, those who are prone to the formation of a large amount of soft plaque - with hard ones, but only if the enamel is strong and there is no hypersensitivity of the teeth. The average one is suitable for everyone else. You need to change your toothbrush every 1–3 months;
- using toothpaste without an abrasive effect - to prevent microdamage to the enamel and not increase the risk of developing dental diseases;
- Using dental floss and mouthwash after every meal;
- giving up bad habits - smoking, drinking alcohol, large amounts of tea and coffee;
- drinking enough water to prevent dry mouth and sufficiently moisturize the mucous membranes.
In case of chronic diseases of internal organs, it is necessary to pay attention to the prevention of complications and take therapy according to the doctor’s recommendations.
If you have a problem with bad breath, you can contact the dentists at STOMA clinics. The high qualifications of our specialists, as well as modern equipment, will help you quickly identify the cause of the symptom and prescribe effective treatment.
Sections we recommend
In these sections you will learn how to solve the problem of halitosis - bad breath:
- Treatment of caries
- Treatment of periodontitis
- Tartar removal
Bibliography:
- Popruzhenko T.V., Shakovets N.V. "Halitosis" - 2006
- Volosovets A.P. and co-authors “Acetone syndrome in children: a modern view of the problem” - 2009.
Author of the article: Mariam Arutyunovna Harutyunyan
Copywriter of the information portal Stom-Firms.ru. Specialization in translations and original articles on medicine and dentistry.
Do you talk a lot? Beware of halitosis
More often than others, halitosis affects workers of the so-called “conversational” genre - public politicians, lecturers, lawyers, radio show hosts... This happens due to the fact that during a conversation the oral cavity “dries out”, and active movements of the tongue help to “extract” the unpleasant odor from the most deeply hidden habitats of microbes. As you understand, in this case, neither candy nor chewing gum are helpful: diction suffers from them. And it’s not nice to chew or suck a pill during a performance. In this case, a traditional decanter of regular or mineral water will help.
How to get rid of unpleasant odor and prevent its occurrence
The fight against halitosis involves influencing the main pathogenetic factor of its development. And as we have already found out, the immediate substrate is anaerobic bacteria. Therefore, as part of comprehensive treatment, it is important to eliminate pathogenic microorganisms. However, taking antibiotics in this case is not justified, especially considering the huge number of side effects.
The basic method of improving the state of microflora in the mouth is regular professional dental hygiene. Primary rules:
- Brush your teeth twice a day (morning and evening);
- Individual selection of hygiene products, taking into account the anatomy of the teeth and their position in the dental arch. Assessing the activity state of the toothbrush bristles, regularly changing the toothbrush - at least once every 2 months;
- Mandatory use of an Irrigator and dental floss (a device that washes away food debris with a stream of water) to remove food debris from hard-to-reach areas where the fibers of a toothbrush cannot penetrate - between the teeth and in the subgingival area;
- Removing white plaque from the tongue using special brushes or spoon-shaped scrapers.
In addition to these rules, it is recommended to visit the dentist once every 6-8 months for professional oral care. The doctor will thoroughly clean hard-to-reach areas and remove tartar even at the microscopic level.
Timely treatment of caries and its complications is a mandatory rule that will help maintain fresh breath. Teeth affected by caries are a source of infection, which threatens not only the oral cavity, but can also spread to the area of the paranasal sinuses and pharyngeal tonsils. When the first symptoms occur (pain, visual changes in the gum contour or tooth color), you should seek specialized help.
Drying of the oral mucosa is another factor contributing to the proliferation of pathogenic microorganisms. To eliminate it, it is enough to follow the drinking regime. An ordinary person without kidney pathology is recommended to consume up to 2-2.5 liters of liquid per day, mainly in the form of pure water without gas.