Ameloblastoma
Treatment of ameloblastoma consists of its removal during surgery, which is performed under general anesthesia in the Center’s own hospital, equipped with the most modern dental and operating equipment, as well as comfortable wards.
The Center for Maxillofacial Surgery and Implantology provides treatment of diseases such as benign jaw formations of any degree of complexity at the highest level.
This work requires a particularly attentive individual attitude towards the patient, extensive experience and professionalism, and impeccable mastery of advanced treatment methods, which our specialists fully possess.
What is ameloblastoma
Ameloblastoma is a benign tumor that occurs in most cases in the lower parts of the jaw, and extremely rarely in the upper ones. For a long time it does not appear in any way, and can be detected on an X-ray of the jaw taken for some other reason.
The tumor grows very slowly and remains asymptomatic for a long time. Patients seek medical help due to jaw deformation, tooth mobility or displacement. If the tumor is significant, its further growth can lead to a pathological fracture of the lower jaw.
Clinically, cystic and massive forms of ameloblastoma are distinguished. A characteristic feature of the cystic form is the presence of isolated or partially disconnected cysts. In rare cases, adamantinoma may present as a solitary cystic tumor. The cyst cavity is lined with a thin epithelial membrane. Massive ameloblastoma is represented by spongy tissue with cysts of varying sizes located in it, which are not always determined radiologically. With prolonged growth, microscopic cysts merge into several larger ones or one large one. In contrast to cystic forms, massive ameloblastoma has a spongy substance along with the cavity.
Types of tumor
Ameloblastomas can develop asymptomatically and painlessly over several years and become noticeable only when the lower parts of the jaw are deformed. In the upper parts of the jaw, its formation can proceed completely unnoticed, sometimes manifesting itself in the form of toothache-like pain. Most often on the lower jaw it is located in the area of the angle or branch of the jaw, and over time attracts attention with noticeable asymmetry of the jaw.
In some cases, the tumor may have a multilocular form, which is why it is mistakenly believed that it is malignant. But that's not true. Malignant tumors are distinguished by the fact that they develop by metastasizing into healthy tissues of the body, while benign tumors develop separately and are easily removed surgically.
Ameloblastoma of the mandible
Among ameloblastomas, mandibular tumor localizations are more common. Such formations most often develop asymptomatically or are accompanied by uncharacteristic signs reminiscent of other tumors, so diagnosis must be carried out as accurately as possible.
The tumor grows slowly, gradually manifesting itself as deformation changes in the lower jaw. Ameloblastomas of similar localization account for about 90% of cases of the total number of tumors of this kind.
Tumor of the upper jaw
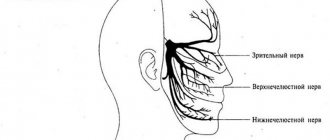
Maxillary tumor localization is rare. When it affects the upper parts of the jaw, patients experience problems with nasal breathing, visual disturbances such as double vision in the eyes, tearing, and impaired skin sensitivity.
Sometimes there is pain in the area of the tumor, reminiscent of toothaches. With the maxillary location of ameloblastoma, defective changes in the jaw usually do not occur.
Tumor symptoms
It develops slowly, so often patients simply do not notice the signs of pathology. But gradually the tumor process begins to acquire specific symptoms associated with jaw deformation:
- Facial asymmetry, which can be slight or pronounced.
- Swelling in the affected area.
- When bone tissue is involved in the tumor process, patients experience a pain symptom, which many perceive as a toothache.
- With maxillary localization, palatal deformation also occurs, and ameloblastoma itself can grow into the orbit and nasal cavity.
- When the tumor process is neglected, fistulas form in the oral cavity, secreting purulent-serous mucus.
If the patient ignores the development of the tumor and delays contacting a specialist, then malignancy of the tumor may occur, which is observed in 4% of cases.
Diagnosis of the disease
To determine the pathology, a thorough diagnosis is necessary, because its symptoms are similar to other tumors.
A qualified diagnostic approach will protect the patient from erroneous treatment.
To identify pathology, radiography is used, which helps determine the shape and size of the tumor, the extent of the spread of pathology and the volume of bone lesions.
Treatment methods
The basis of therapy for ameloblastoma is surgical removal by maxillary resection. Removal is carried out under anesthesia in a hospital setting. The patient is left in the hospital after the operation to exclude possible complications.
The Center for Maxillofacial Surgery and Implantology recommends that if you experience minor pain in the upper jaw or lower jaw, and even if you are completely confident in the absolute health of your teeth, you should definitely seek advice from an experienced specialist. The doctor will prescribe an x-ray of the jaw, an MRI, and, if necessary, a puncture and histological examination.
Treatment for ameloblastoma is only surgical, consisting of jaw resection. Based on the size and location of the tumor, the scope of surgical intervention is determined - resection of the jaw without breaking the continuity, resection of the jaw within healthy tissues with breaking of continuity. When the tumor spreads to the entire jaw, it is disarticulated. To prevent functional disorders, primary plastic surgery of the jaw is performed, and if this is impossible, orthopedic fixing structures are made.
Therapy for ameloblastoma consists of its removal during surgery, which is performed under general anesthesia in the own hospital of the Center for Maxillofacial Surgery and Implantology. It has modern operating rooms equipped with high-precision dental, surgical and anesthesiological equipment, allowing operations of any degree of complexity, as well as comfortable wards for rehabilitation under constant medical supervision. The team of qualified specialists has extensive experience in performing such surgical interventions, and in comfortable rooms under medical supervision it is pleasant to relax and recover.
Recurrent ameloblastoma: a clinical case
Ameloblastoma is a common, localized, aggressive, benign odontogenic tumor of the oral cavity of epithelial origin. This pathology was first described by Cusack in 1827, and its name was given to Ivy and Churchill in 1930.
According to the 2005 WHO classification, there are 4 subtypes of benign ameloblastoma: (1) solid/multycyst, (2) desmoplastic, (3) unicyst, and (4) extraosseous/peripheral. Histologically, 6 tumor subtypes can be differentiated, including follicular, plexiform, acanthomatous, basal, unicyst and desmoplastic. Treatment is carried out either conservatively or radically, depending on the type, location and size of the lesion, as well as taking into account the age of the patient. A systematic review by Almaida and colleagues found that 50% of tumor recurrences are observed in the follicular subtype, and the incidence of such development is reduced when a radical treatment algorithm is implemented. This article describes two cases of recurrent ameloblastoma in patients who underwent segmental resection of the jaw.
Clinical case 1
A 46-year-old patient sought help at a private dental clinic with complaints of swelling in the area of preliminary surgery, covering the area of the lower jaw on the right. According to the medical documentation, it was established that about 15 years ago the patient underwent a segmental resection of the jaw with further augmentation of the formed defect with an augmentation from the region of the ribs. No data on the histopathological characteristics of the lesion were noted in the patient's medical record. After a CT scan and orthopantomography, a multilocular radiolucent lesion was discovered in the area of the previous surgical intervention (photo 1).
Figure 1: 3-dimensional reconstruction of a CT scan demonstrating recurrent tumor in the area of the augmentation involving the articular process.
Clinically, a diagnosis of recurrent multicystic ameloblastoma with involvement of the bone augmentation was made. An incision in the tumor area was made at a distance of 1 mm from the edge of soft tissues unaffected by pathology through the scar contour already existing from the preliminary operation (photo 2-3). The specimen collected for histology allowed a diagnosis of follicular ameloblastoma with acanthomatous changes and free margins. 1 year after surgery there were no signs of relapse. Therefore, alloplastic reconstruction of the mandible on the right side was planned, given the benign nature of the tumor.
Photo 2: View of the exposed tumor during surgery.
Photo 3: Surgical specimen.
Clinical case 2
A 45-year-old patient sought help from the Department of Oral and Maxillofacial Surgery with complaints of swelling in the right temporal region. The swelling did not provoke pain and developed over the course of a month, increasing in size. There were no signs of infection in the affected area. In 2012, the patient already approached a private dental clinic with a similar problem. An orthopantomogram and CT scans revealed a multicystic lesion. After a biopsy, it became clear that the problematic tumor was an ameloblastoma. The patient underwent a hemimandibulectomy procedure. Directly during surgery, radiography of the surgical tumor specimen was taken to analyze the condition of the tissues at a distance of 1.5 cm from the clinically visualized tumor edge. Histological analysis confirmed the diagnosis of ameloblastoma with atypical features and multicellular structure. In 2021, the patient again experienced swelling in the right temporal region. MRI identified heterogeneous signal enhancement in this area measuring 4.4 cm × 3.7 cm × 4.6 cm with the presence of tiny cystic inclusions (Figure 4). Through access along the zygomatic bone, the tumor was removed with a certain amount of surrounding tissue (photo 5-6). The formed defect was restored using the temporal muscle. After histoanalysis of the surgical tissue sample, the diagnosis of ameloblastoma with non-invasive margins was confirmed. At this time, the patient is at the monitoring stage.
Photo 4: Preoperative CT scan showing recurrent ameloblastoma in the infratemporal fossa.
Photo 5: Visualization of the bone defect after tumor removal, which was then reconstructed using the temporalis muscle.
Photo 6: Excised tissue sample.
Discussion
Ameloblastoma is a locally aggressive tumor of the oral cavity that rarely undergoes malignant transformation. After odontoma, it is the second most common odontogenic tumor. According to epidemiological data, 70% of cases of ameloblastoma were reported in developed countries. The problem of low identification of ameloblastoma in developing countries is obviously associated with the insufficient level of their official registration. The WHO classified ameloblastoma into four subtypes in 2005: multicystic/solid, unicyst, desmoplastic, and extraosseous. Solid/multycystic ameloblastoma is the most common type, which is also the most aggressive and often recurs after conservative treatment such as curettage or enucleation. Ameloblastomas of the lower jaw recur much more often than their counterparts in the upper jaw. Also, the follicular type of tumor is characterized by a higher rate of relapse compared to its plexiform subtype. The pathogenesis of ameloblastoma development remains incompletely understood. The genetic theory of development involves the participation in the process of pathogenesis of the BRAF protein in the structure of the mitogen-activated protein kinase pathway (MAPK), which, as a rule, is already identified as mutated.
Ahlem et al found that the activity of the biomarkers Ki67 and CD10 was significantly higher in recurrent tumor types compared to primary tumor types. As a rule, ameloblastoma affects the posterior areas of the lower jaw. Infiltration of the lesion occurs into the cancellous part of the bone with less involvement of the cortical component. The CT scanning method for diagnosing a tumor is the most informative when the cortical structure of the bone is damaged and the damage has spread to the surrounding soft tissue. Treatment of the tumor can be conservative or radical. A conservative approach involves enucleation of the tumor with further chemical cauterization or peripheral osteoectomy with expansion of the excision boundaries by 1-1.5 cm from the visualized edge of the tumor. A conservative treatment approach is more effective in cases of monocystic type of formation. According to Pogrel and Montes, unicystic ameloblastomas respond best to conservative treatment using Carnoy or cryotherapy principles. A radical approach is indicated in cases of large ameloblastomas when the lesion has spread to the area of the inferior alveolar nerve, or in cases of the aggressive nature of the tumor. The radical treatment method involves performing marginal or segmental resection with removal of adjacent bone tissue 1.5-2 cm from the visualized edge of the tumor. To confirm that the tumor has spread to adjacent tissues, it is recommended to carry out control radiography directly during surgery. In cases of ameloblastic carcinoma, excision of bone tissue is recommended at a distance of 2-3 cm from the visualized edge of the tumor. Recurrence of ameloblastoma is most often associated with the histological type of lesion and its location. The solid variant of the neoplasm is the most aggressive. Most often, ameloblastoma occurs in the distal areas of the lower jaw and affects the cancellous component of the bone through the mechanism of invasion, reaching the cortical plate and provoking its perforation. Once the tumor penetrates the periosteum, the risk of its further spread to the surrounding soft tissue increases. Inadequate lesion resection increases the risk of possible recurrence during follow-up. Cases of recurrent ameloblastoma have already been described by Grafft, Carvalho, Dolan, Marinelli, Stea, Zacharides, Vasan, Bianchi, Martins and Favaro, Su, Choi, Basat.
In most of the described relapses, restoration of the defect site after surgery was carried out using an iliac graft. Cases of recurrent ameloblastoma after radical treatment were described in studies by Sehdev, Shatkin and Hoffmeister, Mehlisch, Muller and Slootweg, Olaitan, Ueno, Eckhardt, Nakamura. It is known that the relapse rate with conservative treatment is significantly higher (60%) than with radical treatment (13%). The risk of relapse during surgical excision of ameloblastoma may be associated with retention of epithelial conglomerates of the neoplasm in the structure of the surrounding soft tissue. In the first clinical case described, the augmentation tissue succumbed to tumorigenesis, apparently due to the remaining tumor cells in the area of the osteoectomy. Therefore, before starting reconstruction of solid ameloblastomas, it is recommended to monitor the cleanliness of the edges of the excised tissues using control radiography. It is even better to wait for the results of a histological analysis of a tissue sample taken during the operation. Tumors in the infratemporal fossa are usually asymptomatic, and the main complaint of patients remains only signs of swelling and facial deformation. The infratemporal fossa is a pyramid-shaped structure that is located on the lateral surface of the base of the skull, deeper than the temporal arch, masseter muscle and ramus of the mandible. The medial part of the ramus of the mandible and the floor of the skull form the upper surface of the pyramid-shaped structure. The anteromedial part of the infratemporal fossa corresponds to the posterior surface of the upper jaw, and the posteroinferior part is formed by the pterygoid fascia. In fact, the infratemporal fossa is anatomically inaccessible, so it is almost impossible to monitor neoplastic growth in its structure.
Diagnosis and treatment planning for ameloblastomas localized in the infratemporal fossa should include the use of CT and MRI methods, which make it possible to establish an objective level of tumor spread. Conventional radiography in such cases is not sufficiently informative. Access to the infratemporal fossa can be formed transorally, transnasally, transpalatally, through the zygomatic bone, transcervically, and even through an extended maxillary approach. The approach through the zygomatic bone area is one of the most suitable for both resection of neoplasia and the formation of a temporal flap. The choice of surgical approach depends on the tumor type, clinical features, histological subtype, extent of spread and location.
In the second clinical case, relapse may be associated with preservation of the periosteum during a previously performed operation. It is in the periosteum that conglomerates of neoplastic cells could and will remain. A more extensive resection allows you to remove all tissue that has succumbed to neoplastic invasion, and thus minimize the risk of relapse. Carlson and Marx described the need to remove all anatomical structures adjacent to the tumor area for prophylactic purposes. This approach is reasonable when tumor invasion into surrounding soft and hard tissues is confirmed, since cases of recurrent ameloblastomas have been reported even 30 years after initial removal of the lesion. Laborde and Becelli described that in the cases of 7 patients, there was no evidence of tumor recurrence after treatment, and doctors used an approach with extensive excision of surrounding tissue.
Similar reports were also provided by Vayvada, Chaine and Basat. Vaishampayan suggested that recurrence of ameloblastoma after excision from the infratemporal fossa is associated with retention of the weakened process of the mandible after segmental resection procedures. Peacock et al concluded that the completeness of tumor excision can be verified not only by histological examination, but also by plain radiography. Although several publications indicate the resistance of ameloblastomas to brachytherapy, irradiation of recurrent types of lesions with high doses of 110 Gy was characterized by a fairly successful result.
During treatment for ameloblastoma, we recommend adhering to the following recommendations:
- In order to control the degree of invasion of large ameloblastomas into the surrounding soft tissue, it is necessary to use the MRI method.
- To control the completeness of excision of neoplastic tissue during surgery, it is necessary to use control radiography.
- Tumor resection margins should be widened to minimize the risk of future tumor recurrence.
- After confirming the cleanliness of the working field, it is necessary to carry out surgical reconstruction of the bone defect formed after tumor removal.
- Monitoring the area of preliminary localization of ameloblastomas after their resection is mandatory and should include the use of CT and MRI control.
conclusions
Based on the analysis of two clinical cases, we can summarize that the solid type of ameloblastoma is extremely aggressive and is characterized by a high rate of relapse. During treatment, it is necessary to take into account the risk of tumor invasion into the surrounding soft tissue, as well as the fact that the tumor, as it progresses, can provoke erosion of the cortical ball of the mandible. To gain a deeper understanding of the nature of the development of ameloblastomas, it is necessary to conduct a number of additional clinical and histological studies.
Authors: Chithra Aramanadka, Abhay Taranath Kamath, Adarsh Kudva (India)