What is conduction anesthesia
Conduction anesthesia is a local anesthesia that involves the introduction of a special solution into the peripheral zone of the nerve that controls the site of the planned intervention.
In dentistry, this type is most often used in the treatment of teeth located on the lower jaw. The principle of operation of the method is based on blocking the transmission of impulses from nerves to the brain. This effect is achieved by introducing a special drug that has an analgesic effect. Once the blockage is established, the pain threshold is reduced to a minimum. The duration of anesthesia depends on the pharmacological agent used in the procedure.
Distinctive features of PA:
- for injection, drugs of higher concentration are used (up to 2% of active substances) than with other methods of local anesthesia;
- sensitivity is blocked not in the area of intended intervention, but in the nerve that innervates this area;
- minimal number of complications and side effects that occur after using the technique;
- full control of the time of anesthesia and the area of effect of the drug.
Areas of application of conduction anesthesia:
- traumatology;
- Maxillofacial Surgery;
- dentistry;
- physiotherapy;
- therapy;
- neuralgia, etc.
Differences from the usual and rules of conduct
For local anesthesia using PA, solutions of more concentrated anesthetics are used: up to 2% Trimekain or Lidocaine is injected into the area closest to the nerve endings (perineural) or under the nerve sheath (endoneural).
Basic Rules:
- The anesthetic is administered perineurally, sometimes endoneurally, but slowly, in small doses - not exceeding 5 ml.
- Before anesthesia, a mandatory aspiration test to check the body’s response to small doses of the injected drug.
- To guarantee pain relief, the needle is moved at an angle of 90° to the nerve trunk, and the drug solution is administered in a fan-shaped manner .
- Before the blockade, adrenaline is added to the anesthetic - a proportion of 1:200,000.
- Use only drugs of a certain concentration that do not exceed permissible standards, for example: 1.0% Trimecaine solution - no more than 100 ml; 2.0% – 20 ml.
- For PA, special needles coated with NanoLine from the company PAJUNK®, Germany, are used. Such needles provide easy penetration, thanks to a special sharpening at an angle of 45-60°.
When using large-diameter needles, it is recommended to inject a special solution under the skin to create a “lemon peel”, which significantly facilitates the injection of the anesthetic.
Prices for PA in medical centers and dental clinics in Moscow range from 110 to 200 rubles , depending on the painkillers used.
Conduction anesthesia in dentistry
In dentistry, there are cases when conduction anesthesia is indicated:
- removal of teeth or roots;
- the presence of inflammatory processes in the oral cavity or soft tissues of the face;
- procedures used for the prevention and treatment of periodontal disease and advanced caries;
- dental implantation;
- impossibility of using general anesthesia.
Manipulation in some areas of the oral cavity is difficult due to inaccessibility, so extraoral and intraoral methods are used to administer anesthesia.
In the lower jaw, in the presence of inflammation (on the mucous membrane or soft tissues), one of the extraoral methods is used for pain relief:
- submandibular – the effect of the drug is aimed at blocking the lower alveolar nerve;
- subzygomatic – the injection is administered under the edge of the cheekbone arch;
- mandibular - the mandibular foramen is anesthetized.
After administration of the anesthetic, the numbing effect occurs within 15 minutes. The duration of anesthesia depends on the drug chosen.
Of the intraoral varieties of the method, the following are used:
- apodactylous – the inferior alveolar nerve is blocked;
- torusal - the drug is injected into the mandibular ridge, reducing sensitivity in the area where the molars and premolars are located.
When anesthetizing the teeth of the upper jaw, the following methods are used:
- tuberal - anesthesia is used for the treatment or removal of molars located in the upper dentition;
- infraorbital – the drug anesthetizes the anterior wall of the maxillary bone, mucous membrane, alveolar process;
- palatal – the palate is anesthetized, as well as the alveolar process;
- incisal - the drug is injected into the mucous membrane between the canine and the incisor; the hard palate, nasopalatine nerve and soft tissues surrounding the tooth are subject to freezing.
The anesthesia begins to take effect 10 minutes after injection.
What operations are performed under PA
With the help of such local anesthesia, individual parts of the human body are anesthetized, so it is used only in certain cases.
Surgical dentistry deals with complex operations in the oral cavity aimed at preserving and restoring teeth and improving their appearance.
How much will it cost to treat pulpitis of a three-channel tooth, read in a new publication.
In this article we will tell you what can cause teeth grinding during sleep.
Here https://www.vash-dentist.ru/lechenie/zubyi/lz-mudrosti/bolit-chto-delat-v-takom-sluchae.html you will find recommendations on what to do if your wisdom tooth hurts.
In dentistry, PA has found wide application in the following surgical interventions:
- complex tooth extraction;
- extraction of the tooth root with and without gum incisions;
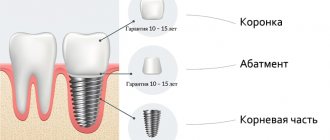
- implantation – implantation of artificial teeth;
- sinus levare – operations before implantation;
- flap operations for the prevention of periodontal disease.
Quite often, surgical intervention is necessary on the mucous membrane, so increased demands are placed on instruments and materials - the level of sterility is maximum, and the material for sutures must be atraumatic and have excellent biocompatibility.
Varieties of methods
Conduction anesthesia is divided into two types:
- central - provides for the identification of the nerve trunks of the trigeminal nerve for the subsequent introduction of an anesthetic into the body;
- peripheral - the drug is injected into a branch coming from the trunk nerve.
| Conduction anesthesia | |
| Name of the method type | Description |
| Infraorbital | After administration of the drug, the peripheral endings of the infraorbital nerve are blocked. Anesthesia is administered through the mouth and outside the mouth. The point of delivery of the anesthetic is the infraorbital foramen. The landmark is a line running through the second premolar to the mental foramen. The distance from the alveolar margin to the infraorbital foramen is approximately 3.5 cm. |
| Infraorbital | Used to “freeze” the front part of the jaw. The method is intraoral; to perform it, you need to pull back the lip to expose the gums. The needle is installed between the projections of the incisor roots and moves upward towards the cheek. |
| Tuberal | The technique is used for anesthesia of the upper molars, maxillary sinuses, and oral mucosa. The injection site for the drug is just below the transitional fold of the second tooth of the upper row. The needle plunges down to 2.5 cm. |
| Palatine | The area of action of the drug extends to the area from the canine to the extreme molar. The amount of painkiller is 0.3 ml. |
| Incisive | The method ensures blocking of the nasopalatine nerve. After the injection of 0.3 ml of anesthetic, the palate, fangs and all teeth located between them “freeze”. The injection site for the drug is near the incisive papilla. |
| Apodactyl | The injection site for the drug is determined by the fold formed as a result of retraction of the pterygomaxillary ligament. An additional reference point is the center of the distance between the wisdom teeth of the upper and lower rows. The method is used to anesthetize the teeth of the lower jaw. |
| Podzykulova | The anesthesia technique is performed outside the oral cavity. The needle is installed on the edge of the zygomatic arch at a right angle, the depth of immersion is 3-3.5 cm. The amount of anesthetic is 3-5 ml. |
| Submandibular | Method of administering the drug outside the oral cavity. The puncture site is the lower edge of the lower jaw, 2 cm from the posterior edge (base of the jaw). When the needle is deepened by 3.5 cm, the area of action of the anesthetic extends to the inferior alveolar nerve; when the needle is advanced another 1 cm, the effect expands to the lingual nerve. The amount of the drug used is 2 ml. |
| Mandibular | The method anesthetizes the teeth of the lower row. The puncture site is the border of the middle and lower jaw fold, which has the appearance of a wing. After passing through the dentin, the needle tip rests on the bone, and half the dosage of the drug is administered. The procedure is repeated on the other side of the dentition to introduce the rest of the product. |
| Torusal | The technique is based on mandibular anesthesia, but expands the area of action of the anesthetic, including the nerve branch from the cheek. |
| Mental | The method is used to reduce the sensitivity of the anterior zone of the lower jaw using intraoral and extraoral techniques. The puncture with a needle is carried out in the transitional fold, the orientation is towards the 1st molar. The drug is administered in an amount of 0.5-1 ml to the location of the apical part of the root of the 2nd premolar. The effect extends to the area where the incisors, canines and premolars are located on one side of the dentition, the alveolar process, lips and chin. |
| Bershe-Dubov method | The method of pain relief is based on the mandibular technique; the drug is injected under the cheekbone (at a distance of 2 cm from the tragus). The needle is deepened to 2-2.5 cm. Novocain is used as an anesthetic. The anesthesia effect extends to half of the dentition. This method is more often used in maxillofacial surgery and physiotherapy. |
Tuberal anesthesia zone
Typically, the zone of tubercular conduction anesthesia reaches in front of the space between the upper second premolar and the upper first molar, behind the free end of the alveolar process, including part of the tubercle of the upper jaw and the buccal mucosa in the area of the upper first, second and third molars.
While studying the method, we used a dental probe to test the sensitivity (actually, pain, since even after the onset of analgesia, tactile and temperature sensations often remain) of the entire area after each tubercular conductive anesthetic injection. We noted several cases where painlessness extended to the middle of the second and even first premolars, although in the vast majority of cases the anesthesia zone border in front was the middle of the upper first molar.
How can we explain cases (albeit very rare) of anesthesia spreading forward to the upper premolars, when, as is known, only three upper molars are innervated by the posterior superior alveolar nerves, and the upper premolars are supplied by the middle upper alveolar nerves.
The authors who studied this phenomenon explain it by the existence of anastomoses between adjacent nerves. However, this can explain the onset of some anesthesia only in part of the second upper premolar, but not the spread of anesthesia to the upper first premolar inclusive.
We explain this phenomenon as follows. It is known that the middle superior alveolar nerves begin from the infraorbital nerve in the middle or posterior part of the infraorbital groove. However, there are cases when these nerves (middle superior alveolar nerves) begin, like the posterior superior alveolar nerves, in the pterygopalatine fossa before the entry of the infraorbital nerve into the groove of the same name. Then they enter jaw through holes that are also located on the back surface of the upper jaw. Thus, during the release of anesthetic fluid at the target point of this anesthesia, on the tubercle of the upper jaw, to interrupt the conduction of the posterior superior alveolar nerves with a similar anomaly of the infraorbital nerve, the conduction of the middle superior alveolar nerves can also be interrupted (the anesthetic solution in this case enters a bit higher)
The mucous membrane and periosteum on the side of the palate are not anesthetized during a tubercular conduction anesthetic injection, and to obtain complete anesthesia of all tissues of the upper jaw in the area of three molars, it is necessary to add palatal (palatal) conduction anesthesia to the tubercular conduction anesthesia of the anterior palatine nerve at the greater palatine foramen.
Anesthesia technique
The conduction method procedure is carried out in compliance with the following technique:
- A consultation with a doctor, during which the specialist finds out what chronic diseases the patient has. Examination and review of the tests help identify contraindications.
- Identifying the nerve endings that need to be blocked.
- Treating the puncture site with a disinfectant.
- Injection of the selected drug into the designated areas. In this case, special attention is paid to the dosage and speed of administration of the solution.
- Monitoring the patient after the anesthetic injection.
Immediately before surgery, the patient is asked control questions to determine the sensitivity threshold.
The duration of the pain relief effect depends on the chosen agent and dosage. Modern drugs provide a fairly long-lasting effect of anesthetics (40-60 minutes or more).
When performing the procedure for administering an anesthetic, you should adhere to the general rules:
- the temperature of the drug should correspond to 36.6°;
- For injection, properly sharpened needles are used so as not to damage tissues and nerve endings;
- the drug is injected into the area of the nerve or directly into the trunk;
- in some cases, before using the conduction method, the puncture site is anesthetized with Analgin (intradermal injection);
- When performing all manipulations, you should use only sterile instruments and materials.
Feelings during conduction anesthesia
The first sign of the effects of conduction anesthesia is slight muscle numbness and a feeling of heaviness. In dentistry, drugs and doses are used that can numb the area in a matter of minutes.
Peripheral nerve blockade using conduction anesthesia is almost 100% safe. The risk of infection remains, but it is minimized in conditions of absolute sterility. Also, a hematoma may appear at the puncture site due to damage to the vessel. This most often happens when the patient takes drugs that reduce blood clotting.
After treatment, the feeling of numbness persists. Sensitivity will remain absent for some time (depending on the patient's response to the drug). Some people do not respond well to anesthesia, and pain may occur during the procedure. You need to notify the doctor, he will give an additional injection.
The duration of the effect is individual for each patient. Complete lack of sensitivity sometimes lasts for hours. The risk of nerve damage is less than one percent.
Drugs used
Successful anesthesia depends not only on the technique used, but also on the drugs. The list of anesthetics for conduction anesthesia includes the following:
- solutions of the Articaine series , differing in duration of action and effectiveness (Ultracaine, Septanest, Ubistezin);
Ultracaine
Septanest
Ubistezin
- Lidocaine is a powerful pain reliever with minimal toxin content;
- Melivacaine is a modern drug that provides pain blocking for up to 40 minutes and has virtually no contraindications;
- Novocaine is one of the most common drugs, low-toxic, and quickly hydrolyzes in the biological environment and blood.
How effective and safe is the method?
For the use of PA in dentistry, special carpules have been developed - ampoules with a strictly dosed drug, which allows you to accurately set the dose of the required anesthetic , with the addition of Epinephrine, artificial adrenaline.
In addition, the use of carpules allows you to comply with all recommended antiseptic rules and prevents cases of overdose due to the carelessness of the doctor:
- The carpula needle is so thin that the injection itself is almost not felt, which has a beneficial effect on patients with a negative attitude towards injections.
- Before the injection, the needle insertion site can be additionally numbed with a spray containing lidocaine.
- The analgesic effect lasts about an hour and has virtually no side effects, so after the procedure you are allowed to drive.
The advantage of PA is that it can be carried out several times: an adult of average weight is injected with up to 7 ampoules of the drug Ultracaine (one ampoule per 10 kg of weight), without much harm to the body. There are no contraindications for nursing mothers and pregnant women.
When performing PA, devices such as the neurostimulator model “Magnon-29D” are often used, the cost of which is 89,800 rubles.
Such devices allow you to determine the location of superficial nerves and how close to the nerve the needle is using the interrupter electrode included in the kit.
Neurostimulation allows you to avoid accidental injection of drugs into the nerve body, injury to it with the subsequent development of neuropathy, thereby increasing the safety of pain relief to 100% of the result.
In many clinics in the Russian Federation , when performing PA, they use a double method - electrical neurostimulation plus ultrasound control .
Advantages and disadvantages
In order to analyze the conduction method of pain relief, it is recommended to familiarize yourself with the important advantages and disadvantages of the technology.
Main advantages:
- the possibility of administering an injection outside the operated area;
- long, and most importantly controlled, period of action of the anesthetic used;
- minimum amount of administered drug;
- soft tissues in the operated area are not deformed;
- decreased salivation activity;
- the safety of the technique, which allows the use of pain relief for children (over 12 years old), pregnant and breastfeeding women;
- affordable cost of the procedure.
Flaws:
- the technique of performing anesthesia requires skill and skill;
- high probability of drug administration inside the vessel;
- age restrictions for the procedure (children under 12 years old);
- possibility of injury to nerves or blood vessels.
Contraindications
The method of conduction anesthesia is considered safe, but there are still a number of contraindications to the use of the procedure. Among the main ones:
- unstable psycho-emotional background, psychiatric diseases;
- the presence of infection on the tissues or skin where the drug is planned to be administered;
- individual characteristics of the body (allergy to the active substances of the anesthetic);
- serious changes in the topography of the operated area resulting from past surgical interventions;
- the presence of purulent foci in the area of therapeutic manipulations.
There is also an age limit; children under 12 years old are not prescribed PA.
Conduction anesthesia in pregnant women
At any stage of pregnancy, the use of anesthesia is undesirable. But in life, various circumstances arise that require immediate solutions. Experts prefer the conduction method of pain relief, which is due to the following factors:
- the drug is injected into the cavity above the dense membrane of the spinal cord, the influence of the active substance extends only to the lower part of the body and limbs, the woman remains conscious;
- the ability to use anesthetics that do not affect the health of the fetus (for example, Ultracaine);
- the painkillers used are quickly eliminated from the body.
If it is possible to postpone treatment procedures using anesthetics, then it is worth considering that the second trimester is considered the most favorable time during pregnancy. At this stage, the fetus has developed systems and organs, which means there is no risk of harming the baby’s health.
When performing dental treatment, you should refuse anesthesia in the following cases:
- in the first trimester of pregnancy;
- in the ninth month;
- if you are allergic to the components of the drug.
Some medical procedures in a child cause not only pain, but also fear, which has great harm on the child’s psyche. Among the existing methods of reducing the sensitivity threshold to a minimum for schoolchildren, general anesthesia is chosen when it comes to a complex intervention. If there are contraindications, preference is given to conduction anesthesia, which is explained by a number of advantages:
- quick effect;
- controlled duration of action of the drug;
- complete blocking of impulse transmission to the brain;
- health safety;
- minimal risk of complications.
How does the patient feel?
When the tissue is pierced with a needle, the patient will experience discomfort and mild pain. The severity of this pain symptom does not exceed the pain felt when taking blood for examination.
The drug is administered slowly, and at this moment the patient may experience fever, slight dizziness, and bloating from the inside. These unpleasant sensations disappear after a few seconds.
When the anesthesia begins to take effect, the patient experiences increasing numbness of the lips. Conduction anesthesia guarantees the absence of discomfort and pain when performing any dental procedure, during which the patient remains conscious. At his request, this anesthesia can be combined with sedation.
Possible complications
The use of innovative technologies for conduction anesthesia minimizes the occurrence of complications and negative consequences. Only one case in 50,000 procedures provokes neuropathy and an inadequate response of the body to the administration of anesthetic.
Other complications that also occur quite rarely include:
- muscle weakness;
- creepy crawly effect;
- partial numbness of tissues.
These symptoms are temporary; a maximum of a month after the application of conduction anesthesia disappears without a trace.
In this case, the functionality of the damaged nerves is completely restored. Many people ask the question: is it painful to have conduction anesthesia? Painful sensations during the process are minimized, however, they exist.
The conduction method of pain relief is considered one of the most effective ways to eliminate pain caused by mechanical action on tissue. Therefore, it is used for complex surgical interventions and blockade of peripheral nerves during the postoperative period.