- home
- Dental news
- Oral candidiasis
|
|
Candidiasis (thrush) is an infectious lesion of the mucous membrane caused by yeast-like microorganisms (fungi) of the genus Candida. This fungus is a normal part of the human microflora and can live both on the skin (not often), and on the mucous membranes or in the intestines. As a rule, in a healthy body, Candida is found in small quantities and does not cause any discomfort. But, under the influence of negative factors (decreased immunity, etc.), increased growth of the fungus begins and, accordingly, such unpleasant phenomena as itching, burning, and other symptoms of candidiasis appear. Most often, thrush occurs in children, especially infants, and the elderly. Various tissues and organs can be affected, including the mucous membrane of the oral cavity.
Signs of oral candidiasis:
- Increased sensitivity of the tongue and throat, pain upon contact with food and drinks;
- The appearance of swelling and white plaque on the surface of the lips, cheeks and tongue. After removing the plaque, a wound remains on the mucous membrane, which may bleed;
- “Cracks” may appear in the corners of the mouth and redness on the inside of the lips and cheeks.
- An increase in temperature and the appearance of small pustules on the mucous membranes of the lips and cheeks with a characteristic unpleasant odor are possible.
- If you have candidiasis, your mouth may feel tight and dry.
Causes of oral thrush
One of the most important factors influencing the appearance of thrush in the mouth is a decrease in immunity. The weakening of the body’s protective function leads to the uncontrolled growth of pathogenic microflora, and accordingly, symptoms appear. Most often, reduced immunity is observed in infants, the elderly, cancer patients, and those infected with HIV and AIDS. It is worth noting that if HIV infection is present in the body, the symptoms of the disease will be somewhat different - the fungus affects not only the oral mucosa, but also the genitals. Also, the “risk group” includes those whose bodies are often subjected to physical and psychological overload, stress, as well as those who regularly neglect healthy food and smoke a lot.
In addition to a decrease in immune status, the causes of oral candidiasis include:
- Lack of vitamins in the body, especially group B, vitamins C and PP.
- Taking medications that suppress the immune system, antibiotics and some other drugs that lead to disruption of the microflora. Hormonal contraceptives can also cause thrush.
- Pregnancy. Changes in the hormonal levels of the expectant mother can cause the active growth of Candida fungus.
- Chemotherapy and radiation therapy in the treatment of cancer.
- Chronic fatigue and stress, excessive physical activity, sleep disturbances.
- Alcohol and drug addiction, smoking.
- Injuries to the oral mucosa - small wounds in the mouth often cause an inflammatory process. Incorrectly chosen braces or dentures can cause especially a lot of trouble.
- Diseases of the gastrointestinal tract, diabetes mellitus, dysbacteriosis, pathologies of the endocrine glands, etc.
There is a possibility of contact infection with thrush - through kissing, sexual intercourse, or using shared hygiene items. Infection of newborns during childbirth also occurs (vertical infection from mother to fetus).
Skin candidiasis: symptoms and treatment
Forms of cutaneous candidiasis
In most cases, the symptoms are nonspecific and the diagnosis is made only based on the totality of all data (both clinical and laboratory).
The most common forms are:
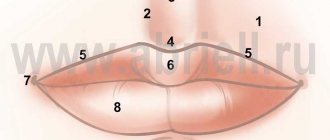
- Candidiasis seizures
- observed, as a rule, in people with malocclusions and the elderly. It looks like an easily removable white plaque in the corners of the mouth, with red smooth erosions underneath it. - Candidiasis of the red border of the lips
- reddened lips (usually the process is more pronounced on the lower ones) are thickened, peeling, swollen, cracks are possible. - Candidiasis of large skin folds
(inguinal-femoral, intergluteal folds and folds of the axillary region). - Interdigital yeast erosions
- most often occur between the 3rd and 4th, 4th and 5th fingers of the hands, rarely on the feet, and are characterized by the formation of eroded foci of a rich red color with a smooth, shiny, as if varnished surface, clear boundaries , with peeling of the epidermis. - Yeast paronychia
- affects the nail folds. - Nail candidiasis
- the nails thicken, detachment of the nail from the nail bed, splitting of the nail plate may occur, and the color of the nail changes (as with other onychomycosis). - Candidiasis of the palms
- occurs in two forms: 1) with rashes of small bubbles (vesicles); 2) with thickening and peeling of the skin. - Nipple candidiasis
is common in nursing women. In this case, red, irregularly shaped, flaky rashes appear in the area of the nipple areola, and sometimes cracks can form. - Candidiasis of the scalp
. The hair itself is not affected by Candida fungi, and changes in the scalp are similar to the manifestations of seborrheic dermatitis. - Candidal balanoposthitis
is characterized by damage not only to the mucous membrane, but also to the skin of the penis.
There are also candidiasis of the genitourinary organs (the well-known “thrush”) and systemic candidiasis, when (as a rule, against the background of serious illnesses) internal organs are affected, but this is a topic for other articles and, probably, other specialists.
Is skin candidiasis contagious?
Conditionally yes. Despite the fact that candida also exists in the microflora of healthy people, contact with an untreated patient with cutaneous candidiasis can trigger the onset of candidiasis in weakened patients or with some other problem that contributes to its occurrence. Agree, this is not a very likely, although not impossible, coincidence. So, although ordinary hygiene is sufficient in everyday life, if there are concerns (contact with the elderly, children, sick people), fungal prevention measures would be useful.
What to do?
Firstly, do not self-medicate under any circumstances. “True remedies” recommended by neighbors and other equally competent sources (including Internet forums) significantly complicate the diagnosis of the disease without bringing results. Many “well-known” remedies, for example Nystatin tablets, are completely useless for cutaneous candidiasis, since they are not absorbed from the intestines.
Secondly, sowing is necessary to determine not only the type of fungus, but also its sensitivity to antimycotics. Unfortunately, recently the frequency of detection of candida other than Candida albicans has increased, and this pathogen itself has become less sensitive to traditionally used drugs, which makes adjustments to treatment.
Thirdly, the most important thing in treatment is not the prescription of antifungal drugs systemically and/or locally (although this cannot be avoided), but mitigation of the effect or (if possible) elimination of those factors that contributed to the onset of the disease. It is clear that we cannot correct the consequences of serious diseases, but we can control obesity and diabetes, avoid prolonged contact with detergents, wean a child from biting his lips, and change into more suitable clothes.
Unfortunately, healthcare optimization does not always leave time for the doctor to analyze each specific situation in detail. However, in the case of cutaneous candidiasis (and, let me remind you, elimination of the pathogen is impossible, since it is found everywhere, including in the skin microflora of healthy people) - without taking measures aimed at the factors contributing to the development of candidiasis - a relapse of the disease is almost inevitable.
Therefore, if you have been diagnosed with cutaneous candidiasis and even cured quite quickly, this is still a reason to think about your state of health and have a thorough examination.
Good health!
Leonid Shchebotansky
Photo istockphoto.com
Products by topic: (glucometer), (glucometer test strips), (fluconazole), [product strict=”PIMAFUTSIN 2%”](pimafucin cream), [product strict=”nystatin”](nystatin ointment), [product strict ="clotrimazole"](clotrimazole)
How to treat oral candidiasis and how to avoid complications
Basically, dentists are involved in diagnosing and treating thrush, but you can also consult an immunologist, ENT specialist, endocrinologist or therapist; if a small child gets thrush, then, naturally, you need to consult a pediatrician. Treatment of oral candidiasis requires a comprehensive solution - the maximum effect is achieved by combining a medicinal approach and following a certain diet. The following are prescribed as drug therapy:
- Rinse with antiseptic agents (sodium tetraborate, boric acid, etc.). It is possible to apply antiseptic applications to the affected areas for a more effective effect of the drug. Also, when treating thrush, the body should be protected from the addition of other fungal infections - for preventive purposes, additional rinses containing broad-spectrum anti-inflammatory and antiseptic substances can be prescribed.
- Taking antifungal drugs. To achieve maximum effect, several different drugs (tablets, ointments, etc.) may be prescribed, alternating them during the treatment process.
- In severe cases of the disease, immunomodulatory and restorative drugs may be prescribed.
For successful treatment of candidiasis, one should not forget about a balanced and healthy diet, which will include a high content of B vitamins, as well as vitamins PP and C. During treatment, one should limit the consumption of flour, sweets and other foods rich in simple carbohydrates.
To prevent oral candidiasis, you should follow a few simple rules:
- Maintain oral hygiene;
- Minimize alcohol consumption, stop smoking;
- Adhere to proper nutrition, reduce consumption of glucose-containing foods;
- Do not take antibiotics without consulting your doctor;
- Visit your dentist regularly for preventive examinations and timely identification of any problems.
- When using dentures, clean them regularly and treat them with antiseptic drugs.
Based on: 1 votes
Candidiasis
Urogenital candidiasis is more common among women. About 75% of women have encountered manifestations of vulvovaginal candidiasis at least once in their lives, and in half of them the disease was recurrent. In women, candidiasis of the genitourinary tract is characterized by damage to the mucous membranes of the vulva and vagina, and less commonly, the cervix, urethra and bladder.
Candidal vulvitis and vulvovaginitis, which does not affect the urinary tract, have the following manifestations:
- abundant, milky-white color and cheesy consistency of vaginal discharge with an unpleasant odor;
- a feeling of irritation, itching or burning in or around the vulva, worse after urination, during sleep or after taking a bath;
- painful sexual intercourse, increased symptoms of irritation and a characteristic unpleasant odor after sexual intercourse.
With candidal vulvitis, yeast-like fungi damage the area of the external genitalia: the clitoris, labia minora and majora, and the vestibule of the vagina. Vulvar candidiasis can occur in typical and atypical clinical forms:
Typical forms of vulvar candidiasis include:
- catarrhal-membranous vulvitis of acute and subacute course;
- catarrhal chronic vulvitis.
Among the atypical forms of vulvar candidiasis are:
- leukoplakiform chronic vulvitis;
- kraurosis-like chronic vulvitis;
- asymptomatic pruriginous chronic vulvitis;
Mixed variants of acute fungal infection are also often found: candidal - bacterial, candidal - chlamydial, candidal - gonorrheal, candidal - trichomonas vulvitis.
The course of typical forms of vulvar candidiasis is characterized by burning and itching, the intensity of which increases before menstruation and decreases or disappears during the menstrual and postmenstrual periods.
The mucous membranes of the vulva affected by candidiasis are hyperemic and have a purple-bluish tint. Small punctate bubbles are visible on the mucous membranes, which upon opening form extensive erosions. The labia minora are covered with layers in the form of white cheesy films.
In the chronic form of vulvar candidiasis, congestive hyperemia and tissue infiltration, thickening and increased dryness are noted.
Atypical course of vulvar candidiasis is rare and occurs in a chronic form.
From the mucous membranes of the vulva, candidiasis can spread to the inguinal-femoral folds and the perianal area. Such manifestations are usually observed in chronic candidiasis in patients with myxedema, diabetes mellitus, and ovarian hypofunction.
Candidal vaginitis is characterized by the spread of fungal infection to the mucous membranes of the vagina and often the vaginal part of the cervix.
Vaginal candidiasis occurs in four main forms:
- candidal catarrhal-exudative-membranous vaginitis of acute and subacute course;
- mixed candidal-bacterial catarrhal-exudative vaginitis of acute and subacute course;
- candidal catarrhal subacute and chronic vaginitis;
- asymptomatic candidal chronic vaginitis.
With vaginal candidiasis, the mucous membranes are brightly hyperemic, covered with a creamy or loose crumbly coating. The walls and vaults of the vagina, as well as the vaginal part of the cervix, are eroded. The discharge is copious, cheesy or creamy in consistency, sometimes foamy and even purulent in nature with an unpleasant odor. Subjectively, patients note moderate pain, burning and itching in the vagina.
Candidal endocervicitis does not occur independently, but develops only in connection with vaginal candidiasis.
As a result of vaginal candidiasis, a fungal infection ascends through the external pharynx into the cervical canal. Often the cause of the development of candidal endocervicitis is inadequate ovarian function. In the typical course of cervical candidiasis, white crumbly lumps or white thick mucus are released from the cervical canal. The outside surface of the cervix is covered with whitish films. The erased form of cervical candidiasis is characterized by scanty milky mucous discharge.
Relatively rare manifestations of genitourinary candidiasis in women are candidal urethritis and cystitis. Acute candidal urethritis is characterized by constant dull pain in the lower abdomen and dysuric disorders: cutting, burning, frequent and painful urge to urinate. On examination, swelling and hyperemia of the urethral sponges and cheesy lumps at the external opening of the urethra are noted.
Acute cystitis with candidiasis is manifested by pain when urinating and frequent false urges.
Chronic candidal urethritis and cystitis, without exacerbations, occur with or without mild symptoms.
Recommended drugs
In the case of cutaneous candidiasis, topical medications are usually used. These include alcohol infusions and antifungal drugs. Prevention recommendations are standard - a balanced diet, a healthy lifestyle, taking care of yourself.
WE RECOMMEND YOU TO WATCH:
More about the pathogen
Candida fungi belong to the group of opportunistic microorganisms. They are found in soil, fruit tree bark, and vegetables. Candida is present in certain quantities on the skin of a healthy person and is excreted in urine, sputum, and excrement. What the result of the activity of microorganisms that cause cutaneous candidiasis looks like is shown in the photo.