Content:
- When it's all about physiology
- Why is there a problem?
- How much can root units become loose?
- Treatment
If, when pressing on a canine, incisor or molar, it begins to become very loose, you should urgently consult a doctor. The doctor will conduct a simple diagnosis and explain what’s going on. Refusal of dental treatment for pathological tooth mobility is a step towards a toothless smile.
Did you know that all dental pathologies can be cured with aligners?
I want to know more about the movement of teeth on aligners
A classification of this pathological process of tooth movement has been created:
- During the first stage,
the teeth move back and forth or, in medical terms, have vestibulo-orally directed mobility. - When, in addition to this, the teeth make movements in lateral directions, the second stage
. - At the most dangerous stage, the third stage
, vertical and circular movements are added to those mentioned earlier. The teeth are already beginning to emerge from the bone alveoli.
If the first two stages are subject to treatment and have a certain chance of recovery, then the last stage of mobility is a kind of sentence - the tooth should be removed.
Why does a violation occur?
Teeth begin to loosen for various reasons. The most common of them:
- Failure to comply with oral hygiene rules. If a person does not clean dental crowns well, a soft plaque is deposited on their surface. Gradually it turns into deposits of hard stone, extending along the roots deep under the gums. Then an inflammatory process develops. The soft tissues swell, turn red, and the ligamentous apparatus slowly collapses. A person may notice that his gums often bleed, and individual teeth become more loose than usual.
- Refusal to undergo annual professional hygiene procedures. This reason is also associated with the accumulation of tartar. It is very important to get rid of it once a year using a professional ultrasonic scaler.
- Bite distortions. It happens that crooked units exert strong pressure on their neighbors. Hence the weakening of the latter.
- Endocrine diseases. Many endocrine pathologies lead to deterioration of blood supply to periodontal tissues. A smaller amount of essential nutrients and oxygen reaches the tooth roots. As a result, they begin to stay in the holes worse.
- It is very important that artificial units do not interfere with natural ones and do not put pressure on them. They must match the dentition in both shape and size.
Poor installation of prostheses/implants.
- Congenital disorders in the structure of the dental system. It happens that mobility occurs due to the frenulum of the lips/tongue being too short. Then the ligamentous apparatus of the oral cavity does not function correctly.
- Periodontal inflammation , as well as other non-inflammatory diseases of periodontal tissues. With periodontal disease, periodontitis, units quickly become loose. The functioning of the ligamentous apparatus is greatly deteriorated.
- Destruction of alveolar processes. Not a very common cause of mobility, but still sometimes dentists encounter it. Atrophy is a consequence of inflammatory processes and traumatic injuries to the gums.
What mobility treatment involves depends on the underlying cause of the abnormal condition. Therefore, before drawing up a correction scheme, the doctor must carry out diagnostic procedures.
What is the cause of pathological mobility of teeth?
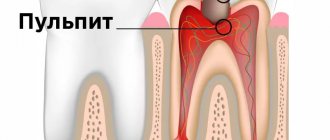
The well-known disease periodontitis is the main cause of this problem. This disease is inflammatory in nature and is characterized by destruction and reduction of tissue adjacent to the tooth. Dental deposits cause inflammation of the gums, which spread to the surrounding bone and ligaments. Inflamed tissue dissolves very quickly and is replaced by granulation tissue. And as a result of the fact that there is no more bone, the teeth acquire pathology in the form of mobility.
How much can root units become loose?
Doctors distinguish several degrees of mobility:
- I. The displacement of the crown in the horizontal direction is no more than one millimeter relative to its neighbors.
- II. Displacement of more than a millimeter. In parallel, slight loosening relative to the vertical axis may be observed.
- III. The unit moves in all directions.
- IV. The crown is very mobile and can even rotate around its own axis.
It is clear that it is easiest to treat a patient with the first degree of mobility. The stronger the loosening, the more serious manipulations the doctor has to carry out in order to keep the dentition intact.
Did you know that all dental pathologies can be cured with aligners?
Star Smile company is a leading Russian manufacturer of aligners.
The design of each set of aligners for patients is based on accurate mathematical modeling of the physiology of patient tooth movement, taking into account the existing pathology. What does it mean? This means that your teeth will be put in place as quickly and comfortably as possible with the help of Star Smile aligners! Star Smile specialists work in more than 70 (!) cities of Russia. We can always advise you in your city for free. And the main thing is to cure it once and for all with the help of aligners!
Treatment
When selecting a treatment regimen, the dentist takes into account:
- the general health of the patient;
- the reason for the violation;
- condition and location of the tooth;
- degree of loosening.
If the disorder is caused by internal processes, for example, hormonal imbalance or endocrine disease, then you need to work with the root cause. If the unit has become mobile due to injury or destruction of periodontal tissue, the question of splinting arises - installing a special dental structure that forces the crown to constantly be in one position.
Types of splints used in treatment
To relieve a person from severe mobility of fangs, molars, and incisors, doctors use the following splinting systems:
- Ring. Metal rings connected to each other are put on top of the crowns. As a result, mobile units become more stable.
- Semi-circular. It works in a similar way to the previous one, but the elements used look like half rings rather than rings. To achieve better aesthetics, they are fixed on the back side of the dentition, so when you smile they are almost invisible to others.
- Cap. The tire includes small caps connected to each other. They cover the cutting edges and partially extend onto the surface of the crowns.
- Coronal. Movable teeth are pre-ground and then covered with dental crowns. On both sides of the bridge, one healthy, stable unit is ground. Due to this, progression of loosening becomes impossible.
- Tab. This treatment option is similar to the cap treatment. Only here they don’t put caps on top of the crowns, but make indentations in the cutting surface of the teeth and place special miniature inlays in them. It turns out that all units of the row are reliably connected to each other.
Splinting is not always effective. If the abnormal process is severely advanced, then after a while the teeth begin to loosen again. But in most cases, doctors still manage to eliminate mobility using splints.
How do teeth move during orthodontic treatment?
A little theory about tooth movement
With the help of connective tissue fibers, the tooth is secured in the dental socket. This ligament is called the priodontal ligament. When the walls of the tooth socket are constantly exposed to the force coming from the aligners to straighten the teeth, areas of tension and pressure appear in the periodontium. Restructuring processes of bone tissue begin to occur in the tooth socket, which trigger bone resorption (resorption) and then its construction (osteogenesis). In the area of pressure, the periodontal fissure contracts, and in the area of tension, expansion occurs. Under pressure, the fibers of the ligament of the tooth and the nerves and blood vessels located in these places are compressed. The surface of the alveoli, located at the root of the tooth, experiences resorption.
In the area of tension, the ligaments of the tooth are stretched, and the process of bone tissue formation occurs. Both of these processes occur simultaneously, but with varying intensity, depending on the stage of treatment. The desired movement can only be achieved by applying a certain force to the jaw and teeth. Empirically, it has been found that less force exerted by aligners to correct a bite results in faster tooth movement. This is explained by the specific processes of regeneration and resorption of dental tissue and alveolar structures. This is why orthodontic tooth movement is a slow process, produced in the desired direction under the influence of small forces. If you make a greater load to move the teeth, the neurovascular bundles will not have time to rebuild in time. Without sufficient innervation and proper blood flow, the position of the tooth is difficult to correct.
Now let's see how teeth move in practice when treating orthodontic pathologies.
Tooth movement in the treatment of dental crowding
How crowded teeth are moved into a straight position using aligners
The clinical director of the Star Smile company, orthodontist Alexander Veniaminovich Spesivtsev, comments on the process of tooth movement:
— Let’s pay attention in the top video to how the upper and lower jaws come into contact with each other at the end of the treatment situation: we see an excellent position, excellent inclination of the front teeth, excellent shape, coincidence of all midlines, all linear parameters. Which, in general, allows us to think that the patient as a whole should be satisfied with this result.
The most important thing - as you have already noticed by watching the video - is that one of the key points of the aligner treatment technology is the creation of a 3D virtual setup
. That is, you and I sit in front of the computer and see WHAT will happen as a result of treatment BEFORE it starts. This emphasis is made on purpose, since many of us find it difficult to understand in principle how teeth move.
This kind of technology, this kind of 3D image, provides the answers. Therefore, look, analyze and begin your orthodontic journey in correcting your not very straight teeth!
Tooth movement during crossbite treatment
This patient has a crossbite. We see not a very narrow, but on the contrary, a very wide skirt-like shape of the upper central incisors. In aligner technology, we very often use a variety of different ways to adjust the size of teeth in order to create room for alignment. Therefore, here, as they say, “your hands are itching” to intervene in the situation and a little - let’s say - “file” the teeth on the sides to make them more attractive. And thereby create the optimal place for leveling.
A 3D virtual setup shows how straight his teeth will become with a crossbite
Quite classic tasks are faced by every doctor who shows a 3D virtual setup to a patient. The setup shows how the position of the teeth changes, how the shape changes slightly. On the lower jaw and on the upper jaw on the left we see the not entirely correct position of the last two teeth, two molars: the upper one tilts very strongly towards the buccal side, and the lower one, on the contrary, tilts towards the tongue. This is a crossbite. The video shows the movement of all teeth to their normal position.
Basic methods for determining tooth mobility
Traditionally, looseness is assessed based on the subjective sensations of the dentist and the patient. Accurate measurement is possible using special devices, but their use is limited due to the complexity of the technique. To make a diagnosis, an additional x-ray is performed to see periodontal disease or other disorders.
The direction and magnitude of the deviation are checked using tweezers. The tool is applied to the top of the crown and moved in different directions. To see vertical or circular movement, the crown is clamped with tweezers, lifted up or twisted.
Selective grinding of teeth
- one of the most common methods in the system of complex therapy of periodontal diseases. According to some data, 95.8% of patients with periodontal pathology need it.
Objectives of selective teeth grinding:
1. Elimination of premature occlusal contacts
2. Elimination of moments that block and interfere with the movements of the lower jaw
3. Elimination of deformation of the occlusal surface of the dentition.
There are different methods of grinding teeth, the most popular are the Jenkelson and Schuller methods.
The technique proposed by Jankelson (1979) is considered a functional method, however, premature contacts are removed in central occlusion.
According to Jenkelson's classification, premature contacts are divided into 3 classes:
1st contacts on the vestibular slopes of the buccal cusps of molars and premolars and the vestibular surface of the lower incisors
2nd contacts on the oral slopes of the palatine cusps of the upper molars and premolars;
3rd contacts on the vestibular slopes of the palatal cusps of the upper molars and premolars.
Indications for selective grinding:
— Presence of premature contacts of antagonist teeth in central, anterior and lateral occlusions;
— Absence or uneven wear of hard dental tissues;
— Deformations of occlusal surfaces;
— Bite abnormalities
Method of selective grinding of teeth:
-carried out before therapeutic and surgical procedures or in parallel with them.
- Preliminary grinding of teeth involves shortening protruding teeth and is intended to eliminate significant deformations of the occlusal surfaces that occur due to defects in the dentition. If significant shortening is necessary, depulpation of the latter is indicated.
- The final sanding is carried out in a certain sequence. First, premature contacts in various types of occlusion are eliminated, then when moving the lower jaw from central to anterior and lateral occlusions.
- Before grinding, an occludogram is obtained, which is stored to monitor the results of grinding. After carrying out this manipulation, it is necessary to polish the ground surfaces and coat them with fluorine varnish.
Orthodontic preparation for orthopedic treatment for periodontal diseases
In patients with periodontal pathology, the clinical picture is often complicated by deformations of the dentition; in addition, malocclusions in some cases can themselves lead to periodontal pathology, so orthodontic preparation before orthopedic treatment is of great importance.
Structurally, orthodontic appliances have some differences from classical ones, these include:
— Application of minimal forces to move teeth.
- Longer active treatment and retention period.
Temporary splints can be used as retention devices.
Functional traumatic overload of the periodontium
-occupies a special place among local causes in the etiology and pathogenesis of periodontal diseases. When chewing and swallowing, at the moment of closure of the dentition, the periodontium of each tooth perceives a force load, which under normal conditions is absorbed by special periodontal devices (cemento-alveolar, interdental fibers, etc.). Then it is transformed and transmitted to the bone structures of the jaws, the temporomandibular joint and the skull. This physiological load helps normalize trophism and metabolism, stimulates the processes of growth and development.
With pathological processes in the periodontium caused by common causes (vitaminosis, diabetes and other disorders of endocrine regulation, diseases of the gastrointestinal tract, cardiovascular system and nervous systems, etc.), the resistance of periodontal tissues decreases.
As a result of weakening of the periodontium, the usual occlusal load begins to exceed the tolerance of its structures and turns from a factor stimulating development into a traumatic one, disrupting the trophism of the periodontium and destroying its tissues. Traumatic occlusion occurs, which subsequently plays a leading role in the course of this disease.
The term “traumatic occlusion” was proposed by PR Stillman in 1919. Other terms have been proposed to characterize and define periodontal overload:
- “traumatic articulation”
- “functional traumatism”
- “pathological occlusion”
- “functional traumatic overload of teeth”, etc.
According to the mechanism of development, three types of traumatic occlusion are distinguished:
— Primary
— Secondary
— Combined
Primary traumatic occlusion develops against the background of unaffected periodontium as a result of the action of an occlusal load that is excessive in magnitude and/or direction.
Thus, primary traumatic overload of healthy periodontium can occur due to excessive magnitude, abnormal direction and duration of action of the occlusal functional load and steam function of the masticatory, facial muscles and tongue. More often than not, overload is caused by the simultaneous action of several causes.
Secondary traumatic occlusion:
Its pathogenesis is based on pathological changes in periodontal tissue. At the same time, degenerative and inflammatory processes develop in the supporting tissues of the teeth throughout the entire dentition, which are accompanied by:
1). resorption of bone tissue of the alveolar process.
2). Gingivitis.
3). destruction of the periodontium with the formation of a pocket.
4). suppuration from it.
Resorption of the bone tissue of the sockets leads to a disruption of the normal biological patterns of the structure and function of the periodontium. From this moment on, a radical change occurs in the biomechanical relationship between teeth and surrounding tissues.
Thus, a change in the ratio of the extra- and inside the alveolar part of the tooth is one of the pathogenetic mechanisms in the development of traumatic occlusion.
The clinical picture of secondary traumatic occlusion is diverse and depends on the patient’s age, the form of the underlying disease (periodontal disease, periodontitis), its severity and stage of development, the presence of dentition defects, malocclusion or tooth position, pathological abrasion and other traumatic factors.
If for primary traumatic occlusion orthopedic intervention is sufficient, then for secondary occlusion complex therapeutic (local and general), surgical and orthopedic treatment is required. The prognosis also varies. In case of primary traumatic occlusion, after eliminating the overload of the teeth in all periodontal tissues, reparative processes occur.