Forms of neuralgia of the facial nerve
- neuritis – minor inflammation of the facial nerve (or part of it),
- paresis is a partial lesion in which weakness of the facial muscles and slight numbness are observed. This disease usually falls into the neurological category. But, like complete paralysis, it can be a consequence of advanced neuritis,
- paralysis - complete defeat. This is a severe stage, in which there is numbness of the face (usually one part of it) and blocking of muscle motor activity.
Symptoms of neuralgia
- tingling or sharp “sliding” pain,
- numbness of a certain part or the entire half of the face, lack of sensitivity and motor activity,
- drooping eyelids and skin around the eyes,
- drooping corners of the lips (on the side where muscle paralysis is observed),
- smoothing out wrinkles on the cheeks and forehead,
- pronounced facial asymmetry.
Causes of neuralgia
- viral infection or inflammatory processes (ear, throat, nose),
- hypothermia,
- inflammatory processes in the roots of teeth and bone tissue of the jaw,
- nerve injury during tooth extraction or installation of implants,
- injury from a needle during the administration of anesthesia,
- jaw injuries,
- old age and natural aging of the body.
The facial nerve belongs to the group of cranial nerves (along with the trigeminal nerve, whose branches are the mandibular and maxillary nerves). It also consists of many branches that run through almost the entire human skull. Depending on which branch is affected, the numbness of a certain part of the face will depend. In relation to implantation or complex surgical interventions, it is the trigeminal nerve that can be damaged.
How to distinguish pulpitis from other diseases?
Many dental diseases are accompanied by pain. But with pulpitis they differ in some characteristic features.
Pulpitis and caries
With caries, pain appears only when exposed to thermal or chemical irritants. If the irritant is eliminated, the pain syndrome immediately stops. With pulpitis, pain most often occurs for no reason. If it is caused by an irritant, then after its elimination the pain disappears no earlier than after a quarter of an hour.
Pulpitis and trigeminal neuralgia
Usually, with pulpitis, the severity of pain is much less than with neuralgia. But sometimes the severity of pain in these diseases is comparable. The difference is that with neuralgia the pain syndrome disappears or is greatly weakened at night, while with pulpitis it intensifies.
Pulpitis and periodontitis
With pulpitis, percussion and biting do not cause pain. With periodontitis, any of these actions causes severe pain.
X-rays will help distinguish between these diseases. With pulpitis, it will not show any pathologies, but with periodontitis, changes will be noticeable.
But you should not try to diagnose and treat pulpitis on your own, as this can cause various complications and lead to tooth loss. If you experience the slightest pain, you should contact a dental clinic.
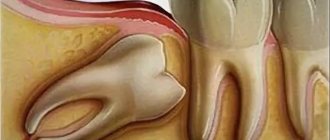
Nerve damage after tooth extraction
As a rule, this problem arises during complex tooth extraction, namely, dystopic or impacted, that is, located inside the bone tissue and has not completely erupted. Removing such teeth requires sawing the bone and using special forceps. If the load is too heavy and the nerve is located close, the doctor may touch it.
The prognosis in such a situation is usually positive - the condition of the nerve is restored after therapy.
Trigeminal neuralgia as a complication of implantation
Unfortunately, one of the fairly common causes of damage to the facial (more precisely, trigeminal) nerve is dental implantation. According to recent studies, the frequency of such complications at this time does not exceed 2.95% (that is, it occurs in 5 out of 169 patients), and only 1.7% of patients are diagnosed with permanent neuropathy, requiring microsurgical correction of the situation1. If the implant is incorrectly selected in length, with increased pressure during its installation, there is a high risk of damage to one of the branches of the trigeminal nerve (passing on the lower or upper jaw). The result is pain or numbness in a certain area, long-term rehabilitation.
Injuries are caused by compression of a given nerve, its stretching, partial or complete damage. In the case of sprain or compression without compromising the integrity of the trigeminal nerve, the sensations pass quite quickly - within up to 7 days as blood circulation in the bone tissue improves. But if there was partial damage to the fibers of the nerve bundle, then the rehabilitation process can take from 14 days to 6 months. In cases of severe trauma, implants may need to be reinstalled because the body of the implant interferes with the restoration of axons (processes) in the nerve bundles.
In our clinic, before the operation, careful computer planning of the placement of implants is carried out, after which surgical templates are printed, protecting the patient and the doctor from incorrect installation of implants. Immediately, or the next day after the operation, a control computed tomography is performed, at which the control commission (consilium of doctors), in accordance with international quality assessment protocols, compares the placement of implants with the original plan and makes a conclusion about the success of the operation, or makes recommendations to the attending physician on the need to take additional measures.
Important! Do not confuse nerve damage with compression on it that occurs in the bone as a result of swelling after the installation of implants located close to the nerve endings. Compression goes away along with swelling and numbness in this situation is a normal reaction. Most often, such symptoms typically appear 2-3 days after multiple implantations; they are a normal reaction to tissue injury when screwing in implants and damage to intraosseous capillaries. Improvements will be noticeable almost immediately after installing the prosthesis on the implants and activating the chewing load, and with it the restoration and blood circulation in the bones.
Please note that there is no point in hiding the fact of damage to the trigeminal nerve for the doctor and the clinic; it will reveal itself anyway - this is the first thing. Secondly, even if this happened, the consequences are eliminated by properly selected therapy and joint work between the doctor and the patient. Yes, if damage occurs, then the patient will have to undergo quite a long period of rehabilitation (up to 6 months), but in difficult clinical situations of complete absence of teeth and low quality bone tissue, the doctor works in very limited conditions, so, unfortunately, some consequences but not life-threatening and health dysfunction cannot always be avoided.
Expert opinion
Nikolay Vladimirovich Namdakov Maxillofacial surgeon, implantologist, orthopedist Work experience 17+
“During one-stage implantation, we very often use elongated implant models that are installed in the deep parts of the bone tissue. Naturally, this increases the risk of damage to the nerves, which in this case are located very close to the implants. However, in our work we use three-dimensional visualization - we carefully study the implantation process in a computer program, where we set all the parameters of the jaw system of a particular patient. This allows us to eliminate the possibility of damage to the facial nerve during surgery, even in difficult clinical conditions of bone atrophy.”
Causes of toothache without caries
If a tooth hurts, but there is no caries, the cause of the symptom should first be sought in other dental diseases. Painful sensations to one degree or another are characteristic of the following pathologies:
- Pulpitis is an inflammatory process that affects the nerve tissues of the tooth, which are located inside the dentin. It usually develops due to untreated tooth decay. It can also occur under a filling. Inflammation makes itself felt by spontaneous pain, which is prolonged. The pain is sharp and acute, and it is usually not possible to eliminate it with the help of analgesics. The tooth hurts very badly at night. If pulpitis becomes chronic, the pain becomes aching, but not so intense. As a rule, because of this disease the pulp has to be removed. The tooth becomes dead and noticeably darker.
- Periodontitis is inflammation of the tooth root. Occurs on intact (untreated) teeth, after trauma, due to the spread of a cyst, as a result of infection, or under a filling. The pain appears during eating, and during exacerbation, it radiates to neighboring teeth. The pain is aching in nature, and gumboil may develop. Acute purulent periodontitis is accompanied by a general deterioration in health, weakness and fever.
- Periodontitis is an inflammatory lesion of the tissues surrounding the tooth. With this disease, periodontal pockets are formed and gum recession is observed. Because of this, teeth become more sensitive and react painfully to external stimuli. Other signs of periodontitis include itchy gums, bleeding and bad breath. The tooth hurts especially badly when pressing and chewing food, and sometimes it becomes loose. The advanced form of the disease is treated surgically.
- Gingivitis is an inflammatory disease of the gums that causes pain in one or more teeth. If suppuration begins in the gum pockets, bad breath appears, the tooth begins to loosen, and the gums bleed. Pain occurs suddenly, for example, during chewing food, especially hot, cold and sour.
- A dental cyst is a new formation between the tooth root and the jaw bone; it looks like a sac filled with pus. The disease is accompanied by aching pain, the tooth hurts especially severely when pressed or exposed to hot food or drinks. A cyst can be detected using radiography. It is treated surgically. After removal, pain, increased sensitivity and swelling of the gums may persist for some time.
- Impacted wisdom tooth. Unerupted “eights” often begin to grow to the side; they often put pressure on neighboring teeth, causing pain. This process is also accompanied by inflammation of the gums. The pathology is easy to diagnose by the location of the pain - behind the last molar, that is, at the very edge of the jaw.
Also, toothache is accompanied by non-carious enamel lesions, for example, erosion, increased abrasion or dysplasia. The tooth hurts when exposed to sour or sweet foods, during contact with a toothbrush or dental instrument. During differential diagnosis, the doctor must distinguish caries from the listed diseases and prescribe appropriate treatment. It is almost impossible to accurately determine the pathology only by the nature of the toothache.
Treatment of lesions of the facial or trigeminal nerve
The first thing to do (if the cause of the lesion is not known) is to undergo a full diagnosis and find out why this problem occurred. This will allow the doctor to choose the right treatment tactics.
It is very important to consult a doctor as soon as possible if you experience the first symptoms of complications after tooth extraction or implant installation. If treatment is started promptly, complete restoration of muscle functionality can be achieved. It is also important that if numbness persists for 3 months and no measures have been taken, it will most likely not be possible to restore the affected nerve, since persistent degenerative changes develop in it.
Diagnostics
- a blood test to check for a viral or bacterial infection that could cause nerve damage,
- CT or MRI of the skull and brain to determine the affected area,
- electromyography, which involves direct impact on nerve endings to determine the level of disturbance in the passage of impulses along the nerve.
Treatment
- drug therapy: this group includes anti-inflammatory, painkillers and anticonvulsants, as well as antidepressants and sedatives.
- physiotherapy: facial gymnastics, massage performed by specialists, electrical stimulation and acupuncture,
- microsurgery: surgery is performed to restore the integrity of the damaged nerve. This is a fairly serious surgical procedure that should be performed by a professional surgeon. Surgery is an extreme method of solving the problem; it is needed only in case of serious damage and if the first two options did not bring any result.
Surgery
As a rule, patients with trigeminal nerve pathology are offered surgery after 3-4 months of unsuccessful conservative treatment. Surgical intervention may involve eliminating the cause or reducing the conduction of impulses along the branches of the nerve.
Operations that eliminate the cause of neuralgia:
- removal of tumors from the brain;
- microvascular decompression (removal or displacement of vessels that have dilated and put pressure on the nerve);
- expansion of the exit of the nerve from the skull (the operation is performed on the bones of the infraorbital canal without aggressive intervention).
Operations to reduce the conductivity of pain impulses:
- radiofrequency destruction (destruction of altered nerve roots);
- rhizotomy (dissection of fibers using electrocoagulation);
- balloon compression (compression of the trigeminal ganglion with subsequent death of fibers).
The choice of method will depend on many factors, but if the operation is chosen correctly, attacks of neuralgia will stop. The doctor must take into account the patient’s general condition, the presence of concomitant pathologies, and the causes of the disease.
Surgical techniques
- Blockade of certain sections of the nerve. A similar procedure is prescribed in the presence of severe concomitant pathologies in old age. The blockade is carried out using novocaine or alcohol, providing an effect for about a year.
- Ganglion block. The doctor gains access to the base of the temporal bone, where the Gasserian node is located, through a puncture. Glycerol is injected into the ganglion (glycerol percutaneous rhizotomy).
- Transection of the trigeminal nerve root. This is a traumatic method, which is considered radical in the treatment of neuralgia. To implement it, extensive access to the cranial cavity is required, so trepanation is performed and burr holes are applied. At the moment, the operation is performed extremely rarely.
- Dissection of the bundles that lead to the sensory nucleus in the medulla oblongata. The operation is performed if the pain is localized in the projection of the Zelder zones or distributed according to the nuclear type.
- Decompression of the Gasserian node (Janetta operation). The operation is prescribed when a nerve is compressed by a vessel. The doctor separates the vessel and the ganglion, isolating it with a muscle flap or synthetic sponge. Such an intervention relieves the patient of pain for a short period of time, without depriving him of sensitivity or destroying nerve structures.
It must be remembered that most operations for neuralgia deprive the affected side of the face of sensitivity. This causes inconvenience in the future: you can bite your cheek and not feel pain from injury or damage to the tooth. Patients who have undergone such surgery are advised to visit the dentist regularly.
Dental restoration in the presence of neuralgia
Neuralgia of the facial or cranial nerve is a curable disease in 70% of cases. However, it can recur. In addition, the patient needs very long-term treatment to recover: he needs to do gymnastics, talk as much as possible, inflate balloons, etc. In addition, impaired facial expression can also affect chewing, which may be difficult. That is why, in the case of missing teeth, very high demands are placed on the prosthesis: it must be comfortable, it must not fall out of the mouth, so that the patient cannot choke on it.
In the acute stage of neuralgia, it is worth postponing dental restoration. After at least 2-3 weeks, if the treatment has given positive results, you can contact your dentist with a question about prosthetics.
Removable prosthetics are not recommended, since the structures are quite massive, causing discomfort and long-term addiction. In addition, they do not have good fixation. Therefore, the best option would be to use implantation. However, not classical, but one-stage - it involves the use of modern technologies for 3D visualization of the treatment process, as well as simpler and less traumatic installation of implants.
We remind you that the most important thing when dental implantation is a professional doctor who conducts a thorough diagnosis of the condition of the patient’s jaw system, knows its anatomical structure and uses progressive methods for planning and installing implants that minimize the risks of complications.
1 According to research conducted at the Department of Surgical Dentistry of Odessa State Medical University. N.I. Pirogov.
Diagnosis for toothache
First, the dentist will conduct a visual examination of your mouth. Usually, to identify caries, if it does not develop on the tooth root or under the gum, the doctor simply needs to examine the diseased tooth. In some cases, he uses special indicators that color the areas of enamel affected by the carious process blue or purple. The doctor may also prescribe radiography, laser diagnostics, electroodontometry and transillumination. If dental pathologies are excluded, you will need to go to other specialists - an otolaryngologist, a surgeon, a neurologist or a therapist.