Macroglossia is an enlargement and thickening of the tongue that occurs as a result of a pathological process or as a developmental anomaly. It can develop evenly (diffuse enlargement of the tongue) or partially involving the root, back or lateral surfaces of the tongue. The tongue does not fit in the mouth, protrudes outward, teeth imprints are detected on it, and speech impairment occurs. In the classification criteria, macroglossia is distinguished between true (congenital and acquired) and relative (with micrognathia) [1, 2]. Congenital macroglossia is more common in childhood and is the result of hypertrophy of the tongue and vascular developmental anomalies (Beckwith-Wiederman syndrome, neurofibromatosis type I, Starge-Weher hemangiomatosis, congenital lymphangioma). Macroglossia associated with hereditary metabolic disorders is observed in hypothyroidism, Huller syndrome, Sanfilippo syndrome [3]. Acquired macroglossia is most often associated with amyloidosis, a group of diseases characterized by the deposition of specific interstitial insoluble fibrils in organs and tissues, leading to severe functional impairment and death [4, 5]. Various tumors of the oral cavity (squamous cell carcinoma, verrucous carcinoma, lymphoepithelial carcinoma, squamous interepithelial neoplasia) can cause macroglossia. It develops extremely rarely with syphilis and tuberculosis [6].
Enlargement of the submandibular salivary glands (MSGs) is observed in a number of rheumatic (autoimmune sialadenitis in Sjogren's disease and syndrome, IgG4-related sialadenitis, ANCA-associated vasculitis, etc.), dental (viral/bacterial sialadenitis, sialosis, etc.) and oncohematological diseases (B- and T-cell lymphomas with damage to the salivary glands, plasmatic dyscrasias, etc.) [7, 8].
AL amyloidosis is a systemic oncohematological disease related to plasmatic dyscrasias. It is characterized by the deposition in various organs and tissues of a protein formed from the variable part of monoclonal light chains of immunoglobulins as a result of clonal plasma cell proliferative disorders. It is known that 15% of patients with AL amyloidosis have a unique symptom complex associated with a massive increase in the frequency of heart function, the development of diffuse macroglossia with tongue biting and a change in voice timbre. Periorbital edema, carpal tunnel syndrome, purpura, and muscle hypertrophy develop in 40% of patients with AL amyloidosis [9]. The average life expectancy of patients with AL amyloidosis ranges from 1-1.5 years after diagnosis, while when the heart is involved in the process, it is only 5 months. Dental manifestations of the disease may long precede the development of severe functional disorders of the heart, gastrointestinal tract and kidneys [10, 11]. Therefore, knowledge of soft tissue lesions in AL amyloidosis can significantly improve early diagnosis and significantly increase survival of patients with this severe systemic disease. Our observation can serve as an example of late diagnosis of soft tissue lesions in AL amyloidosis.
Patient A
., 61 years old, October 10, 2014, was admitted with complaints of a dense tumor-like formation in the submandibular region, enlarged tongue and periodic biting of the tongue, difficulty swallowing when eating, hoarseness of voice, numbness of the fingers and limitation of movements in the hands and right shoulder joint , hemorrhagic rashes on the skin of the neck (Fig. 1).
Rice.
1. Macroglossia, increased PFS and diapedetic hemorrhages on the skin of the neck (a) and in the supraclavicular area (b) in a patient with AL amyloidosis. The patient has been aware of herself since March 2013, when she noticed the appearance of tumor-like formations in the area of the prostate gland, which gradually increased in size and merged into a single conglomerate. She was examined at her place of residence. According to ultrasound examination (ultrasound), exacerbation of chronic parenchymal sialadenitis was diagnosed. Standard therapy for acute sialadenitis was carried out: antibacterial and anti-inflammatory drugs. Cytological examination of the thyroid gland did not reveal tumor growth. The tumor formation continued to increase further, numbness in the fingers and difficulty clenching the hand into a fist appeared. In March 2014, due to the ineffectiveness of therapy, a biopsy of the prostate gland and magnetic resonance imaging (MRI) were performed. Hyperplasia in chronic sialadenitis was diagnosed. According to the studies conducted, Mikulicz's disease (damage to the parathyroid gland and sublingual salivary glands) was diagnosed and the patient was referred for consultation to an oncologist to resolve the issue of radiation therapy. Radiation therapy was performed with a total radiation dose of 46 Gy. Despite the therapy, the disease progressed, the tongue significantly increased in volume, the dryness of the mouth increased, swallowing of food was impaired, and movement in the hands and shoulder joint became limited. In October 2014, an MRI examination of the head was performed with a puncture biopsy of the tongue; the diagnosis of a tongue tumor was excluded. A patient with a diagnosis of sialadenitis of the parathyroid gland was sent for consultation to the Research Institute of Rheumatology named after. V.A. Nasonova and was hospitalized with a diagnosis of AL-amyloidosis with soft tissue damage (increased PFS, macroglossia, carpal tunnel syndrome, tendon flexion contractures of the hands, diapedetic petechial skin rashes). On admission: condition of moderate severity, asthenic physique (weight loss per year 25 kg). Flexion contracture of the right hand (Fig. 2), tunnel syndromes on both sides in the wrist and elbow joint, limitation of movements in the right shoulder joint.
Rice. 2. Flexion contracture of the right hand of a patient with AL amyloidosis.
Examination of the dentist: skin: multiple petechiae in the supraclavicular areas and along the anterior surface of the neck. Facial skin color is not changed.
The configuration of the face is changed due to the massive formation of stony density in the submandibular region (20×8 cm) (see Fig. 1). The parotid glands are not palpable. Regional lymph nodes are not palpable. Movement in the temporomandibular joint is free.
The mucous membrane of the oral cavity is almost impossible to examine due to the massive enlargement of the tongue. There is no free saliva. The tongue occupies the entire space between the palate and the floor of the mouth; there are deep imprints of teeth on the lateral surfaces. The tissues of the tongue are stony, the back of the tongue is hyperemic and dry. The patient cannot close her mouth completely. Sleeps half sitting.
In a photograph of the skull in a direct projection, the fan-shaped divergence of the molars and premolars of the upper and lower jaws attracts attention (Fig. 3).
Rice. 3. Multiple destructive foci in the bones of the skull, fan-shaped divergence of teeth in a patient with AL amyloidosis.
Sialometry (stimulated test) was performed - 0 ml of secretion was obtained.
Sialography: there are no signs of parenchymal mumps. The X-ray picture is normal (Fig. 4).
Rice. 4. Sialograms of patient A. Normal variant. a - direct projection; b - lateral projection.
In a biopsy of the minor salivary gland: sialoadenosis with signs of atrophy. Amyloidosis was not detected.
Examination by a rheumatologist: the condition is closer to satisfactory. Asthenic physique. Consciousness is clear. Body temperature is normal. There are flexion contractures of both hands (see Fig. 2), tunnel syndromes on both sides in the wrist and elbow joint. There is no swelling. The cardiovascular and respiratory systems are unremarkable.
Echocardiography revealed diffuse thickening of the myocardium of the “semolina” type. Cardiac amyloidosis is questionable. Ultrasound of the shoulder joints: subluxation of the heads, deformation of the articular surfaces of the shoulder blades on both sides.
Immunological blood test: antinuclear factor was determined at a titer of -1/320 h+sp. An immunochemical study of blood serum and urine confirmed the presence of monoclonal secretion of Bence Jones protein (BJλ).
Considering the absence of AL amyloidosis in the biopsy of the minor salivary gland, the patient underwent a repeat biopsy of the prostate gland and skin. A biopsy of the thyroid gland (Fig. 5) and skin revealed massive deposits of amyloid protein. Based on the results of a myelogram, trephine biopsy of the bone marrow and computed tomography of the skeletal bones (multiple foci of destruction of the skull bones in the thoracic vertebrae, sternum, clavicles, humeral heads and shoulder blades), a combination of two plasmatic dyscrasias was diagnosed: multiple myeloma and AL amyloidosis.
Rice. 5. Amyloid masses (orange-brown) located periductally to the PIJ. Coloring Congo red. ×200.
Thus, by the time of diagnosis, the patient’s clinical manifestations were extensive and almost irreversible. Despite the patient’s repeated visits to various dental institutions and a biopsy of the prostate gland 5 months after the appearance of their enlargement, the diagnosis of the disease was not verified within a year. Therefore, we consider it necessary to familiarize dentists with the algorithm of dental examination for systemic diseases that occur with enlargement of the major salivary glands (MSG), developed at the Research Institute of Rheumatology named after. V.A. Nasonova (see diagram, table).
Anatomical features of the salivary glands
The salivary glands secrete slightly alkaline saliva in the mouth. Saliva is a liquid that is approximately 99% water. These organs secrete between 1000 and 2000 ml of saliva every day. It contains mainly two types of substances that are secreted by the salivary glands. The first substance is mucus, a combination of mucin and water, which is a highly viscous substance used to lubricate food particles and maintain oral hygiene. The second is a serous fluid containing the enzymes amylase, ptyalin, maltase, peptidase, and proteinase. For example, amylase is a substance that begins the digestion process by breaking down starch into oligosaccharides.
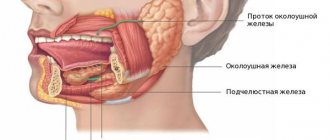
There are three pairs of major salivary glands - parotid, submandibular and sublingual. Three ducts depart from them, respectively, which open into the oral cavity. Also on the mucous membrane of the oral cavity are the buccal, lingual, palatine, labial, and molar minor salivary glands.
Parotid gland
This is the largest pair, each of which consists of a superficial and a deep part. It produces saliva containing large amounts of protein. The parotid glands lie in front and are somewhat inferior to the ear. The deep part of the parotid gland extends to the neck below the angle of the mandible. A dense connective tissue capsule covers this organ, the parenchyma of which has a lobulated alveolar structure. These alveoli consist of secretory cells. The parotid duct, also called Stensen's duct, is 5 to 7 cm in length. It runs across and to the anterior edge of the muscle, where it rotates medially to open into the mouth opposite the upper second molar tooth.
Submandibular gland
The submandibular glands lie medial to the mandible, with each gland also consisting of a superficial and a deep part. The superficial part is inferior and is located in front of the angle of the mandible, and its posterior part lies next to the apex of the parotid gland. A small, deep part of the gland flows around the posterior border of the mylohyoid muscle. From this deep part arises the submandibular canal, also called Wharton's duct. It averages approximately 5 cm in length, running anterior and medial to the mandible and opening laterally near the frenulum of the tongue. The organ has a complex mixed alveolar-tubular structure, the second largest.
Sublingual gland
It is the smallest of the three pairs of salivary glands. It is also alveolar-tubular, but the difference is that it is of the mucous type. The organ is located under the mucous membrane of the mouth and forms a longitudinal ridge on both sides of the base of the tongue, the sublingual fold. From each of them large sublingual ducts depart, which can open into the submandibular canal. There are also approximately 12 small sublingual ducts, the ducts of Rivinus, running from the superior border of the gland to open at the sublingual fold.
What are salivary glands and their purpose?
The organ is responsible for the formation of saliva. Essentially, these are small canals in the oral cavity. The largest are the parotid, submandibular and sublingual, in addition to these there are also small ones. When an infection enters the mouth, the infection process often spreads to this organ, leading to inevitable inflammation. In addition, there may be cases of congenital pathology of their structure, which can also be detected by ultrasound . Price
surveys are quite accessible to all segments of the population.
Depending on the purpose of the diagnosis, ultrasound can be performed separately for the salivary glands, or it can be performed in a single complex.
Doctors prescribe this procedure in the following cases:
- Diagnosis of cancer;
- Differential examination, including analysis of inflammation and tumors;
- Identification of the disease, as well as determination of organ obstruction;
- Suspicion of a cyst;
- Suspicion of stones in the gland.
In the case when a person has been suffering from pain in the ears, tonsils or mouth for a long time, and this pain is reflected by pain in the temples and back of the head, swelling of the neck and cheekbones, and an increase in temperature, it is necessary to consult a doctor and be sure to visit an uzist. Prices, as already mentioned, are affordable, and we have one thing for health.
You can make an appointment for ultrasound diagnostics with our consultants by phone
Prices for ultrasound Clinic addresses Ultrasound at home Acetone in urine Consultation with a surgeon Call a doctor to your home
Indications for sialography
Sialography is used to demonstrate the relationship of the salivary glands to their adjacent structures. It provides diagnostic, including preoperative information in cases of salivary gland pathology. This study is indicated for:
- persistent inflammatory diseases of the glands (mumps);
- the presence of stones (sialoliths) in the excretory ducts;
- siaexatia - dilation of the ducts;
- fistulas and tumor neoplasms;
- determination of cysts of varying severity and duct obstruction.
Patients will complain of weakness, swelling of the jaw in the parotid area, pain and discomfort in the face and mouth.
Treatment in Japan
Russian Medical Server / Treatment in Japan / Endoscopy of the parotid salivary glands in Japan
Endoscopy of the parotid salivary glands is used for the diagnosis and treatment of inflammatory processes of the salivary glands and salivary stone disease. According to statistics, 10% of stones are formed in the parotid glands.
Not all stones are visible on x-rays, so ultrasound, endoscopic examination methods and computed tomography are used for diagnosis. Endoscopy of the parotid glands allows the surgeon to identify the patient's problem and treat it during the examination.
The central channel of the endoscope contains instruments that allow you to remove foreign bodies and stones, expand the lumen of the gland duct in case of stenosis, administer medications, perform intraductal focal laser treatment on the salivary glands and balloon plasty.
Using endoscopic technology at the present stage, Japanese clinics successfully diagnose and treat the following pathologies:
- parenchymal and interstitial sialadenitis;
- salivary stone disease (sialolithiasis);
- obstructive lesions of the salivary glands (strictures, polyps);
- sialoses (endocrine, autoimmune, neurogenic);
- Sjögren's syndrome.
According to statistics, about 10% of stones are formed in the salivary glands, and up to 50% of stones are not visualized on x-rays. The problem of sialolithiasis is relevant for 1.2% of people.
Endoscopy of the salivary glands in diagnosis
Sialendoscopy of the parotid salivary glands using flexible microendoscopes with a diameter of 0.9 to 1.3 mm makes it possible to visualize the extraglandular section of the excretory duct of the salivary gland. In addition, the examination area includes most areas of the intraglandular ductal system, up to the ducts of the 2nd-3rd, and in some cases, the 4th-5th orders.
Endoscopy of the salivary glands with sialolithiasis makes it possible to establish the cause of their obstruction by detecting fixed and migrating stones and mucus plugs.
When diagnosing mumps, endoscopic examination reveals pathological changes in the ducts, their uneven expansion, or, conversely, swelling and narrowing, parietal mucous plugs and plaques.
This diagnostic method has replaced radiography (sialography), ultrasound examination (in the case of X-ray negative stones) and computed tomography, favorably differing in the possibility of carrying out therapeutic manipulations.
Endoscopy of the salivary glands in treatment
During endoscopy, directly conducting an examination, the surgeon can simultaneously perform the necessary therapeutic interventions, since in the second working channel of the tube the endoscope contains a number of necessary tools: tweezers, micro drill, laser, forceps, balloons for dilating the ducts. With their help, you can remove or fragment stones (foreign bodies), bougienage, intraductal local laser treatment, balloon plasty, administer medications, and wash the gland ducts.
In the case of sialolithiasis, after determining the size and position of the stone in the duct, Japanese surgeons use one of the methods for removing it: in a single block using a wire basket grip (forceps) or destroying the stone into fragments with their subsequent removal. If the first two methods are unsuccessful, dissection of the duct above the stone and removal of the stone under endoscopic control are used.
Endoscopic treatment is also successfully used in Japan for inflammatory diseases of the salivary glands (sialoadenitis). In this case, the therapeutic effect is due to an improvement in the passage of saliva in the presence of an inflammatory process, which creates favorable conditions for eliminating congestion in the gland, and already on the second day after the procedure, the size of the gland returns to normal.
Endoscopy of the parotid salivary glands is performed under general or local anesthesia, depending on the clinical situation. The operation lasts no more than an hour. The duration of postoperative hospitalization does not exceed 1 day.
Benefits of salivary gland endoscopy in Japan
It should be noted that the introduction of gentle endoscopy techniques into medical practice has completely changed the tactics of treating sialolithiasis, since previously the operation was accompanied by complete removal of the salivary glands. Nowadays salivary stones are removed without additional skin incisions through natural means. In addition, the latest techniques have made it possible to avoid the use of extracorporeal shock wave lithotripsy, which was often used for sialolithiasis, thereby avoiding unwanted risks.
Manipulations during endoscopy of the salivary glands are absolutely safe, minimally traumatic and practically bloodless, characterized by the absence of the risk of damage to nerves, blood vessels and other anatomical formations.
Endoscopy of the salivary glands is a minimally invasive, simple and highly informative diagnostic and treatment procedure. The possibility of simultaneous surgical intervention on the duct system makes sialoendoscopy the method of choice in the diagnosis and treatment of sialolithiasis and chronic inflammatory pathology of the salivary glands.
Japanese otolaryngologists have an excellent command of the sialoendoscopy technique, which ensures high speed, accuracy and efficiency in diagnosing and treating diseases of the salivary glands.
+7 (925) 50 254 50 – Treatment in Japan
REQUEST TO THE CLINIC
Selection of contrast agent for sialography
Contrast agents are divided into two groups: fat-soluble and water-soluble agents. Water-soluble contrast agents can fill the thinner elements of the flow system. Fat-soluble ones are viscous and can cause allergic reactions, causing discomfort in patients.
They also fill not the thin elements of the channels, but the larger ones.
The contrast used for sialography was originally developed for other medical applications. Therefore, scientists came to the conclusion to investigate the properties of these substances for use in sialography. 11 radiopaque substances were selected and their properties for sialography were studied. An in vitro study was conducted to determine their contrast qualities and the extent of their evacuation after sialography. In animal experiments, their possible harmful effects on salivary gland tissue were studied. In addition, the effects of radiopaque contrast material on extragranular tissues were examined, which are important for determining the consequences after contrast is administered to these tissues. The results of this study were compared with data from the literature. Conray 80, Amipaque 440, Lipiodol UF, Myodil and Duroliopaque appear to be the most suitable media for sialography.
Sialography technique
No special preparation is required before this procedure. The patient can continue to take their medications, drink and eat before the test. But if a person has dentures, the doctor will ask you to remove them before the procedure. They will also be sure to ask whether the patient is allergic to the contrast agent or iodine, and whether there is a possibility that the patient may be pregnant.
To perform sialography, a contrast agent is injected into the ducts of the salivary glands. First, the contrast is heated to 40 degrees Celsius, so as not to cause convulsive syndrome. The substance is administered using a syringe. Based on gender, age and type of gland, the required amount of contrast is determined. To diagnose the submandibular gland, approximately 1.5 ml of contrast agent is needed, for the parotid gland - 2.5 ml. Then the ducts are washed with isotonic sodium chloride solution, a catheter already filled with contrast is taken and advanced into the duct to approximately three centimeters. It is fixed on the skin of the cheek.
A series of radiographs are then taken to determine the distribution of fluid and the level of filling of the duct, to identify any obstructions and their location, and the rate of fluid release from the gland. Photographs are taken in straight, profile, tangential and axial views. It is by them that the normal functional activity of the salivary organs is determined. To stimulate saliva production, use citric acid. The excretory function of the glands is assessed every half hour for two to three hours. X-rays are taken in at least two projections. If a more detailed study is necessary, panoramic tomography is performed.
Types of sialography
This study should be carried out not during the period of exacerbation of the disease, but during the period of remission. Indeed, during acute processes, a worsening of the inflammation of the salivary glands – sialadenitis – can be observed.
There are several types of examination of the salivary glands - pantomosialography, digital sialography, sialadenolymphography, computed sialotomography, sialosonography, thermosialography. Sialotomography, electroroentgenosialography, pneumosubmandibulography, stereoradiography and many other types of examinations are used very rarely today, except in scientific research.
Pantomosialography
This examination includes simultaneous contrasting of both parotid or submandibular glands, or all four glands are examined simultaneously. Afterwards, a panoramic tomography is performed - an orthopantomogram - an image of both jaws to identify pathologies of all teeth, bone tissue, and paranasal sinuses. The study is carried out for the same indications as conventional sialography. The advantage is that with simultaneous examination of paired glands, the chances of detecting inflammatory processes in the paired organs being examined increase without the presence of an obvious clinic. During diagnosis, the doctor will be able to identify uniform or uneven narrowing and expansion of the duct, their displacement or intermittency, determine whether the contours are clear and whether there are various defects in the filling of the ducts.
Sialadenolymphography
The procedure for diagnosing pathologies of the salivary glands by determining the functioning of their lymphatic system. Scientists have proven that an unevenly depleted pattern of lymphatic vessels inside organs, with preserved organ contours and regional lymph drainages, indicates the possible presence of chronic sialadenitis in the patient. And filling defects are observed in tumor formations. The manipulation takes place in such a way that a medical worker subcutaneously injects two milliliters of fat-soluble contrast or four milliliters of a water-soluble substance into the parotid gland with a syringe needle. After five and twenty minutes, and then after two hours and a day, a series of photographs is taken.
Digital sialography
This is an examination of the salivary organs, which is carried out using an X-ray machine with digital material. The examination time is usually less than one minute. It allows you to study a more detailed contrast image at the time of filling and release of the contrast agent, as well as the state of all tissue and bone formations.
Sialosonography
This is what ultrasound examination of the salivary glands is called. Only it helps to establish the macrostructure of the organ under study. The echogram determines the size, shape, ratio of tissue layers at different densities, sclerotic changes, the presence of salivary stones and tumors.
Thermosialography
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
This method helps to monitor the dynamics of changes in the temperature of the organs being studied. For this, a thermal imager is used, the kinescope of which creates a thermal cartogram of the temperature of a person’s neck and face. As is known, there are three types of facial temperature patterns: cold, intermediate and hot faces. Each type is purely individual and, as a rule, does not change throughout life.
Malignant neoplasms and inflammation in the salivary glands lead to an increase in the temperature of the facial skin, especially in comparison with the healthy side. This diagnostic method allows you to simply, harmlessly and without contraindications detect hidden inflammatory pathologies in the glands.
Discussion
The diagnosis of AL amyloidosis is challenging for physicians around the world due to the variety of clinical manifestations and vague symptoms [9, 11–13]. A significant increase in PVS occurs in autoimmune, granulomatous, lymphoproliferative and IgG4-related diseases (see table), but the development of macroglossia in combination with a massive increase in PV is highly specific, suggesting the presence of AL amyloidosis [10, 14]. A biopsy of the prostate gland was performed on the patient 5 months after the onset of clinical manifestations, but the lack of Congo red staining of the biopsy specimen did not allow diagnosing the deposition of amyloid masses in the salivary gland. A biopsy of the affected organs (heart, kidneys, liver, lungs, parathyroid gland, etc.), for histological verification of AL amyloidosis, is performed in the absence of a positive result in alternative sites (minor salivary glands, gums, subcutaneous fat aspirate, rectum) [9, 10, 14]. In our case, a biopsy of the minor salivary gland and gum gave a negative result, but a biopsy of the prostate gland and skin confirmed the presence of AL amyloidosis.
Symptoms of damage to the salivary glands in systemic diseases occurring with an increase in BSG Note. LPD - lymphoproliferative diseases; PP - parenchymal parotitis; CS - chronic sialadenitis; focus >1—focus of lymphoid infiltration of more than 50 cells; LHI—lymphohistiocytic infiltrate; LEP—lymphoepithelial lesion; MSG - minor salivary glands; BSG - large salivary glands.
Scheme. Algorithm for examining patients with enlarged major salivary glands during a dental appointment. MSG - minor salivary glands; BSG - large salivary glands. Note. LPD - lymphoproliferative disease; IHC - immunohistochemical staining of tissues.
It should be noted that immunochemical testing of blood serum and urine should be performed before biopsy. The presence of low levels of monoclonal secretion or light chains of monoclonal Ig in serum or urine is mandatory for AL amyloidosis [9–14], while the absence of these signs suggests manifestations of secondary AA amyloidosis [5]. Considering the variety of diagnoses that were made to the patient during the year, we should focus on the algorithm for examining a patient who came to the dental clinic with enlarged salivary glands (see diagram). Infectious parotitis, salivary stone disease and solid tumors of the salivary glands are well covered in textbooks on surgical dentistry, while diseases with systemic involvement of the major salivary glands receive little attention. The picture of chronic sialadenitis can be present in biopsy samples of the salivary glands in all systemic diseases (see table). Its severity depends on the duration and activity of the pathological process, and without additional research methods it does not allow diagnosing the pathology of the salivary glands. An important diagnostic method is sialographic examination. Parenchymal sialadenitis is a radiological sign. Its presence is a diagnostic sign of Sjogren's disease and primary MALT lymphomas of the major salivary glands [7]. The patient was diagnosed with parenchymal sialadenitis without a sialographic examination. Functional diagnostic methods and MRI can be used to determine the degree of enlargement of the salivary glands and intraglandular lymph nodes, to partially exclude the presence of salivary stones and solid tumors and, in some cases, to suggest the presence of parenchymal parotitis based on multiple cystic changes in them. These methods cannot make a diagnosis, which requires morphological verification. According to the modern classification, Mikulicz's disease is classified as a group of IgG4-associated lesions. Determination of the levels of the IgG4 subclass of IgG in the serum and immunohistochemical examination of the biopsy specimen to determine the synthesis of IgG4 by more than 40% of plasma cells is necessary to make a diagnosis of IgG4-related sialadenitis [6, 7].
The use of radiation therapy for systemic diseases involving the salivary glands (Sjögren's disease/syndrome), granulomatous and IgG4-related sialadenitis, etc.) is a serious mistake, as it increases the manifestations of xerostomia and stimulates the development of lymphomas in these diseases [15] . Using an algorithm for examining patients with systemic lesions of the salivary glands, developed during the examination of 298 patients with a significant increase in the major salivary glands at the Research Institute of Rheumatology named after. V.A. Nasonova, can reduce diagnostic errors in dental practice when conducting differential diagnostics.