Salivary gland stone removal is a procedure indicated for the formation of large stones in the salivary gland. The formation of stones in the salivary gland is a relatively rare occurrence, which, however, can have serious consequences. In the early stages, it is possible to remove the stone from the gland duct on your own. If the resulting stone has become large enough to block it and interfere with the normal outflow of saliva, surgical intervention may be indicated. Sialoscopy The most popular and modern method of surgical removal is sialoscopy. This type of operation is relatively new and became available only with the advent of the latest technologies in the field of medicine. This is due to the fact that the salivary glands are quite complex in structure, and the diameter of their openings does not exceed 0.5 mm.
A modern endoscope is a thin device with miniature systems with a diameter of 0.8 millimeters and a set of even thinner instruments for performing complex medical procedures. Using an endoscope avoids dissecting the salivary gland (previously this was the only way to detect and remove tartar). Using an endoscope, the doctor can see what is happening inside the salivary gland and remove the salivary stone from it with the finest instruments.
Causes
The occurrence and growth of stones in the salivary glands is most often a consequence of a disturbance in the body's calcium metabolism, accompanied by a lack of retinol.
This situation often occurs in people suffering from the following diseases:
- diabetes;
- diseases of the genitourinary system;
- excess vitamin D in the body;
- pathology of the functioning of the endocrine system – hyperparathyroidism.
In addition, experts note that there are some prerequisites for the accumulation of mineral or organic formations in the glands.
The main ones are considered to be:
- mechanical damage to the ducts due to incorrectly selected dentures or sharp edges of teeth and crowns;
- the occurrence of crystallization or stagnation of saliva secretion due to a slowdown in its separation;
- the presence of inflammation in the oral cavity , which causes compression of the salivary ducts and accumulation of pathogenic microflora;
- the development of an inflammatory process as a result of the penetration of foreign particles into the ducts , around which bacteria accumulate and multiply.
Various age groups of the population are susceptible to salivary stone disease, however, the disease is most often diagnosed in men and women aged 25-45 years who abused smoking or took certain groups of medications.
Chemical composition
Stone formation begins around the core, which may be an accumulation of pathogenic microorganisms or have a non-microbial structure.
It is often based on epithelial cells and foreign particles - toothbrush villi, small non-decomposing particles of food products.
The process often occurs against the background of changes in the qualitative composition of saliva, a decrease in the rate of its separation, changes in the amount of mineral salts and acidity.
Stones that form in the tissues or ducts of the salivary glands are composed of organic and mineral components . The elements of organic structure include mucoproteins and amino acids.
The stones contain about 15-25% of these substances. The remaining 75-85% are minerals such as sodium, potassium, calcium, iron, and phosphates.
Reasons for performing sequestrectomy for osteomyelitis and preliminary diagnostic measures.
This material contains detailed information about osteosynthesis of the lower jaw.
Here https://zubovv.ru/hirurgiya/operatsii/udalenie-kapyushona-mudrosti.html we’ll talk about the price of wisdom tooth hood removal.
Destruction of large stones
Large stones cannot be removed endscopically, since the stone simply will not pass through the narrow duct of the salivary gland. It is also not recommended to crush them with a laser. Therefore, if the stone is larger than 3-4 mm, it is removed through a small incision at the bottom of the mouth. Then the excretory duct of the salivary gland is reconstructed and a small silicone drain is installed. Typically, such endoscopic operations are performed under general intubation anesthesia.
Despite the fact that the described technique is an invasive intervention, when the manipulation is performed by an experienced doctor, an excellent result is noted. However, it is better not to start the pathology and, if there are stones of any diameter, remove them as soon as possible.
Symptoms
The initial stage is asymptomatic, so the development of the disease can only be detected through instrumental examination - taking an x-ray.
The appearance of signs of pathology development is often observed when the stone reaches a large size and blocks the lumen of the excretory canal.
The patient experiences the following symptoms of sialolithiasis:
- increased dryness in the mouth due to the production of insufficient saliva;
- replacement of saliva with mucous contents with a purulent admixture;
- swelling of the facial and cervical area due to fluid accumulation;
- pain when opening the mouth , chewing food and swallowing, which can radiate to the ear;
- feeling of fullness in the problem area , swelling in the lower jaw and neck;
- redness of the skin of the face and neck in the area of stone formation.
When a mineral formation reaches a large size, a person can determine its location during an external examination or palpate it.
At an advanced stage of development of the disease, a person experiences general signs of intoxication of the body - a slight increase in temperature, lethargy .
A severe form of the disease can lead to the formation of a through hole in the wall of the salivary gland, through which the stone exits into the soft tissue.
Performing surgery to remove the salivary gland
With the traditional method of surgery, the patient assumes a lying position with his head thrown back and to the side. The operation involves local infiltration anesthesia. Several parallel incisions are made in the submandibular area, the tissue is lifted, and the capsule of the salivary gland is discovered, which is opened, and the gland tissue is extremely carefully removed and removed. When a malignant tumor grows together with nearby tissues, the latter are also removed. After this, stitches are applied.
During endoscopic surgery, both local and general anesthesia can be used. Through small punctures in the tissue, manipulators and a video probe are inserted, which projects all the actions performed on the screen. When the manipulators reach the gland, small incisions are made with their help, through which pathological tissue is removed. The endoscopes are then removed and sutures are placed at the puncture sites.
Postoperative care of the surgical site includes:
- hygiene - no water or dirt should get into the wounds;
- special diet - the diet will consist of semi-liquid warm food, no hot or cold drinks, no alcohol;
- smoking ban;
- special treatment - it is recommended to regularly treat the seams with antiseptics, and the oral cavity after each meal should be rinsed with a mixture of antiseptic and water.
If all the recommendations of the attending physician are followed, complete wound healing occurs within a few months.
Diagnostics
To diagnose salivary stone disease, specialists use a combination of various examination methods:
- with the help of external examination and palpation, an increase in the size of the gland is detected compared to the norm, an increase in the density of its consistency is detected, and pain when pressed is determined;
- instrumental diagnostic methods, in particular radiography, contrast study of saliva, ultrasound, make it possible to confirm the presence of a mineral formation and determine its size and position in the parenchyma of the gland;
- Sialometry is the optimal way to determine the secretory function of the salivary glands .
In addition to the above studies, saliva is often taken from the patient to determine its acidity and qualitative composition.
In combination with other examination methods, this makes it possible to differentiate sialolithiasis from phlegmon, abscess, and neoplasms of the oral cavity.
Treatment
There are various methods for treating salivary stone disease, depending on the degree of its development.
At the initial stages of pathology, specialists often give preference to minimally invasive techniques that facilitate spontaneous stone passage.
At an advanced stage of the pathology, surgery may be required.
Surgical intervention
Today, there are four methods for eliminating stones from the salivary glands:
- Interventional sialendoscopy. The essence of the intervention is that using a thin flexible instrument with a camera at the end - an endoscope.
When introduced into the salivary ducts, the specialist is able to examine them and remove stones. The procedure is minimally invasive and is performed under local anesthesia. - Extracorporeal lithotripsy involves ultrasonic exposure of stones from the outside, as a result of which they are crushed.
This creates the possibility of further endoscopic extraction and washing of the ducts with a special solution, which prevents the development of the inflammatory process. - Dissection of the duct used when the stone reaches a large size and it is impossible to remove it using a minimally invasive method.
In this case, access to the mineral formation can be through the skin or mucous membrane of the oral cavity.Stone removal is performed using a surgical spoon or finger tweezers. Most often, suturing and drainage of the duct wound is not required.
- Extirpation of the salivary gland or the procedure for its removal is the most radical method of treating salivary stone disease.
The operation is used only if it is impossible to eliminate the pathology in another way - with repeated formation of stones or irreversible changes in the parenchyma of the gland. The procedure is performed in a hospital setting under general anesthesia.
What problems are solved with the help of flap surgery in dentistry, and what are the indications for it?
In this publication we will talk about the effectiveness of plastic surgery of the anastomosis with the maxillary sinus.
At this address https://zubovv.ru/hirurgiya/operatsii/udlineniya-i-puti-resheniya.html we will talk about the intricacies of surgical lengthening of the coronal part of the tooth.
Medicines, physiotherapy
A non-invasive technique for eliminating stones from the salivary glands is based on freeing the clogged duct and activating the process of self-removal of the mineral formation.
This treatment option is suitable only when the disease is detected at the initial stage. Conservative treatment of sialolithiasis is based on the following measures:
- Taking medications prescribed by your doctor. Most often, the basis of treatment is anti-inflammatory drugs, medications that enhance saliva secretion, and antibacterial drugs.
- Physiotherapeutic procedures, in particular electrophoresis, fluctuarization, UHF, contribute to the expansion of the salivary ducts and the unhindered passage of stones through them.
- A special diet containing acidic foods and drinks activates saliva production, which also helps remove stones through the ducts.
Professional massage performed by a specialist is another way to remove small mineral formations from the salivary glands. However, the decision on the need for it is made only by the attending physician.
ethnoscience
Non-traditional treatment methods can only be used in conjunction with conservative therapy to remove small mineral formations. According to people's reviews, the following folk recipes are most effective:
- Dry sage leaves are poured with boiling water in the proportion of 400 ml of liquid per 2 tablespoons of the plant, and infused for 1.5-2 hours. Rinse the mouth with the strained solution every 2-3 hours.
- Fresh cranberries are ground to a pasty state, then dissolved in a teaspoon before each meal for 10 minutes. The product helps to increase salivation and remove stones.
- Non-canned birch sap is taken daily, one glass. The liquid helps dissolve calcium-based compounds present in mineral formations.
Remember! The use of traditional methods of treatment is permissible only after consultation with a specialist, in parallel with the implementation of his recommendations.
Sialendoscopy as a method for removing stones from the salivary gland
Chronic obstructive pathologies of the salivary glands can be caused by the presence of salivary stones, the formation of a mucus plug, duct stenosis, the influence of foreign bodies, or anatomical variations in the gland duct system, which can result in retention of saliva in the duct, discomfort, and even infection. Specifically, sialolithiasis is a condition in which a calcified mass forms in the salivary gland. Most often, this disorder is observed in the area of the submandibular gland (in the so-called “Wharton’s duct”) and can cause swelling and pain in the affected area, especially during stimulation of salivation. If the stone does not come out of the gland on its own, it must be removed surgically.
To diagnose such pathologies, methods of radiosialography, ultrasound examination and magnetic resonance sialography can be used. Radiosialography is the most common method for identifying stones in the salivary gland duct, but its use is contraindicated in cases of acute infection or if the patient is hypersensitive to the contrast agent. Ultrasonography is a first-line diagnostic method that allows non-invasively and without the use of contrast to visualize the presence of a calculus in the salivary gland. It should be remembered that the parameters of sensitivity and specificity of this method vary depending on the stage of mineralization of the stone. For diagnostic purposes, of course, you can use more expensive methods such as computed tomography, magnetic resonance imaging or scintigraphy.
Currently, sialoendoscopy is widely used as a non-invasive approach for diagnosing and treating pathologies of the salivary glands. This method allows for direct access to the gland duct, its expansion and irrigation, as well as to establish the presence or absence of patency of the duct.
In this article, we describe the clinical cases of two patients who underwent sialolithotomy procedures using a sialoendoscope at Korea University Anam Hospital. In addition, we will describe the differences between sialoendoscopy and other methods for diagnosing and treating sialolitis.
Clinical case 1
Patient Information
An 81-year-old female patient presented to the dental clinic with a sensation of a foreign body under her tongue and symptoms of dry mouth. She was previously diagnosed with thyroid carcinoma in June 2003 and underwent a total thyroidectomy procedure. The patient's medical history included hypertension and chronic kidney disease. The stone was identified in the duct of the right submandibular gland (Figure 1).
Figure 1. Salivary stones measuring 2 × 10 mm were identified in the right submandibular gland using CBCT.
Surgical procedure
The working area was treated with betadine. After disinfection, the oral cavity was washed generously with saline solution. Local anesthesia was performed in the area of the tongue and floor of the mouth with a 2% lidocaine solution with an epinephrine concentration of 1:100,000. Afterwards, the tongue was sutured with 3-0 silk thread in order to provide optimal conditions for the operation. Using a microscope, the entrance to the duct of the right mandibular gland was found, after which it was entered with probe No. 0000, and then expanded to the size of probe No. 3 (photo 2). In order for the endoscope to penetrate the lumen of the duct, it was expanded using a dilator. The sialoendoscopy procedure was performed under copious irrigation with saline solution. The stone was removed using a three-wire ring (loop) (photo 3). The size of the opening of the duct was smaller than the size of the stone, so the doctor had to make a 0.1 cm incision at the entrance to the gland duct. After removing the stone, we examined the gland with an endoscope to make sure there was patency (photo 4). The glandular system was washed with a steroid solution. No bleeding, swelling or pain was noted in the postoperative period. The patient underwent daily dressings of the intervention area and monitoring for the development of possible wound infection.
Photo 2. a. Gland duct probe. b. Orifice dilator. c. Endoscope monitor. d. Three-portable endoscope. e. Three-wire ring (loop).
Photo 3. a. Stones in the gland duct. b. Removing stones using a loop. c. Capture the stones with a loop and remove them from the duct.
Photo 4. Removal of stones through the mouth of the submandibular salivary gland. b. View of removed stones.
Clinical case 2
Patient Information
A 66-year-old man sought dental attention due to a blocked duct of the right mandibular gland (Figure 5). Approximately 7-8 years ago, he noticed swelling and pain in the lower neck while eating. The sialolithotomy procedure was performed 4-5 years ago in another hospital, but the stones were never completely removed due to their pathological mobility during the operation. The patient had no systemic health problems.
Figure 5. Salivary stones measuring 3 × 4 mm were identified in the right submandibular gland using CBCT.
Surgical procedure
The working area was treated with betadine. After disinfection, the oral cavity was washed generously with saline solution. The patient was given full anesthesia via nasotracheal intubation, and the tongue was sutured with 3-0 silk suture. The intervention protocol was similar to the one we have already described in the first clinical case (photo 6). No bleeding, swelling or pain was noted in the postoperative period. The patient underwent daily dressings of the intervention area and monitoring for the development of possible wound infection.
Photo 6. View of the removed stone.
Discussion
Symptoms of obstructive salivary gland pathologies include recurring, painful swelling of the major salivary glands, which can negatively affect the patient's quality of life. Previously, radiosialography, sonography and MR sialography methods were used to diagnose diseases of the salivary glands. Radiosialography is the main method for examining the salivary glands, which can be used to diagnose sialolithiasis by analyzing images obtained after the injection of contrast into the gland duct. Contraindications to the use of this method are similar patient reactions to the contrast agent and the presence of an acute infectious lesion. Sonography is a non-invasive method for diagnosing stones in the structure of the salivary glands, however, the effectiveness of this approach largely depends on the experience of the doctor conducting the diagnosis. MR sialography allows for complete visualization of the entire salivary gland system, however, the resulting diagnostic images may be characterized by the presence of various types of distortions and artifacts, especially in cases of adjacent localization of dental restorations. However, all of the above-mentioned limitations characteristic of different diagnostic methods can be overcome using the sialoendoscopy method. It is less invasive than other approaches to diagnosing salivary gland pathologies and can be successfully used to assess the condition of their ducts and internal structure.
Several research groups have examined how satisfied patients were with the sialoendoscopy treatment process. Kroll et al, using the short version of the SF-36 questionnaire, found that patients reported a high level of satisfaction after sialoendoscopy. Aubin-Pouliot et al, using a questionnaire designed to assess chronic obstructive sialadenitis, demonstrated similar results. In addition, an interesting fact was established that after sialoendoscopy on the submandibular gland, the symptoms decreased much more pronounced than after a similar manipulation on the parotid salivary gland.
Recent studies have shown that microsialoliths play an important role in the pathogenesis of chronic sialadenitis. They can accumulate in normal salivary glands and provoke the development of obstructive atrophy. The latter, in turn, promotes the colonization and proliferation of microbes, causing inflammation in the peripheral ductal system, accompanied by even more severe atrophy and progressive infection, leading to chronic sialadenitis. According to Quinn et al, intraductal placement of antibiotics facilitates their penetration into the parenchyma of the glands, allowing the existing symptoms of the lesion to be completely eliminated. However, the same results were obtained when irrigating the internal structure of the glands with saline solution.
Radioactive iodine (RAI) therapy is another cause of salivary gland disease. According to Kim, chronic sialadenitis is the most common complication of RAI, especially in cases after thyroidectomy. The prevalence of chronic sialadenitis associated with RAI is 11–65%. Damage to the salivary glands caused by radioactive iodine leads to the development of obstructive sialadenitis and recurrent swelling with or without pain during meals. This chronic condition subsequently causes hyposalivation and associated symptoms, such as difficulty swallowing, taste disturbances, oral candidiasis and caries. Currently, chronic sialadenitis caused by radioactive iodine therapy is treated conservatively by maintaining a good level of oral hygiene, frequent hydration, the use of saliva substitutes, and stimulation of the salivary glands.
According to Kim's study, sialoendoscopy demonstrates similar effects to sialocentesis (intraductal irrigation with sterilized saline) and can improve obstruction symptoms as early as 3 months after mechanical dilatation with an endoscope. However, in patients with chronic sialoadenitis caused by radioactive iodine therapy, sialoendoscopy has been found to have limited ability to relieve existing symptoms of xerostomia.
This article described examples of using the sialoendoscopy method to remove stones from the salivary glands. This method is more effective compared to other approaches to the treatment of sialolithiasis, and at the same time less uncomfortable. In the two clinical cases analyzed, patients did not demonstrate any significant complications or similar effects after performing the manipulation.
Conclusion
This article describes two clinical comparisons of non-invasive sialolithotomy procedures using sialoendoscopy. This approach can be effectively used not only to treat cases of sialolithiasis, but also for ductal stenosis and sialadenitis. At the same time, sialoendoscopy is a minimally uncomfortable procedure, which is characterized by a low level of complications. To formulate any definite recommendations regarding the use of sialoendoscopy in cases of stones in the salivary glands, it is necessary to ensure that studies are carried out with the participation of a larger number of subjects.
Authors: Dong-Keon Lee, Euy-Hyun Kim, Chang-Woo Kim, Mong-Hun Kang, In-Seok Song, Sang-Ho Jun
Relapse and exacerbation
Re-formation of stones in the salivary glands after their removal occurs in 8-10% of cases. As a rule, the situation indicates the persistence of problems with the functioning of the endocrine system and metabolic disorders in the body.
The patient may need to consult with specialized specialists who can identify the existing disease leading to the growth of stones.
Often, a relapse of sialolithiasis entails irreversible changes in the structure of the glands, which sooner or later requires their removal.
Diagnosis of salivary gland stones
Suspected salivary gland stones are characterized by certain symptoms, but various tests are used to assess the shape and number of stones, as well as their location. The density of the mineralized stone is quite high, so it is quite clearly visible on x-rays. In some situations, an x-ray is not an effective diagnostic method due to the fact that a shadow may fall on the stone or the stone is not sufficiently mineralized. For clearer X-ray results, before starting the procedure, a special substance is injected into the duct, which makes it possible to view the structure and shape of the ducts; the places of ruptures are stones in the salivary gland.
In modern medicine, a diagnostic method in the form of computed tomography is used. With such an examination, stones of the salivary glands are determined, the size of which is less than one millimeter; it is also obvious how many stones are and where they are located. The disadvantage of the method is the inability to determine the condition of the soft tissues.
A clearer diagnostic method is magnetic resonance imaging (MRI). It is used to determine the condition of soft tissues, but it is not able to show the number and location of stones.
Ultrasound examination is also used as diagnostics, but this method requires a highly qualified doctor.
The most accurate and clear method that gives a complete picture of the disease is sialoscopy. It involves inserting microscopic endoscopes into the salivary ducts, allowing doctors to see a real picture of the processes occurring inside the body.
Forecast
The experience of specialists shows that in 90% of cases of timely seeking professional help, the prognosis in the treatment of salivary stone disease is favorable, regardless of the chosen treatment method.
However, an important factor in a successful outcome and the absence of re-formation of stones is identifying the cause of the pathology and its elimination.
A visit to a specialist at an advanced stage of sialolithiasis most often ends with an operation to remove the salivary gland. In the future, this can lead to disruption of the oral microflora and problems with teeth and gums.
What are salivary stones?
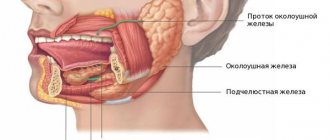
The salivary glands in the mouth produce a fluid called saliva. Saliva protects the teeth, aids in chewing and swallowing food, and initiates the digestion process. The mouth contains hundreds of minor salivary glands and three pairs of major salivary glands. This:
- parotid glands, which are located below the ears on the inside of the cheeks;
- submandibular glands on the floor of the mouth near the jaw line;
- sublingual glands, which are located under the tongue.
Saliva stones contain calcium and other minerals. According to statistics, stones can form in the ducts of any type of salivary glands. Larger stones can block the flow of saliva and cause the glands to swell. More than 80% of salivary stones form in the submandibular gland, while 6-15% occur in the parotid gland and 2% in the sublingual and minor salivary glands.
Prevention
Preventing the development of pathology is much easier than eliminating its consequences, so dentists recommend adhering to the following rules:
- eat fully and balanced;
- drink purified drinking water;
- monitor oral hygiene;
- if there is a high amount of calcium in the body, avoid excessive consumption of foods rich in this element;
- give up bad habits such as drinking alcohol and smoking;
- undergo regular dental examinations.
The video contains additional information on the topic of the article.
Reviews
The formation of stones in the salivary gland is a rather rare disease, but if it is not diagnosed in a timely manner and the initiation of therapeutic procedures, it can lead to serious consequences.
For this reason, dentists strongly recommend not to neglect regular preventive examinations, and not to self-medicate if any painful sensations occur.
If you have had to deal with the need to remove a mineral formation that has formed in the salivary gland, share with your readers the features of the operation and recovery period in the comments section.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags salivary gland stone removal surgery
Did you like the article? stay tuned