Chronic periodontitis: description and symptoms
Unlike acute periodontitis, chronic periodontitis is often practically asymptomatic, that is, it is not accompanied by severe swelling and severe pain. That is why many patients come to the doctor when conservative treatment of chronic periodontitis is impossible, and to eliminate complications they have to resort to more radical measures. Chronic periodontitis in the acute stage has much more pronounced symptoms.
Symptoms of chronic periodontitis
- pain
- soft tissue swelling
- tooth mobility
- enlarged lymph nodes
- weakness
- temperature increase
Exacerbation of chronic periodontitis is often associated with concomitant diseases, as well as hypothermia, decreased immunity and other factors.
Symptoms of periodontitis
Symptoms of acute periodontitis are:
- acute pain in the teeth, intensifying at the time of percussion;
- swelling of the lips and cheeks;
- swelling of the gums;
- tooth mobility;
- low-grade fever (37.2-37.7 C);
- enlarged lymph nodes.
Chronic periodontitis is characterized by:
- pain when eating (especially hot);
- sharp pain when biting;
- swelling of the mucous tissues near the affected tooth;
- hyperemia of the oral mucosa;
- the appearance of submucosal, subcutaneous granuloma.
During an exacerbation, a fistulous tract may appear next to the affected tooth, from which pus is released. Often the opening of the fistula tract is localized in the area of the cheeks, cheekbones and chin. Serous-purulent fluid may ooze from the wound. Alternatively, granulation tissue may swell. After an exacerbation, closure of the fistula is observed with the formation of a scar in its place.
Chronic type of granulomatous periodontitis
often asymptomatic. As a result, a greatly enlarged granuloma changes into a cyst, which is characterized by the following clinical manifestations:
- swelling of the gums;
- severe pain in the tooth;
- changes in enamel color;
- hyperemia;
- flux.
If the cyst increases critically in size, even a jaw fracture is likely.
Fibrous chronic periodontitis
characterized by mild symptoms. With this form of the disease there may even be no pain at all. This form of periodontitis is the least dangerous. But in case of exacerbation, the pain can instantly intensify, swelling of the soft tissues of the collateral type is observed, loose teeth and enlarged lymph nodes appear.
Complications of chronic periodontitis include abscess of the soft tissues of the neck and face, meningitis, osteomyelitis of the jaws, periostitis, brain abscess, purulent sinusitis and blood poisoning.
Causes of chronic periodontitis
Chronic apical periodontitis (chronic apical periodontitis, chronic root periodontitis) is so named because the inflammatory process occurs in the area of the apex of the tooth root. This type of disease is often the next stage of the acute form, but it can also develop independently. Based on their origin, experts distinguish two types of chronic periodontitis.
✔
Infectious chronic periodontitis. Occurs as a result of the activity of pathogenic bacteria in the oral cavity. The presence of foci of infection contributes to the penetration of bacteria into periodontal tissue and the development of the disease.
✔
Non-infectious chronic periodontitis. It can be caused by trauma and mechanical damage to the teeth, including due to doctor errors during therapeutic treatment. Another reason may be an allergic reaction to medications (in particular, arsenic and anesthetics), as well as the toxic effects of pulp decay products.
Medicinal periodontitis
Drug-induced periodontitis develops when aggressive liquids or drugs, such as arsenic paste, formalin, tri-cresol formalin, and phenol, enter the periodontium. Penetration into the periodontium occurs through the root canal.
This also includes periodontitis, which develops in response to the removal of phosphate cement, resorcinol-formalin paste, pins and other filling materials into the periodontium during the treatment of pulpitis. Drug-induced periodontitis also includes periodontitis due to allergies as a result of the use of drugs that can cause a local immune response (antibiotics, eugenol, etc.).
Diagnosis of chronic periodontitis
Unfortunately, without the necessary equipment, it is very difficult to identify chronic periodontitis. A visual examination performs a purely formal function, since even in the presence of symptoms (pain, swelling, etc.), it is necessary to determine the type and stage of periodontitis in order to draw up the most effective treatment plan. Today, diagnosis of the disease is carried out in several proven ways.
- X-ray examination. The most popular type of diagnostics. All types of chronic periodontitis can most often be detected on a regular targeted X-ray. In case of fistula formation, a narrow-profile X-ray examination - fistulography - is often prescribed.
- Radiovisiographic examination. A more modern and gentle x-ray examination, during which the image is transferred to a computer screen.
- Electroodontodiagnosis (EDD). Diagnosis of inflammatory processes in the dental pulp by monitoring its response to electric current.
- In the case of periodontitis, specialists use differential diagnosis to distinguish it from other dental diseases with similar symptoms.
Diagnostics
To diagnose periodontitis, it is enough for an experienced dentist to examine the patient’s oral cavity. The presence of fistulous openings, inflammation of the gums around the tooth and the presence of symptoms typical of periodontitis will help to recognize the disease. To differentiate pathology from pulpitis and periodontal disease, use:
- X-ray of the tooth - the images will show rarefaction of the periodontium, the presence of a purulent focus, granuloma or cystic neoplasm at the root apex;
- CT is a more informative method of radiation diagnostics, which allows you to obtain a three-dimensional detailed image of the tooth and its surrounding tissues, on which the boundaries of periodontal inflammation will be visible, and its sources will also be determined.
Chronic forms of periodontitis
Chronic fibrous periodontitis
Periodontal tissues are gradually replaced by connective tissue, and the inflammatory process is usually mild. One of the most common types of periodontitis, which is most often asymptomatic. With exacerbation, pain, enlarged lymph nodes and fever are possible. When diagnosed on an x-ray, you can notice an expansion of the periodontal fissure.
Treatment of chronic fibrous periodontitis is usually easier compared to other forms.
Chronic granulating periodontitis (chronic granular periodontitis)
In the apical region of the root, granulation tissue is formed, which actively replaces bone. In terms of symptoms, this is the most pronounced type of chronic periodontitis, which manifests itself in the form of pain, especially when pressing on a tooth or biting. During an exacerbation, the pain intensifies, and fistulas with purulent discharge may occur. On an x-ray, it is quite easy to notice dark, irregularly shaped areas: clear evidence of the development of granulating periodontitis. It is advisable to treat chronic granulating periodontitis quickly enough to avoid the spread of granulation tissue.
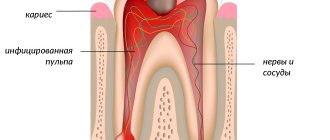
Chronic granulomatous periodontitis
A type of periodontitis in which a purulent sac forms near the tip of the root, which, as it grows, first turns into a granuloma, and then into a cyst filled with dense epithelial tissue. The diameter of the cyst can exceed 1 centimeter. In the early stages it hardly manifests itself, but in later stages pain occurs, and the color of the tooth may also change. On x-ray it appears as a dark round spot. Treatment of chronic granulomatous periodontitis in some cases requires surgical intervention, since it is often not possible to get rid of the cyst using conservative methods.
Acute periodontitis –
In accordance with the theory of the course of the inflammatory process, the acute form of periodontitis is usually divided into serous and purulent forms. Diagnosis of acute serous and acute purulent periodontitis is carried out only by symptoms, because There are usually no changes on the x-ray.
This is due to the fact that the diagnosis of “acute periodontitis” is made only when it first occurs. It can arise, for example, as a consequence -
- during untreated pulpitis,
- poor-quality filling of canals (after treatment of pulpitis).
Acute serous periodontitis –
Symptoms - at first, the pain may be spontaneous, which is due to the fact that the inflammatory exudate accumulating in the periodontium is localized in a confined space, and therefore it compresses the nerve endings. The pain intensifies sharply when biting on a tooth.
It is periodontal edema that is associated with patients’ complaints about the feeling of elongation of the causative tooth, and its premature closure with antagonist teeth of the other jaw. The swelling actually causes the causative tooth to protrude slightly vertically.
There may be slight swelling of the soft tissues of the face in the projection of the causative tooth, but upon palpation (feeling) it is usually painless. Since the pulp, as a rule, is already dead during the development of periodontitis, probing the carious cavity is usually painless. There are still no changes on the x-ray at this stage of inflammation.
Acute purulent periodontitis –
Symptoms: After about two days, the serous stage of inflammation turns into a purulent stage. This is associated with a significant increase in symptoms. Painful sensations take on the character of throbbing pains with rare pain-free intervals.
As a result of the pus melting the periodontium (the ligamentous apparatus of the tooth), the tooth becomes mobile. Significant swelling of the soft tissues of the face may occur. The gums in the area of the causative tooth are usually sharply painful when pressed. The radiograph still does not show any significant changes.
Stages of development of acute purulent periodontitis (Fig. 1-4) –
- Periodontal stage - the purulent process is limited to the area of the periodontal fissure, i.e. a microabscess occurs in the area of the apex of the tooth root (Fig. 1). Clinically, this may correspond to the appearance of a feeling of an overgrown tooth.
- Endosseous stage - pus penetrates the bone tissue and infiltrates it (Fig. 2).
- Formation of a subperiosteal abscess - pus accumulates under the periosteum (Fig. 3). Clinically manifested by severe swelling of the gums, soft tissues of the face, and severe pain. Patients call this gum flux.
- Submucosal stage - destruction of the periosteum occurs and pus comes out into the soft tissues (with the formation of an abscess in them). After the periosteum breaks through, the pain immediately subsides, because tension in the focus of purulent inflammation decreases. But at the same time, swelling of the soft tissues of the face increases (Fig. 4).
Acute purulent periodontitis: video
In the video you can see how, when opening a tooth with acute purulent periodontitis, pus begins to emerge from the mouth of one of the root canals.
Treatment of chronic periodontitis on teeth
Despite the fact that acute and chronic periodontitis are similar in many ways, treatment of chronic forms of periodontitis is usually more difficult and takes longer than the acute form. Treatment of acute chronic periodontitis is most often carried out using conservative methods and may require endodontic intervention: opening the tooth cavity to drain purulent exudate, filling the canals. Antiseptic drugs and antibiotics are also actively used. In the case of chronic periodontitis, the treatment method depends on the stage of the disease and the presence/absence of complications. Based on this, a conservative or surgical treatment plan is drawn up.
Treatment methods for chronic periodontitis
✔
Conservative treatment of chronic periodontitis. It implies a whole range of measures to eliminate the source of the disease. First of all, the tooth canals are cleaned, antiseptic medications are administered, and anti-inflammatory drugs and antibiotics are taken if necessary. After sanitation, the canals are filled with medicinal filling paste, after which it is necessary to wait for the restoration of periodontal tissue for 1 to 3 months. After this period is completed, a permanent filling is performed. In the treatment process, techniques such as electrophoresis, laser and UHF therapy are often used.
✔
Surgical treatment of chronic periodontitis. Surgical methods for treating chronic periodontitis one way or another involve invasive intervention in periodontal tissue. Typically, this technique is used in advanced stages of periodontitis and when complications develop (cysts, fistulas, etc.). Modern dentistry has a number of surgical techniques that allow you to save part of a root or tooth. These include: tooth root resection (removal of part of the root along with a pathological formation), cystectomy (operation to remove cysts and granulomas), and hemisection (removal of the crown part of a multi-rooted tooth along with the root). Despite the fact that chronic periodontitis of permanent teeth is most often tried to be cured with the help of tooth-preserving manipulations, in the most severe cases complete tooth extraction is indicated.
Periodontitis
- Conservative treatment of patients with periodontitis
Clinical and morphological features of chronic periodontitis in childhood cause difficulties in developing treatment tactics, which should be aimed at achieving the ultimate goal - preserving the tooth and eliminating foci of chronic infection.
Conservative methods of treating periodontitis do not always achieve complete elimination of the odontogenic focus of infection, so there is a need for surgical intervention. When choosing a method of sanitation of permanent teeth with periodontitis, it is advisable to use the recommendations proposed by T.F. Vinogradova:
- determine the functional value of the tooth based on the permanent dentition;
- assess the condition of each root (the degree of formation and secondary pathological root resorption) during an x-ray examination;
- reveal the nature of the pathological process and the degree of its spread relative to each root (according to X-ray examination);
- determine the accessibility of the root canal for full instrumentation;
- assess the possibility of the manifestation of chronic periodontitis as a focus of odontogenic infection that maintains the disease
There is an opinion that in case of severe chronic diseases of a child (chronic pneumonia and bronchitis, kidney diseases, frequent respiratory infections, severe sore throats), the indications for radical sanitation sharply expand. T.F. Vinogradova believes that in children, removal of a permanent tooth at the current level of development of endodontics is a last resort. In difficult cases, conservative surgical methods should be used to save the tooth.
Treatment of patients with periodontitis involves very complex manipulations. It is necessary to correctly assess the condition of a temporary tooth with periodontitis. It must be removed if: less than 2 years remain until the physiological change; with tooth mobility of II-III degree; with root resorption of more than 1/3 of the length; The history reveals several exacerbations of the pathological process. A temporary tooth that cannot be treated can become a chronic source of infection in weakened children with reduced resistance. The opinion of some authors - to preserve a temporary tooth with periodontitis at any cost - from the standpoint of preventing anomalies of permanent occlusion is unjustified. Sanitation of teeth with formed roots in children is not fundamentally different from the treatment of those in adults. The most labor-intensive treatment is for temporary and, especially, permanent teeth with incomplete root formation.
It is not always possible to come to the right decision based on the clinical picture alone. Sometimes a shallow carious cavity without a fistula on the gum or even an intact tooth can be observed with significant resorption or early cessation of root formation. Therefore, there is a strict rule: before treating a tooth with chronic periodontitis, especially in children, it is necessary to conduct an x-ray examination to assess the condition of the root and periapical tissues and the degree of involvement of the permanent tooth germ in the inflammatory process.
Treatment of patients with acute periodontitis, which has developed against the background of acute or chronic pulpitis, is reduced to the elimination of inflammation in the pulp, which leads to the cessation of the inflammatory process in the periodontium.
When acute arsenous periodontitis occurs, treatment is aimed at removing necrotic pulp and neutralizing arsenous acid, which is carried out by introducing arsenous acid antidotes into the root canal: a 5% alcohol solution of iodine or unithiol, which is less toxic and more effective. After the pain and inflammation subsides, the canal is sealed.
If acute periodontitis is accompanied, in addition to severe pain, by a reaction of the surrounding soft tissues and tooth mobility, then after opening the tooth cavity and removing decay from the tooth canal, it is advisable to leave the latter open to ensure the outflow of inflammatory exudate. General anti-inflammatory therapy is prescribed. After the disappearance of acute inflammatory phenomena, treatment is the same as for chronic periodontitis. When acute periodontitis develops as a result of the filling material being removed beyond the apex of the tooth, painkillers, UHF therapy, fluctuarization, and laser irradiation are prescribed. If acute periodontitis occurs as a result of defective canal filling, repeated treatment is necessary.
Medicinal substances used for filling root canals must have bactericidal properties, be biologically active, fill not only macro-, but also micro-channels, accelerate the elimination of the inflammatory process in periapical tissues and promote bone regeneration.
Currently, oil-based hardening pastes are used for filling, as they have a water-repellent effect and are absorbed in temporary teeth parallel to root resorption. Such pastes include eugenolic acid, pastes based on sea buckthorn oil, and rosehip oil. These pastes are plastic, harden slowly, which makes it possible to re-fill the canal, and are not washed out of the canal, like soft pastes based on glycerin. Resorcinol-formalin paste can be widely used for filling canals in permanent and temporary molars. It is plastic, penetrates well into narrow and curved areas of the canal, for which a more liquid consistency is used. It inhibits the growth of microorganisms, including yeast, which many other drugs have no effect on.
ON THE. Belova, V.V. Zhilina, E.N. Fadeev, when treating children aged 1 to 3 years with chronic periodontitis, all endodontic interventions were consistently performed, filling 1/2 of the canal with an oil-based paste. The authors note that heavy bleeding from periodontal tissue indicates either an exacerbation of chronic periodontitis, or the ingrowth of granulations into the unformed root canal or its pathological resorption. Such teeth must be removed. In this group of children, the first temporary molars were also removed, since their full treatment is difficult.
In case of chronic fibrous periodontitis, the canal is filled to the apex. Filling the roots of formed permanent teeth with pastes promotes the restoration of bone tissue in the periapical region in a period of 3 to 18 months, even with significant bone loss.
When filling temporary teeth with the same pastes, bone tissue is almost not restored, since during the period of tooth change, resorption prevails over bone formation. The destroyed area of the cortical plate, limiting the developing follicle, is never restored, therefore, a temporary tooth with chronic periodontitis must be removed, otherwise there is a threat to the permanent tooth germ.
Treatment of children with chronic periodontitis of multi-rooted teeth with patent canals is carried out using the same techniques as in adults. The resorcinol-formalin method is quite reliable in the treatment of temporary and permanent molars, when mechanical treatment is very difficult. In teeth with narrow and curved canals, the treatment time should not be reduced. After mechanical and medicinal treatment of the passable part of the canal for 2-3 visits, the narrow parts of the canals are treated with a resorcinol-formalin mixture. If the canals are difficult to pass, it is necessary to first restore them through mechanical means. The mixture, penetrating into the macrocanal and dentinal tubules, hardens due to the polymerization of its phenolic and aldehyde components. Bone tissue restoration occurs not only in the periapical tissues, but also at the level of root bifurcation, destruction in the area of which is not a contraindication to treatment.
- Treatment of patients with chronic periodontitis in permanent teeth at the stage of incomplete root formation
Treatment is very difficult even for an experienced doctor and often ends in failure. The development of chronic periodontitis is facilitated by rough extirpation of the pulp when performing the vital method in an immature tooth
If x-ray reveals that the cortical plate in the area of the bottom of the socket is not destroyed, then the growth zone is most likely preserved. In this case, you can count on the continuation of root formation, so manipulations in the root canal should be carried out with greater caution. Unfortunately, in the vast majority of cases, the growth plate dies because children seek treatment too late. In case of exacerbation of chronic periodontitis, the tooth cavity is opened, decay is carefully removed from the canal and it is treated with antiseptic. The tooth is left open until the inflammatory process is completely eliminated. In severe cases, antibiotics and sulfonamide drugs are prescribed in doses appropriate to the child’s age. It is recommended to drink plenty of fluids and liquid high-calorie foods.
When treating patients with any form of periodontitis, the main attention is paid to opening the tooth cavity, mechanical and medicinal treatment of the canals.
Associations of various types of microorganisms play a significant role in the etiology and pathogenesis of chronic periodontitis. Therefore, a positive clinical effect can be obtained by using a complex of drugs aimed at eliminating aerobic and anaerobic microflora. In dental practice, various antiseptics are used to treat root canals: 3% hydrogen peroxide solution, 0.2% chlorhexidine solution, 1% quinosol solution, as well as enzymes.
ON THE. Kozionova et al. observed good rapid cleanability of root canals using a 5% sodium hypochloride solution, which also helped stop bleeding in the apical part of the root canal and had a drying effect. As an analogue, the drug “Chlorax” is used - a 5.25% solution of sodium hypochloride.
A positive clinical effect was obtained by E.F. Kononovich when treating canals with other antibacterial agents, taking into account not only their bacteriological activity, but also the possible toxic effect on the peri-apical tissues. Metrogil (India) and its domestic analogue metronidazole (Trichopol) had the greatest antibacterial effect and minimal toxicity in the treatment of patients with chronic periodontitis.
E.A. Savinov and V.D. Shchegolev, in the treatment of children with chronic periodontitis of teeth with unformed roots, in addition to traditional antiseptics, chlorophyllipt was used to treat root canals. This drug has a bacteriostatic and bactericidal effect; its 1% alcohol solution is widely used in purulent surgery and gynecology. When turunda with a chlorophyllipt solution is introduced into a root canal with a large amount of necrotic masses, its color changes from green to white. Clinical observations have shown that chlorophyllipt effectively suppresses the growth of root canal microflora during a purulent-inflammatory process, and can also serve as an indicator of the cleanliness of the root canal.
In addition to traditional pastes (eugenol, resorcinol-formalin), collagen paste containing collagen, methyluracil, bismuth hydroxide-nitate, and zinc oxide has been widely used in recent years. Immediately before use, the specified composition is mixed with eugenol to the consistency of a paste. Clinical and radiological data indicate that the use of collagen paste can stop the inflammatory process and accelerate tissue restoration in the periapical area in chronic forms of periodontitis.
R.S. Kundzinya recommends Intradont-D for filling root canals with both completed and unfinished root formation of permanent teeth with chronic periodontitis. The peculiarity of its action is the stimulation of reparative osteonesis. However, removal of zinc-eugenol paste and intradont past the apex leads to necrosis of the periapical tissues. E.A. Savinova, V.D. Shchegoleva, L.A. Ilyenkov received good results when filling.
In recent years, a number of companies have synthesized hydroxyapatite for clinical use. Hydroxyapatite, being part of root fillings, has ideal biological compatibility, low solubility, contains 39-40% calcium and 18-19% phosphorus. patented and launched the production of hydroxyapatite preparations with the brand name “Hydroxyapol”. Positive experience has been accumulated in the use of hydroxyapol-containing paste for filling root canals.
VC. Leontiev et al. conducted a comparative study of pastes for filling root canals: resorcinol-formalin, zinc-eugenol, pastes with endomethasone and based on hydroxyapol in the treatment of adult patients with chronic periodontitis. Paste with hydroxyapol gave the best results, promoting the rapid elimination of the inflammatory process, and after 6 months the authors noted the restoration of bone tissue in the periapical area.
The effectiveness of conservative treatment of patients with chronic periodontitis should be checked after 6-12 months. If the focus of destruction increases, conservative surgical treatment or tooth extraction is indicated.
- Conservative surgical methods of treating patients with periodontitis
To increase the effect of sanitation of permanent teeth with chronic apical periodontitis, conservative treatment is combined with surgical procedures that partially preserve tooth tissue. Such conservative surgical methods include: resection of the root apex, amputation of the root or roots, hemisection, coronradicular separation and tooth replantation.
In the practice of pediatric dentistry, the development and implementation of these methods was inspired by the work of S.D. Lapshin et al. and M.S. Ivanova. The idea itself - to remove roots from multi-rooted teeth that are inaccessible to therapy, and preserve the remaining ones and even use them for prosthetics - arose a long time ago and was embodied in several surgical treatment methods
- Removal of affected roots while preserving the tooth crown is root amputation.
- Removal of the part of the crown adjacent to it by the root - coronradicular amputation.
- Dissection of a tooth through the area of root divergence, when the affected root is removed along with the corresponding half of the crown - hemisection of the tooth. This method is used mainly in the treatment of lower molars and sometimes upper premolars.
- The division of the lower molar into two equal parts, each of which takes the form of a premolar, and the upper molar into three parts. This method is used when the roots of the teeth are healthy, but there is damage to the furcation. It is called coronradicular separation
- Interradicular granulectomy - grinding off the edge of the intersocket septum after detachment of the mucoperiosteal flap.
- Resection of the root apex.
There are three groups of indications for radical treatment of children with chronic periodontitis of permanent teeth.
- Somatic indications. Issues of treatment of children and adolescents with chronic foci of odontogenic infection must be considered comprehensively with an assessment of the patient’s somatic status and his membership in a particular health group. The use of radical methods to eliminate chronic foci of odontogenic infection is one of the most important measures to prevent exacerbation of somatic diseases. Conservative therapy alone, which does not provide complete sanitation of odontogenic lesions in children and adolescents with somatic diseases, is insufficient to maintain an optimal level of health.
- Ineffectiveness of conservative treatment. The reasons may lie in errors in endodontic treatment, a decrease in the reactivity of the patient’s body. Sensitization to the filling material or its strong and prolonged irritant effect are also possible. The indication for conservative surgical methods is the absence of bone tissue regeneration in the periapical pathological focus for more than 12 months after conservative treatment.
- Difficulty or impossibility of conservative treatment in cases of: damage to the furcation, perforation of the bottom of the tooth cavity or roots, insufficient obturation of the canal (canals) with hardening filling material (cement), obliteration of the canal, denticles, dentinal bridges, the presence of a fragment of an endodontic instrument in the canal, especially extending beyond the apex root, bur head, additional roots inaccessible for filling canals (with a bend angle of more than 50°), excessive removal of filling material beyond the apex of the root, caries damage to the crown and root of a molar, in which further restoration of these parts is impossible, retrograde infection of adjacent teeth, extensive foci of bone tissue resorption.
General contraindications to conservative surgical methods of treating patients with chronic periodontitis: severe concomitant diseases (children of the fifth health group), mental illness, emotionally labile patients.
Local contraindications: significant tooth destruction and the impossibility of restoring it by filling or prosthetics.
Conservative surgical treatment methods include the following steps
- Therapeutic treatment with careful instrumental and transcanal medicinal treatment of root canals. Eugenol paste can be used to fill the root canals of incisors and premolars, and resorcinol-formalin paste can be used for molars. The anatomical shape of the tooth is restored using amalgam or composite materials.
- Surgical treatment consists of performing one of the operations listed above. If necessary, splinting is carried out.
- Orthopedic treatment is carried out 4-5 weeks after surgery. Religious inlays and crowns are used. The anatomical shape of the crown can be restored by applying a filling.
After conservative surgical methods, physiotherapeutic procedures are indicated to relieve pain, reduce postoperative inflammation and stimulate regenerative processes in bone tissue. Inflammatory phenomena, manifested by pain, swelling, hyperemia of the mucous membrane in the area of the operation, completely disappear on the 5-6th day.
Dynamic X-ray observation is carried out. Bone tissue restoration occurs within a period of 3 to 11-12 months. Bone tissue forms most quickly around single-rooted teeth.
- Operation techniques
Resection of the root apex. It is carried out in cases where it is not possible to seal the canal to the apical foramen. Conduction or infiltration anesthesia. A semi-oval or trapezoidal incision is made and the muco-subperiosteal flap is peeled off. After trephination of the bone and exposure of the apex of the tooth, the granulations are scraped out. The exposed part of the root at the apex is cut off with a bur until the filling material is found on the cut. If it is absent, the canal is filled retrogradely, after which the wound is sutured. Drainage for 1 day is advisable.
Granulectomy. Indicated if the canal is filled up to the apical foramen. The technique differs from the previous one in that the granuloma is removed without violating the anatomical integrity of the root.
Interradicular granulectomy. It is used when the pathological focus is localized in the area of divergence of the roots of the upper and lower molars, as well as in case of minor perforations of the bottom of the tooth cavity, including with the removal of filling material beyond the boundaries of the tooth.
After anesthesia and detachment of the muco-subperiosteal flap, the bone tissue is trepanned in the area of root divergence. The granulation tissue is scraped out, and excess filling material located in the interroot space is removed. The affected furcation tissue and the adjacent edge of the interradicular septum are carefully ground off. The wound is sutured.
Root amputation. The canal is first filled above the level of the intended amputation. A filling is applied.
After anesthesia, a semi-oval or trapezoidal incision is made, the muco-subperiosteal flap is peeled off, and the bone is trepanned. The root is exposed and cut off with a bur from the divergence of the roots or a stump of 3-6 mm is left. The stump is carefully ground off. The granuloma is removed. The wound is sutured.
Hemisection. It is divided into simple and complex. With simple hemisection, the tooth crown is dissected to the point where the roots diverge, and the part of the crown that is not subject to treatment is removed along with the root using forceps.
Complex hemisection is used if difficulties are expected in root removal. With this type of hemisection, gingivotomy and folding of the mucosubperiosteal flap are performed. After removing the root, the wound is sutured. During the operation, special attention should be paid to preserving the interradicular septum, on which the stability of the preserved fragment largely depends. If the septum is damaged, the tooth is fixed with a ligature wire to the adjacent one.
Coronradicular separation. The indication for coronal-radicular separation is damage to the molar furcation by an inflammatory process due to extensive perforation of the bottom of the tooth cavity or its destruction by a carious process. The operation consists of cutting a two-root tooth into 2, and a three-root tooth into 3 equal parts. After removal of the interroot lesion, orthopedic restoration of the crown is performed.
Coronradicular amputation. Used to remove one of the roots of the upper molar due to the impossibility of its treatment and at the same time significant destruction of the crown above this root. The cut of the destroyed crown is made according to the projection of the root in the bifurcation area. The root with a fragment of the destroyed crown is removed with forceps.
Hemnreplantation. They are used only on molars of the lower jaw in cases where other methods of root canal therapy cannot be carried out, and half of the tooth crown is completely destroyed by the carious process. The operation consists of dividing the tooth between the roots into 2 parts, followed by replantation of one tooth fragment into the socket.
After anesthesia, the mucosubperiosteal flap is dissected and removed. The crown of the tooth is cut into 2 parts with a bur. The affected root, granuloma or cyst is removed. Then the tooth fragment to be replanted is removed. On this fragment, resection of the root apex and retrograde filling with amalgam are performed. The root edge is ground, the tooth fragment is replanted into the socket, and the gum flaps are sutured. Splinting is advisable.
Complications. It is possible to open the maxillary sinus during amputation of the roots of molars. In this case, the wound is carefully sutured with a closed suture (without drainage), healing occurs within the usual time frame. Anti-inflammatory and physical therapy are prescribed. When operating on the mandible, care must be taken regarding the mandibular nerve canal. In the postoperative period, inflammatory complications are possible. Anti-inflammatory and physical therapy are carried out.
- Surgical methods for treating patients with periodontitis
Surgical methods for treating patients with periodontitis include the removal of a tooth that cannot be treated and the opening of purulent foci in the surrounding tissues (purulent lymphadenitis, abscess, purulent periostitis).
The principle approach to deciding on a surgical treatment method is different for temporary and permanent teeth. The determining factor when deciding whether to remove a temporary tooth can be the patient’s age, or more precisely, the time remaining until the tooth is replaced. In cases where there is less than 0.5-1 year left before replacing a tooth affected by periodontitis, it must be removed. The degree of root resorption is also important, which does not always coincide with the standard timing of tooth changes. Indications for the removal of temporary teeth are also unsatisfactory treatment results, recurrent fistulas, frequent exacerbations of the process, involvement of the permanent tooth germ in the pathological process. Indications for the removal of primary teeth in children belonging to the “risk group” are more widely established.
The indication for removal of a permanent tooth affected by periodontitis is complete destruction of the crown and the impossibility of therapeutic or conservative surgical treatment.
Repeated treatment of chronic periodontitis
Sometimes specialists have to re-treat chronic periodontitis. This is usually due to the fact that previous treatment was ineffective. This could be poor cleaning and filling of canals, defects during surgical procedures, non-compliance by the patient with rehabilitation rules, as well as an initially incorrectly selected treatment plan. Secondary treatment almost always takes longer and is more difficult. In this case, it is still possible to do without tooth extraction or carry out repeated conservative treatment, however, quite often the patient comes with already developed complications that require surgical intervention.
Symptoms of the disease in acute form
Periodontitis often develops quickly. Signs of a purulent process:
- Constant pain, which intensifies, pulsates and creates a feeling of fullness, can radiate to neighboring areas;
- The impression of an enlarged tooth - mobile and sharply painful when touched;
- Inability to close teeth;
- Hyperemia of the gums and cheeks;
- Pain on palpation;
- Pus comes out through the fistula, swelling decreases and pain dulls;
- Sulfebrile temperature.
Chronic periodontitis: treatment at home
Any form of periodontitis cannot be cured at home: this should only be done by a professional doctor. The only option is antibiotic therapy, which in the vast majority of cases is prescribed as an addition to complex treatment. The same applies to traditional medicine. In medical practice, there have been cases when a cyst or granuloma resolved without any intervention, but this should not be attributed to miraculous natural decoctions and tinctures. Much more important are preventive measures that will help improve oral health and avoid problems with teeth and gums. In this case, some traditional medicine can really help, but the main measures to prevent periodontitis are good hygiene, proper nutrition and regular visits to the dentist.
Why periodontitis is dangerous
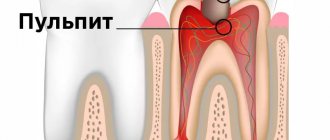
Periodontal inflammation is the stage following pulpitis in the spread of infection from a carious tooth.
Its focus is located at the apex of the root and is a small cavity filled with pus.
In the absence of therapy, the infectious-inflammatory process spreads to the periodontium - the intermediate tissues that separate the roots and neck of the tooth and the bone tissue of the gums.
Important! The periodontium surrounds the entire subgingival part of the tooth and plays the role of cement that fixes the tooth in the jaw. When it is damaged due to periodontitis, the likelihood of tooth loosening and loss increases many times over.
Most often, periodontitis is localized at the apical part of the root affected by pulpitis. If left untreated, the inflammation spreads further, covering the entire subgingival part of the tooth. As the disease develops, a purulent cavity forms around the roots, which sooner or later opens onto the mucous membranes of the oral cavity or onto the skin of the face. When it becomes chronic, periodontitis is accompanied by constant suppuration with the outflow of contents through a fistula - long-existing ducts, the walls of which do not grow together.
Complications after periodontitis treatment
Within a week after treatment, pain may be observed when clenching the jaws, but this phenomenon is considered normal and is not a complication. To minimize the risk of such an effect, you should try not to use the treated tooth - do not touch it or chew with it, do not eat too cold or hot food.
One of the most common complications is the poor quality of filled canals. This does not necessarily happen because the dentist is inexperienced: the fact is that the canals can be very long and curved, so placing a full filling material in them can be problematic.
The consequence of this is severe pain, swelling and the development of an inflammatory process, which can lead to the recurrence of periodontitis.
To avoid this complication, after filling, the dentist should send the patient for an x-ray to monitor the result, and also schedule a follow-up visit a couple of weeks after treatment to monitor the situation.
If root resection was performed during treatment, the recovery process may take a slightly longer period of time: pain in the gums may be observed for several weeks, which can be reduced by rinsing with antiseptics.
Prevention of the development of chronic fibrous periodontitis
In order to properly organize preventive measures, you need to know that any of the chronic forms of periodontal inflammation occurs, as a rule, against the background of the formation of pathogenic microflora and untreated caries.
Taking this fact into account, we can say with confidence that regular and proper brushing of teeth can significantly reduce the risk of developing chronic oral diseases. Brush your teeth twice a day, rinse your mouth after every meal and never go on a night's rest without performing hygiene procedures - and you will not have to deal with such complex and dangerous pathologies as chronic periodontitis.
For those who are forced to wear orthodontic appliances, we can recommend ASEPTA dental gel, which reliably protects teeth and gums from the development of inflammation. Special ASEPTA rinses will also help in creating the correct microflora. Do not forget that wearing dentures and braces can expose teeth to prolonged traumatic stress. Provide them with especially careful care during these periods.
Clinical researches
Clinical studies have shown that for the treatment of chronic localized periodontal disease of traumatic etiology in young patients, a complex of therapeutic and preventive measures is required, which includes domestic gum balm and gum gel with propolis (JSC VERTEX, Russia), as well as personal hygiene products oral cavity in the form of therapeutic and prophylactic toothpaste "ASEPTA PARODONTAL SENSITIVE" (JSC "VERTEX", Russia) and mouth rinses "ASEPTA PARODONTAL ACTIVE" and "ASEPTA PARODONTAL FRESH", (JSC "VERTEX", Russia), which allows within 6 months after completion of complex treatment, not only improve oral hygiene and reduce inflammatory processes in the gums by 55.37%, but also reduce the number of relapses of localized periodontitis by 21.36%.
To increase the effectiveness of treatment of chronic localized periodontitis of traumatic etiology in young people, it is advisable to include a gum balm in the complex of treatment and preventive measures, which should be used after completion of the surgical stage (curettage) as a gingival dressing, and subsequently used to optimize gum regeneration, gum gel with propolis, should be used against the background of adequate individual oral hygiene.
Sources:
- Prevention of recurrence of localized periodontitis in young A.K. YORDANISHVILI, Doctor of Medical Sciences, Professor, North-Western State Medical University named after. I.I. Mechnikov, Military Medical Academy named after. CM. Kirov, International Academy of Sciences of Ecology, Human Safety and Nature.
- Report on clinical trials to determine/confirm the preventive properties of commercially produced personal oral hygiene products: mouth rinse "ASEPTA PARODONTAL" - Solution for irrigator." Doctor of Medical Sciences Professor, Honored Doctor of the Russian Federation, Head. Department of Preventive Dentistry S.B. Ulitovsky, doctor-researcher A.A. Leontiev First St. Petersburg State Medical University named after academician I.P. Pavlova, Department of Preventive Dentistry.
- Clinical studies of antisensitive toothpaste “Asepta Sensitive” (A.A. Leontyev, O.V. Kalinina, S.B. Ulitovsky) A.A. LEONTIEV, dentist O.V. KALININA, dentist S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry, St. Petersburg State Medical University named after. acad. I.P. Pavlova