Causes of gum inflammation
There are many causes of gum inflammation. They can be caused by systemic and local factors. Local ones include:
- mechanical trauma to the gums during brushing;
- formation of tartar;
- eruption of wisdom teeth;
- pulpitis and caries;
- poor oral hygiene.
Painful sensations may appear due to the root of the tooth affected by pulpitis or caries. The reason for this may be dental treatment, which resulted in inflammation of the gums. It may also be associated with canal injury and poor filling.
System factors include:
- diabetes;
- diseases of the stomach and intestines;
- hormonal disbalance;
- weakened immune system;
- reaction to taking medications.
What kind of toothpaste do you need?
One that affects the weak links in a person’s dental health. A few decades ago, toothpaste helped remove plaque and deodorize (freshen) breath. Today the list of problems that it can solve is much wider. On store shelves you can find types of toothpastes that differ in purpose and, consequently, composition.
Classification of toothpastes, their purpose
All pastes can be divided into 2 large groups. Hygienic – clean teeth from plaque, freshen breath. Designed for young children, as well as patients with a healthy oral cavity, without bad habits. Such patients visit the dentist only for a routine examination in order to hear from the doctor: “You are doing well, we’ll see you in six months.” The second group of pastes are therapeutic and prophylactic, that is, they are intended to solve certain problems. There are many species in this group.
Anticarious
Caries is a pathological process of tooth decay that can occur in both adults and children.
It is the fourth most common disease among people around the world. The use of such pastes is recommended for people with an increased risk of caries, after teeth whitening or when wearing braces. The chemical composition of the pastes makes the enamel more protected against the action of acids of caries-forming bacteria and inhibits the growth of pathogenic microbiome. High-quality anti-caries pastes contain a complex of minerals: hydroxyapatite, calcium, magnesium, phosphorus, fluorine. Fluoride is an important element in the prevention of caries; this element reliably seals minerals in the enamel. It prevents minerals from leaving the enamel uncontrollably. It is known that in the presence of fluoride, pathogenic microorganisms cannot actively reproduce. Anti-caries pastes must contain at least 1350-1450 ppm or 0.135-0.145% fluoride.
For sensitive teeth
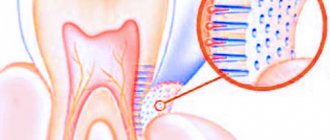
With hyperesthesia, sharp pain appears when exposed to temperature stimuli - cold foods, water or air. This happens due to the exposure of the dentinal tubules, which quickly transmit impulses and irritate the nerve endings closer to the pulp of the tooth. Hyperesthesia rarely resolves on its own, unless it occurs after dental procedures: teeth whitening, removal of tartar, or if the teeth have been “ground” for crowns or dentures. In other cases, treatment is necessary. And using paste will help complement it. Pastes for sensitive teeth usually contain hydroxyapatite, the main element that restores normal sensitivity. They should not contain chemical bleaching components, calcium carbonate; the inclusion of silicon oxide, lactic or plant enzymes is acceptable.
To “treat” gum disease
Bleeding gums are the first symptom of existing problems. Healthy gums do not bleed when brushing your teeth, much less eating. But if such symptoms appear, this is a reason to visit a doctor, and not just change hygiene products and items. Pastes for gums reduce the severity of inflammation due to the inclusion of medicinal plant extracts that have an astringent and antiseptic effect. They may include:
- chlorhexidine with antibacterial properties;
- extracts or decoctions of sage, chamomile, echinacea, calendula, oak bark have an anti-inflammatory and astringent effect;
- vitamins support metabolic processes, tissue restoration, and increase local immunity.
Some of these pastes, especially those containing chlorhexidine and other antiseptics, cannot be used for a long time and independently. They can only be recommended by a doctor and only for a certain period of time, otherwise you can get more harm than good.
Whitening toothpastes
Remember! Whitening toothpastes do not whiten. The maximum they can do is return the teeth to their original color, that is, remove pigmented plaque. They can act due to abrasives, sometimes coarse, and this indicator is reflected as RDA. For daily use, 75 RDA is recommended. But those pastes where this indicator is more than 100 are not recommended for long-term use. Enzyme whitening pastes are more gentle. They remove pigmented plaque more carefully and do not harm the enamel. Such pastes are recommended for occasional use by smokers, people with diseases of the digestive tract and kidneys, when tartar quickly forms.
How to choose pasta
When choosing a paste yourself, you need to pay attention to its composition.
It is better not to buy pastes with coarse abrasives: chalk, calcium carbonate, aluminum oxide. Give preference to those containing silicon dioxide, dicalcium phosphate, etc. Use pastes with triclosan and chlorhexidine with caution. And even if you use them, then no more than 2-3 weeks in a row. Pastes with sodium lauryl sulfate are not recommended for patients suffering from frequent stomatitis, especially chronic aphthous stomatitis. Prolonged and frequent exposure to this surfactant can cause exacerbations. Despite the composition of the paste, its focus will not work if you use the toothbrush incorrectly and do not follow the brushing time and recommended rules. Moreover, no paste or brush can remove 100% of all plaque, so you need to visit the dentist at least 2 times a year to remove tartar and carry out professional hygiene procedures.
Text: Yulia Lapushkina.
Symptoms
When gums become inflamed, symptoms appear that are severe. These include swelling, hyperemia of soft tissues, and pain when chewing food. An unpleasant odor from the mouth, bleeding gums, tooth decay, pus above the tooth, increased temperature, the formation of light plaque, and excessive sensitivity of the teeth may also appear.
In case of dental problems, an inflammatory process is observed in the lower gum, mainly in the area of the front teeth, as well as in the area of the wisdom teeth.
If prompt treatment is not provided, deep pockets in the gums and other complications may develop that can lead to tooth loss.
How to get rid of gum pain?
Unpleasant sensations in the gums in the first hours after dental treatment are normal. A good doctor will always warn the patient about such things after a dental procedure.
However, a distinction must be made between some discomfort and pain that is difficult to bear. Discomfort is characterized by unpleasant sensations, tingling, and sometimes slight pain in the treatment area during the first two days. The opposite is a state of unbearable pain, the inability to eat, rolling and throbbing pain. In this case, the patient cannot function normally: work or fall asleep.
Causes of pain after dental treatment
- Individual patient reaction to an anesthetic injection. Gums and soft tissues react differently to the action of the injected drug;
- Rejection of the installed filling. Soft tissues “do not accept” the filling installed by the doctor, signaling this with pain;
How to relieve gum pain at home
In any case, the patient is unlikely to be able to function normally, since the pain tends to increase: it becomes more frequent and more difficult for the person to bear. Therefore, it is better to visit the doctor again as soon as possible. If for some reason it is impossible to do this, then try to reduce the pain yourself.
- Try not to eat foods at high or excessively low temperatures. This will only aggravate the situation, since in the first time after treatment the gums are sensitive to external irritants;
- Brush your teeth only with a cool brush. There is a misconception that a warm toothbrush helps reduce gum pain. In fact, this will only increase the sensitivity of already inflamed tissues;
- Do not apply mechanical force to the gums. This applies to both the pressure applied when brushing your teeth and simple picking in your mouth out of curiosity. It is human nature to touch those places that hurt, so make sure that soft tissues are not touched by hands or other objects;
- Under no circumstances apply traditional painkillers or disinfectants to the gums - peppers, garlic, and so on.
- Rinse your mouth with a salt solution, a decoction of sage or chamomile. When rinsing, try to focus on the affected area. At the same time, do not forget that you should not abuse this procedure - rinse no more than three times a day;
- Crush one tablet of analgin and aspirin. Mix the resulting powder, pour it onto a cotton swab (or a cotton swab) and gently apply it to the inflamed area without pressing;
- If the pain is mild, then prepare the following solution: add 0.02 furatsilin to a full glass of water. Mix thoroughly and caress the inflamed area 3 times a day for 5 minutes.
Remember that these recommendations are intended to alleviate the patient’s condition and gain time to visit the doctor.
Therefore, even if you feel the pain easing, do not rush to refuse a visit to the clinic. After a short period of calm and cessation of home treatments, the pain may intensify again, so it is wiser to deal with the root cause of the inflammation in the doctor's office. You can find out more about the features of gum treatment among our services. MAKE AN APPOINTMENT
Gum pain in a child
Teeth growth
. In young children, unpleasant and painful sensations can be caused by teething. In this case, children constantly gnaw and bite objects, making it clear that they are “uneasy” in their mouth. If the cause of concern is teething, then make sure that the toys and special objects the child bites are treated with antiseptics to prevent infection. The best option would be to buy a special rubber “biting ring” for your child and treat it with an antiseptic.
Infection
. If a child experiences severe pain, he either cries or lets his parents know that he has pain “in the mouth.” This may be the cause of infection from constant bites of various objects. At home, you can temporarily use Nurofen or Viburkol. However, the best solution is to visit a doctor.
Tablets against pain in the gums:
- Analgin
. A common cheap pain reliever that is found in almost every first aid kit. Efficiency is average. - Nise.
This is a serious drug that specializes in muscle pain and post-traumatic consequences. - Ketanov
. The most effective drug against toothache. - Dexalgin
. A fast and long-lasting drug. - Baralgin
. An effective pain reliever. The effectiveness is average, since severe pain requires taking two tablets at a time. The patient is not recommended to exceed the norm of 6 tablets per day. - Nurofen.
In addition to relieving pain, it also directly affects the soft tissue of the gums. - Paracetamol. Used against pain, inflammation and fever. A cheap product that is in every first aid kit.
Why does the pain get worse at night?
Surely a person has noticed throughout his life that pain in the mouth (gums, teeth, throat) begins to worsen at night. More often a person notices this in two ways:
- Before sleep, there is an increase in pain.
- A man wakes up in the middle of the night in pain.
The peculiarity of such phenomena is that in the morning the unpleasant sensations subside. So what is the reason? The mystery lies in the nature of the process - inflammation. This process in the human body is regulated by the adrenal glands - glands near the left and right kidneys. In the evening and at night, the adrenal glands do not work, so the pain is felt more strongly. When morning comes, they are active again, which improves the person’s condition.
How to keep your gums healthy
As has already become clear, one of the causes of pain is the incorrect insertion of an artificial tooth or its rejection by soft tissues. But the fact is that it is wiser, in principle, not to bring the tooth to the point of removal or artificial replacement.
Firstly
, having natural healthy teeth is better than wearing artificial implants.
Secondly
, this will save the patient from possible pain and complications after the installation procedure, although it does not exclude the chance of pain in his own teeth.
Third
, if a patient receives an implant, this increases by half the chance that he will have another artificial tooth installed in the near future. The fact is that if the doctor finds one unhealthy tooth that needs to be removed, then there is a high probability that another similar one is “ripening” in the mouth, because this indicates the general level of oral hygiene of the patient.
Therefore, maintain oral hygiene: brush your teeth at least twice a day, select a suitable brush and toothpaste with the help of dentists, use rinses and dental floss. Also, remember to visit your dentist at least twice a year. Good luck!
We recommend you read it
What is the difference between periodontal disease and periodontitis?
How and how to relieve toothache at home
Pulpitis
Types of inflammation
As a result of gum inflammation, other oral diseases may appear, namely:
- periodontitis;
- stomatitis;
- gingivitis;
- pathologies of the oral mucosa associated with mechanical, chemical or physical damage;
- oral disease due to specific harmful microorganisms;
- damage to the mucous membrane as a result of allergies.
Pain in a tooth after a temporary filling is placed - normal or pathological?
If, after several days or a week of keeping a temporary filling with a medicinal drug under it, with the pulp preserved, intense pain continues, does not tend to decrease, increases with temperature and chemical stimuli, or signs of complications appear (sharp throbbing pain, swelling of the tissues surrounding the tooth, swelling of the cheek, signs of general intoxication, fever, enlargement, soreness of peripheral lymph nodes, etc.) – an urgent appointment is required to review treatment tactics.
It is concluded that there is severe inflammation of the pulp that is not amenable to biological treatment and that it must be removed. In this case, a devitalizing arsenic-containing or paraformaldehyde paste is placed for a period depending on its composition (from two days to a week), followed by depulpation and cleaning of the canals. After placing such pastes under a temporary filling, after the required time has passed, depending on the type of paste, the tooth should stop hurting due to the death of the nerve. If this does not happen, we can assume that the drug was poorly delivered and had a bad effect on the pulp, or the pulp is completely necrotic and the canals are filled with pus (in this case, swelling of the gums is added to the clinical symptoms), in such cases you should urgently consult a specialist.
In case of any progression of pain or the addition of other symptoms, urgent treatment is necessary with removal of the filling, re-cleaning of the canals and long-term step-by-step treatment, and in some cases even surgical treatment.
Features of pain under a temporary filling in various diseases
The different nature of pain is, to one degree or another, inherent in different inflammatory processes.
Thus, a characteristic sign of acute pulpitis is intense pain in the tooth, often manifesting itself in the form of attacks lasting up to half an hour, worsening at night, when eating food of contrasting temperature, radiating to neighboring areas.
Chronic pulpitis is manifested by mild, spontaneously occurring periodic pain, also associated with eating food of contrasting temperature.
Intense, acute, increasing twitching, paroxysmal pain is also characteristic of acute purulent periodontitis.
Gradually developing, aching, bursting pain with the sensation of an “overgrown tooth” is characteristic of chronic periodontitis.
Mild aching pain is characteristic of ongoing inflammation in the pulp and at the top of the tooth during the action of devitalizing pastes.
Of course, it is categorically impossible to completely rely on the nature of the pain and try to diagnose yourself; you should definitely consult a qualified dentist, who, based on examination data and objective research methods, will accurately diagnose and carry out appropriate treatment.
Treatment at home
To treat inflammatory processes in the gums, you can resort to home remedies.
Rinsing gums:
- Chlorhexidine. The medicine in the form of a solution is used to disinfect the oral cavity from harmful microorganisms. You need to rinse 5 times a day.
- Rotokan. A drug containing herbal ingredients. You need to rinse your mouth 3 times a day.
- Furacilin. Antibacterial mouth rinse every 2 hours.
Ointments and gels:
- Holisal. Copes with swelling, suppresses pain.
- Periodonticide. The composition contains vegetable oils. Apply to gums 2-3 times a day for 8-10 days.
- Heparin ointment. Helps achieve an anti-inflammatory effect. You need to rub it into your gums 2 times a day.
Medicinal toothpastes:
- Lakalut active. Reduces swelling and has an antiseptic effect.
- Parodontax. Copes with inflammatory reactions and swelling.
Gum massage
To improve blood flow in the gums, you can massage with a toothbrush while brushing your teeth or with your hands.
When massaging with your fingers, you need to stroke, rub, squeeze and squeeze the gums. It is worth doing a massage every day in the morning and evening.
Vitamins
In addition to treatment with ointments and gels, you should take care of taking vitamin supplements that will help maintain oral health. Inflammation of the gums may be associated with a lack of vitamins A, PP, D, as well as the minerals calcium and phosphorus.
How does peroxide affect teeth?
Peroxide is a very strong oxidizing agent, which, on the one hand, effectively whitens teeth, and on the other, increases their sensitivity. Therefore, those who already complain about the sensitivity of their teeth should avoid this method.
During the whitening process, peroxide penetrates the tooth enamel and dentin of the teeth, and begins to lighten them. Moreover, a good result is visible after a couple of weeks of use.
Many dentists question the advisability of using peroxide for whitening, but many ordinary citizens, due to the effectiveness and low cost of this method, prefer to whiten their teeth with peroxide.
Teeth whitening with hydrogen peroxide at home: basic methods
- There are several basic ways to use peroxide for DIY whitening.
- Peroxide solution with water. Prepare the solution: dilute 3% peroxide with ordinary purified water in a 1:1 ratio. Brush your teeth in the usual way (it is advisable to use fluoride paste), then rinse your mouth with the prepared solution, then thoroughly with plain water. This remedy should be used twice a day. After a week, you need to take a break for at least a couple of weeks, then the procedure can be started again.
- A mixture of peroxide and toothpaste. Mix a teaspoon of toothpaste and a teaspoon of hydrogen peroxide (3%). Brush your teeth with the mixture twice a day, take a break after seven days. You need to understand that even if this method does not show such an impressive result as the previous one, it is more gentle and gentle on tooth enamel.
- Peroxide rinse. Take 30 ml (about two tablespoons) of undiluted 3% peroxide and rinse your mouth for sixty seconds. Foam appears - don’t be alarmed, this is how it should be. After this, you need to spit out the solution, rinse your mouth thoroughly with water and be sure to brush your teeth thoroughly. Under no circumstances should you swallow the solution!
- A mixture of peroxide and tooth powder. You need to take in equal proportions, for example, a teaspoon, peroxide and tooth powder. Mix and use instead of toothpaste a couple of times a day. Then rinse your mouth thoroughly.
- A solution with the addition of soda and salt. Prepare a solution using 1 part peroxide (3%) and two parts water, add soda and salt. After this, rinse your mouth with the resulting solution and brush your teeth using a soft brush.
- A mixture of baking soda and hydrogen peroxide. Prepare a paste of 15 ml of baking soda and 10 ml of hydrogen peroxide. To give the resulting solution a pleasant taste and fresh aroma, you can add a drop of mint extract or a little toothpaste to it. Apply the resulting paste onto your teeth using circular movements and wait a couple of minutes. Rinse thoroughly with water and brush with toothpaste.
- Pure peroxide. Used to remove plaque from a specific problem area. To do this, dip a cotton swab in peroxide and apply it to an individual tooth, rinse and use toothpaste.
Treatment at the dentist's office
In dentistry, doctors may resort to treatment with medications or prescribe surgery.
When gums become inflamed, antibiotics are prescribed to stop the spread of infection. In addition to antibiotics, you can use anti-inflammatory drugs: Ibuprofen, Ketoprofen, Ketorolac.
Surgical intervention is necessary if the neck of the tooth is exposed, which occurs as a result of prolonged inflammation of the soft tissues. Surgical methods include:
- Flap surgery. Necessary in cases of severe periodontitis, when there is a possibility of being left without a tooth.
- Open curettage. Performed for the treatment of periodontitis. Allows you to get rid of harmful microorganisms.
- Excision of the hood. It is carried out in case of severe eruption of wisdom teeth, which leads to inflammation of the gums.
Trigeminal facial pain: systematics of clinical forms, principles of diagnosis and treatment
Facial pain, which includes pain on the surface of the face and/or in the mouth (orofacial pain), is one of the most common types of pain. Most often, orofacial pain manifests itself as acute dental pain, which usually regresses after dental treatment. However, in a number of cases, facial pain itself (prosopalgia) is noted, manifested by chronic or recurrent pain, often resistant to various methods of conservative treatment. A kind of primacy in severity belongs to trigeminal facial pain, especially trigeminal neuralgia and deafferentation trigeminal neuropathy, during exacerbation of which the severity of pain is many times greater than the intensity of acute toothache familiar to most people.
Taxonomy of trigeminal prosopalgia
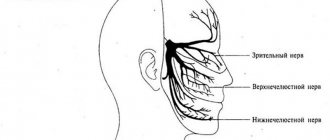
Trigeminal prosopalgia (Greek prosopon (face) + algos (pain)) includes facial pain caused by damage to the trigeminal nerve. From the point of view of topical diagnosis, the development of any form of trigeminal prosopalgia is associated with damage to the peripheral trigeminal neuron - the peripheral trigeminal branches, the sensory trigeminal ganglion (located at the base of the skull), the sensory root of the trigeminal nerve that follows it in the direction of the brain stem, as well as those entering the brain stem sensory trigeminal fibers and sensory nuclei of the trigeminal nerve (
).
Despite the difference in the symptomatology of the clinical forms of trigeminal prosopalgia, the features of facial pain are of primary importance for their differentiation, in some cases manifested by prolonged (constant) pain, and in others in the form of paroxysms of pain. Paroxysmal forms of trigeminal pain are traditionally referred to as neuralgia, and non-paroxysmal forms - trigeminal neuropathy. However, non-paroxysmal postherpetic facial pain is also called neuralgia. These forms of facial pain—neuralgia and trigeminal neuropathy—fundamentally differ in their approaches to treatment.
Paroxysmal trigeminal prosopalgia
Paroxysmal facial pain, lasting from several seconds to several minutes, is manifested by trigeminal neuralgia (typical trigeminal neuralgia), trigeminal neuralgia due to multiple sclerosis, and symptomatic trigeminal neuralgia arising from a tumor lesion of the trigeminal nerve.
Until recently, trigeminal neuralgia, not associated with multiple sclerosis and tumor lesions of the trigeminal nerve, was called idiopathic, i.e. occurring for no apparent reason. However, as it was established as a result of serial neurosurgical interventions, the main etiological factor of typical trigeminal neuralgia is compression of the sensory root of the trigeminal nerve by an atypically located arterial or venous vessel.
Trigeminal neuralgia
Trigeminal neuralgia is the most common form of paroxysmal (paroxysmal) facial pain. It is also considered the most excruciating type of facial pain. It manifests itself as attacks of sharp, high-intensity pain in the area of innervation of the trigeminal nerve. The cessation of an attack of facial pain within a few tens of minutes after taking the anticonvulsant carbamazepine radically distinguishes trigeminal neuralgia from most other types of chronic pain. The symptoms of trigeminal neuralgia undergo significant changes as the pain syndrome increases and regresses, reaching its greatest severity at the height of the exacerbation period.
In secondary (symptomatic) forms of trigeminal neuralgia, which arise from tumor damage to the trigeminal nerve, already at the first stage of the disease symptoms may be observed that differ from the typical clinical picture.
Non-paroxysmal trigeminal prosopalgia
Non-paroxysmal trigeminal prosopalgia, manifested by prolonged facial pain, as well as sensitivity deficit (hypesthesia, anesthesia) in the facial area, includes various clinical forms of trigeminal neuropathy, including postherpetic neuralgia (). Most often, the development of trigeminal neuropathy is associated with obvious etiological factors - trigeminal herpes zoster and traumatic injury to the trigeminal nerve. In some cases, trigeminal neuropathy is one of the early manifestations of systemic diseases, in particular systemic scleroderma, systemic lupus erythematosus, sarcoidosis and Lyme disease.
Traumatic trigeminal neuropathy
It is the main form of trigeminal neuropathy, the clinical signs of which are non-paroxysmal facial pain, sensory impairment (numbness) and, very rarely, motor impairment. As a rule, the acute development of these symptoms has an obvious relationship with local pathological processes and iatrogenic effects in the maxillofacial area.
The first sign of traumatic trigeminal neuropathy is acutely developed sensory insufficiency - from mild hypoesthesia to anesthesia, limited to the innervation zone of the affected sensory branch. Subsequently, paresthesia (a feeling of “pins and needles”) and/or non-paroxysmal pain occurs in the same area of the face. Symptoms of sensory loss that accompany facial pain may persist significantly longer than facial pain. In the affected area, hyperesthesia is often detected, as well as pain on palpation of limited areas of facial skin.
Postherpetic trigeminal neuralgia
Trigeminal postherpetic neuralgia is persistent facial pain and/or burning and itching that persists from the time herpetic lesions develop or occurs several weeks after the lesions resolve (delayed postherpetic neuralgia).
Trigeminal postherpetic neuralgia most often develops in patients over 60 years of age. Its occurrence is usually facilitated by:
- late seeking medical help during the period of acute herpes zoster;
- presence of concomitant pathology;
- complicated resolution of rashes - rashes with a hemorrhagic component and secondary pyoderma;
- pronounced residual sensory deficit (“numbness” of the skin after resolution of the rash).
Deafferentation trigeminal neuropathy (prosopalgia)
Deafferentation facial pain (prosopalgia) is the most severe form of trigeminal lesion, manifested by highly intense facial pain, often resistant to conservative therapy, and severe sensory impairment. Develops as a result of significant damage (destruction) of the peripheral or central structures of the trigeminal system.
The concept of “deafferentation trigeminal prosopalgia”, as a general syndromological definition, was proposed by Yu. V. Grachev and Yu. A. Grigoryan (1995) to designate a special form of facial pain that develops as a result of deafferentation in the sensory system of the trigeminal nerve. The pathophysiological term “deafferentation” (de- + lat. afferentis bringing), literally means the separation of the receptor zones of peripheral nerves from the central sensory structures, due to a violation of the integrity or conductivity of nerve fibers.
Typical peripheral forms of deafferentation trigeminal prosopalgia are postherpetic, tumor and iatrogenically caused facial pain (caused by destruction of the ganglion and trigeminal nerve root), and central are two quite rare forms caused by syringobulbia and medulla oblongata infarction.
Diagnosis of trigeminal prosopalgia
The examination of a patient experiencing facial pain should begin with a systematic medical interview, including clarification of the clinical characteristics of the pain and analysis of anamnestic data (
).
The presence of facial pain requires a detailed study of the function of the cranial nerves, and also makes certain additions to the traditional neurological examination. Objective signs of damage to the nervous system of the face are sensory disturbances in the orofacial region - trigger zones, areas of increased and/or decreased sensitivity (Fig. 2, 3), local autonomic disorders, as well as the presence of local palpation pain.
| Rice. 2. Pattern (model) of sensory disturbances characteristic of exacerbation of paroxysmal trigeminal prosopalgia - neuralgia | Rice. 3. Pattern (model) of sensory disturbances characteristic of exacerbation of non-paroxysmal trigeminal prosopalgia - neuropathy |
When conducting palpation examination of the facial area, it is necessary to distinguish between “neuralgic” and “myofascial trigger” (English trigger).
- Neuralgic trigger points or zones (in patients with trigeminal neuralgia) are hyperexcitable areas of the skin and mucous membrane, with mechanical irritation, including light touch, causing a painful attack. At the same time, strong pressure, usually applied by the patient himself, not only does not cause pain, but in some cases leads to a decrease or disappearance of pain.
- Myofascial trigger points (essentially pain points) are located in the soft tissues of the face in the projection of the masticatory muscles. “Pressing” on them is accompanied by localized or radiating pain.
Establishing a specific form of trigeminal facial pain, which usually requires an interdisciplinary clinical examination, involves excluding a number of forms of orofacial pain not associated with damage to the trigeminal nerve, in particular temporomandibular (arthrogenic and myofascial), symptomatic (ophthalmo-, rhino- and odontogenic) and psychogenic prosopalgia.
Treatment of trigeminal prosopalgia
The complexity of treating patients with trigeminal facial pain is due to the need to determine differentiated treatment approaches due to the ineffectiveness of the use of conventional analgesics for certain forms of trigeminal prosopalgia, the frequent need to change standard treatment regimens and, in some cases, the development of “pharmacoresistant” forms of facial pain that require surgical treatment.
The ineffectiveness of traditional analgesics (for example, NSAIDs) prescribed in connection with the development of trigeminal facial pain is an indication for the use of drugs from other groups, in particular carbamazepine, gabapentin or amitriptyline, which have analgesic activity in a number of forms of prosopalgia (scheme of differentiated therapeutic approaches for paroxysmal and non-paroxysmal trigeminal prosopalgia is presented in
).
Over the past few decades, carbamazepine has remained the most effective and affordable drug in the treatment of patients with trigeminal neuralgia. At the same time, the maximum effectiveness of carbamazepine (as a “monotherapy”) appears in the initial period of the disease. The main indication for the use of carbamazepine is paroxysmal pain, covering the area of innervation of the trigeminal nerve. The daily dose of carbamazepine during an exacerbation of trigeminal neuralgia is usually 600–1200 mg (with a 3–4-time dose of the usual dosage form or 2 times of the retard form), but with uncontrolled use by a doctor it often exceeds 2000 mg/day. As neuralgia regresses, a transition is made to maintenance doses of carbamazepine and its gradual withdrawal when facial pain disappears. If there are contraindications for the prescription of carbamazepine or its forced withdrawal, gabapentin is used as an alternative remedy for the elimination of paroxysmal trigeminal pain.
Gabapentin (Gabagamma) is an anticonvulsant that has an analgesic (GABAergic-like) effect. Obviously, this explains its effectiveness in the treatment of patients with neuropathic pain, including paroxysmal and non-paroxysmal trigeminal prosopalgia. Indications for the use of gabapentin (Gabagamma) are paroxysmal facial pain in trigeminal neuralgia and trigeminal neuralgia caused by multiple sclerosis, as well as subacute and chronic non-paroxysmal pain (including deafferentation) in herpetic and traumatic trigeminal neuropathy. The daily dose of Gabagamma in patients with trigeminal prosopalgia can range from 300 to 1500 mg, with a dosage frequency of at least 3 times a day. Gabagamma is used for a long time and is gradually withdrawn. In general, the use of gabapentin (Gabagamma) is considered safer than carbamazepine and especially amitriptyline.
Amitriptyline is a tricyclic antidepressant that is a norepinephrine and serotonin reuptake inhibitor. This drug is widely used for the treatment of postherpetic neuralgia, especially accompanied by a burning sensation. The analgesic effect of amitriptyline usually develops within 1–2 weeks. To reduce the sedative and anticholinergic effects of amitriptyline, treatment begins with small doses of the drug - 10 mg 2-3 times a day (especially at night), gradually increasing the daily dose (due to evening administration) to 75-100 mg. If amitriptyline is insufficiently effective and facial pain persists, gabapentin (Gabagamma) is indicated.
Treatment of patients with damage to the trigeminal nerve also includes the use of high doses of B vitamins in the form of multicomponent preparations “Milgamma” and “Milgamma compositum”. The composition of the drug "Milgamma" (solution for intramuscular administration) includes 100 mg of thiamine and pyridoxine, 1000 mcg of cyanocobalamin and 20 mg of lidocaine. Milgamma compositum is available in the form of tablets containing 100 mg of benfotiamine and pyridoxine. The effectiveness of Milgamma in the treatment of patients with neuropathic pain is associated with inhibition (probably serotonergic) of nociceptive impulses, as well as acceleration of the regeneration of axons and the myelin sheath of peripheral nerves. The regimen for using Milgamma for trigeminal facial pain includes: prescribing Milgamma in the form of a solution for intramuscular administration - 2 ml daily, for 10 or 15 days, then Milgamma compositum - orally, 1 tablet 3 times a day, for 6 weeks.
Yu. V. Grachev , Doctor of Medical Sciences, V. I. Shmyrev, Doctor of Medical Sciences, Professor, Scientific Research Institute of Advanced Promotion of the Russian Academy of Medical Sciences, State Medical University of the Administration of the President of the Russian Federation, Moscow