Causes of allergic stomatitis
The main etiological factors contributing to the occurrence of allergic stomatitis can be divided into two categories:
- contact - substances and objects that have direct contact with the skin or mucous membrane of a person, as a result of which superficial irritations develop;
- non-contact - often products that a person eats, or medicines; allergies can also be caused by dust, mold bacteria, and pollen.
If we talk about the reasons for the appearance of contact allergic stomatitis, then dentures come first, which is associated with direct contact of the dental system and the oral mucosa. Avoiding the occurrence of such stomatitis can be quite simple - the main thing is not to skimp on dentures and install only systems made of high-quality materials that do not cause allergies. Another reason for the development of prosthetic stomatitis is pathogenic microorganisms that accumulate in large quantities in the denture bed. It is worth noting that even a minor injury to the mucous membrane is enough for the pathogenic process to begin to arise.
Also, the result of the appearance of such stomatitis can be medications that are often used to treat diseases of the gums and teeth, or medications that are absorbed into the mucous membrane for a long time (they need to be absorbed in the mouth).
The cause of non-contact allergic stomatitis is substances that, to one degree or another, can cause an incorrect reaction to their action, for example, a rash or redness, itching or burning may appear. Drugs that can cause such a reaction include antibiotics and sedatives.
Ecology and genetic predisposition may also be a likely cause of allergic stomatitis.
Causes and classification of the disease
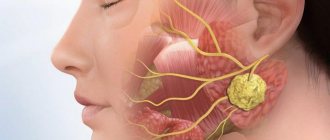
General allergies develop under the influence of an antigen, which can be food products, dust, pollen, skin particles from the body of animals. It is possible that an allergic reaction may occur after being bitten by animals, birds or blood-sucking insects: ticks, lice, mosquitoes.
General allergies develop under the influence of an antigen
Allergic stomatitis also has several factors that influence its manifestation. According to the causes of occurrence, there are five main types of this disease:
- medicinal;
- food;
- contact;
- toxic-allergic;
- autoimmune.
Let's take a closer look at each type.
Classification of allergic stomatitis
According to the form and nature of the course of the disease, allergic stomatitis is classified into the following types:
- catarrhal allergic stomatitis - considered the mildest form of the disease;
- catarrhal-hemorrhagic allergic stomatitis is a more complex form of the disease in relation to the previous type, and is a consequence of an allergy to medications;
- bullous allergic stomatitis - characterized by the appearance of ulcers, and subsequently - an erosive surface;
- erosive allergic stomatitis - a severe form of the disease, the result of drug intolerance;
- Ulcerative-necrotizing allergic stomatitis is the most complex form of the disease, characterized by the appearance of ulcers, subsequent tissue death and the formation of scars on the surface of the mucosa.
Allergic stomatitis is also classified according to the main cause of its occurrence:
- as a result of taking medications;
- as a result of a reaction to dentures and other factors in contact with the mucosa;
- as a result of damage to the mucous membrane by toxins produced by bacteria;
- as a result of genetic predisposition;
- as a result of complications of milder forms of the disease;
- as a result of dysfunctions of the main body systems.
According to the speed of development, allergic stomatitis is:
- immediate manifestation - characterized by rapid swelling of the tongue and enlargement of the palate, lips and gums;
- delayed manifestation - a long absence of symptoms after the allergen enters the body.
What is the danger of the disease
If stomatitis of allergic origin is not treated, osteomyelitis may develop - purulent-necrotic inflammation in the jaw bone, meningitis - inflammation of the meninges, or sepsis - a general infection of the body with pathogenic microbes that have entered the blood.
General allergies, combined with advanced allergic stomatitis, can be fatal.
The speed at which symptoms of allergic stomatitis appear depends on the intensity of its development. Thus, with the immediate type of development, the first signs of the disease appear within a few hours, and in some cases, minutes. The delayed type causes symptoms after a few days.
Symptoms of allergic stomatitis
Depending on the form of allergic stomatitis, the symptoms and clinical picture will differ slightly.
The simplest symptoms and course of the disease can be observed in the catarrhal form of stomatitis. Basically, the patient feels severe itching in the oral cavity. Sometimes there is a burning sensation. As symptoms increase, difficulties begin with chewing and swallowing food, to the point that this process becomes impossible. In this case, the patient loses his sense of taste and cannot distinguish between spicy and salty. There is a constant desire to drink water due to dry mouth.
When a patient has erosive-ulcerative stomatitis, the oral mucosa is covered with small blisters, which over time burst and form an open wound - an ulcer that has a tendency to bleed. Disruption of the microflora in the oral cavity leads to the appearance of pathogenic bacteria that penetrate the open ulcer and cause an increase in body temperature, lymph nodes may become inflamed, and soft tissues have severe swelling. Pain is present not only during eating, but also when the patient is at rest.
A more severe form of allergic stomatitis is ulcerative-necrotic; this type usually manifests itself against the background of a decrease in the protective function of the body. In this case, the symptoms are expressed in general weakness, constant headache and decreased appetite.
In addition, with any form of the disease, the patient has a characteristic taste in the mouth, and, accordingly, an unpleasant odor emanates. The inability to swallow causes increased accumulation of saliva in the mouth.
Manifestations of the disease
The disease negatively affects the functioning of the entire body. It doesn’t just cause inflammation of the mucous membranes—it also causes migraines, elevated body temperature, and lethargy. Many people notice dry mouth, severe pain when chewing, which is present even when the integrity of the tissues has not yet been compromised.
Saliva thickens, becomes viscous, more like foam. The gums, tongue, and inner surface of the cheeks may swell. All these symptoms deprive the patient of the opportunity to lead a normal lifestyle.
You shouldn’t wait for the disease to clear up. The sooner her treatment is started, the sooner her health will be normalized.
Diagnosis of allergic stomatitis
Any disease that is allergic in nature must be diagnosed using a differential method. Consultations with specialists from various fields of medicine (for example, immunologist, endocrinologist, allergist and others) are also necessary. Due to the fact that the disease affects the mucous membrane of the oral cavity, the primary treating physician is the dentist.
The first thing that is necessary to establish an accurate diagnosis is to perform allergy tests, study the patient’s complaints and the clinical picture of the disease. Next, a dental examination is carried out, during which the doctor determines the volume of saliva secreted, examines the oral cavity for ulcers, erosions and blisters, and evaluates dental systems and fillings (if any).
An important step in laboratory diagnostics is identifying the allergen; a biochemical study of saliva, determining the level of sensitivity of soft tissues and scraping to determine candidiasis are also necessary. In addition, the prosthesis is removed for some time to exclude prosthetic stomatitis, and its subsequent installation to confirm the diagnosis.
During diagnosis, the disease is differentiated from hypovitaminosis B and C, stomatitis caused by the herpes virus, and other diseases that have similar symptoms.
Content:
- Description of the disease
- Manifestations of the disease
- How does allergic stomatitis develop?
- Why does it occur
- Establishing diagnosis
- Fighting the disease
- How to reduce the risk of developing the disease
A dental disease in which the integrity of the oral mucosa is damaged - allergic stomatitis - occurs quite often in medical practice. It comes in different forms, so a person cannot always understand what caused the disease and what factors caused its negative symptoms.
Treatment of allergic stomatitis
When allergic stomatitis is diagnosed, treatment begins with identifying and eliminating the allergen - the substance that caused the body’s atypical reaction. If the disease is caused by an allergy to dentures or braces, then they are removed and replaced with better ones, the same thing happens with installed fillings.
If the disease is mild, then rinsing the mouth with disinfectants and taking antiallergic medications will be sufficient.
Severe forms of the disease are treated by intravenous administration of corticosteroid drugs; also, in the absence of allergies, diphenhydramine lotions are performed. Intravenous administration can be replaced by applying corticosteroid ointments if the effect is satisfactory. The application of agents that accelerate epithelial growth is also indicated. If the patient is in severe pain, a painkiller is prescribed.
The diet is balanced, excluding possible irritants and foods that can cause allergic reactions.
Itchy gums: what to do?
The first thing to do at the first sign of itching is make an appointment with your doctor. Only a specialist can identify the true cause of the disease and eliminate it through competent treatment.
The examination will help determine whether the gums are itchy after tooth extraction or whether there are other causes of the inflammatory process.
Itching itself seems to many people to be an insignificant reason to see a doctor, but it can be a side symptom of various diseases, the delay in treatment of which can lead to unpleasant consequences. Even if after using traditional medicine the itching has subsided, the disease, if it has already begun to develop, will definitely return after some time.
Forecast and prevention of allergic stomatitis
If allergic stomatitis was diagnosed at an early stage of the disease, then recovery will occur quite quickly. For any form of allergic stomatitis, the prognosis for recovery is favorable, but the time and technique of treatment will vary depending on the underlying cause of the allergy. Thus, the initial stages of the disease are treated in a period of no more than two weeks, all other forms - depending on individual reactions and the correctness of the chosen treatment method.
To prevent the development of allergic stomatitis, it is necessary to carefully monitor the condition of the oral cavity and perform regular hygiene procedures. If necessary, you should contact your dentist to help you choose the right toothpaste and brush. It is important to promptly treat such concomitant diseases as caries and various gum lesions. Fillings and dentures of inadequate quality should be replaced. If the patient has a genetic predisposition to stomatitis and allergies, care must be taken to ensure that contact with the allergen is minimized or completely eliminated (for example, you should not eat foods that can arouse allergies).
What causes gingivitis?
The disease occurs due to local and general factors:
- Poor oral hygiene
- Taking specific medications (for example, bismuth preparations)
- Chemical or thermal effects
- Hypovitaminosis
- Bad habits
- Infectious processes in the body
- Gastrointestinal diseases
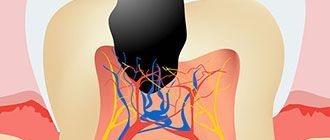
- Caries and its complications
- Decreased immunity
- Errors in dental treatment
- Malocclusions
- Radiation damage
The main cause of gingivitis in adults and children is the accumulation of dental plaque with its hardening into tartar. Leftover food, being an excellent breeding ground for bacteria, breaks down and causes an unpleasant odor. Microbial plaque contributes to gum injury, the impact of decay products of pathogenic microflora on the gums and impaired microcirculation.