The eruption of wisdom teeth is a natural process, which for some goes unnoticed and painlessly, while for others it causes a lot of trouble. For example, when a wisdom tooth grows into the cheek. The symptoms of this pathology will be described below with photographs and advice from specialists. You cannot let the situation take its course, otherwise unpleasant consequences may arise, deterioration of well-being and the condition of neighboring teeth.
Regardless of a person’s actions, his hygienic culture, lifestyle and health, each dental unit has its own direction of growth and its own characteristics. Pathologies usually arise due to genetic and natural predisposition, which are practically not amenable to any influence.
Causes of abnormal growth
“Eights” or, as dentists call them, third molars, are a vestige left over from our ancient ancestors - the Neanderthals. The structure of their skull was different, and their jaw was more elongated, so there was enough room for 16 teeth. Over time, the structure of the head changed, human food became softer, and the jaws stopped protruding strongly forward - the “eights” simply became cramped. Sometimes they literally have nowhere to grow, so they erupt wherever there is at least a little free space. There are frequent cases when a dystopic wisdom tooth begins to grow towards the cheek in both the upper and lower jaws) - you can understand what kind of anomaly this is from the visual photo below.
The pathological process of eruption also arises because the “eights” do not have milk precursors, and therefore, no ready place for growth and location, like the other units of the series. Therefore, they have to pave the way with difficulty, in several stages. For the same reason, in some people, third molars do not grow at all - they either remain in the thickness of the bone or do not form at all.
For your information! In some European and American clinics, doctors remove third molars at the stage of their formation, thus saving patients from the painful periods of eruption of “eights” and possible complications with their growth. Russian dentists do not adhere to this practice, believing that there is no point in removing a healthy “eight”: sometimes when other molars fail, it can become a support for an orthopedic bridge during prosthetics.
Sometimes the cause of a dystopic “eight” can be a pathology of the jaw structure (as a rule, such a defect is inherited) or a non-standard shape of the third molar (too large a crown). You can see in detail what a wisdom tooth looks like growing into the cheek in the photo.
Why do people need wisdom teeth?
Are wisdom teeth necessary? This is perhaps one of the most common questions asked by millions of patients who come to the dentist’s office. Ancient people who lived tens of thousands of years ago had a larger and more massive jaw, so they could accommodate more teeth. This helped chew hard and tough foods. Over time, the need for this disappeared, so wisdom teeth gradually became a vestigial organ. Of course, only nature knows the exact answer to the question of why wisdom teeth grow in modern people, but one should not think that they are absolutely useless. Despite the fact that third molars are almost not involved in distributing the chewing load, wisdom teeth in adults can become a support for a prosthesis, and also prevent bone loss in the absence of neighboring molars.
Symptoms of improper germination of the "eight"
Since the third molar rarely erupts immediately, it is difficult to determine with the naked eye whether it is positioned correctly. If the “figure eight” remains vertical relative to the plane of the jaw, then doctors consider this to be the norm. Dentists, as a rule, retain this unit.
Such teething is accompanied by discomfort, and the norm is considered to be slight swelling of the gums and very mild pain when closing the jaws. If the condition goes beyond these signs, then with a high probability we can say that the “eight” is growing incorrectly, and then you should consult a doctor for qualified help.
Symptoms indicating that a wisdom tooth is growing sideways to the cheek:
- the appearance of wounds or ulcers on the mucous membrane: from the fact that the sharp edges of a growing wisdom tooth cut and scratch the cheek,
- bleeding gums: when brushing or eating hard foods,
- the cheek is visually enlarged and swollen,
- the appearance of headaches,
- increased body temperature: sometimes above 38 degrees,
- enlarged cervical lymph nodes,
- inflammation of the throat mucosa,
- the appearance of an unpleasant taste in the mouth,
- signs of intoxication of the body: aching muscles, joints, stiff neck, general weakness, sometimes nausea, etc.
Diagnostics
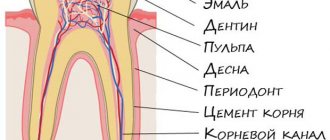
Any pathology associated with the problematic eruption of one or more wisdom teeth should always be investigated through x-ray diagnostics. To determine the position of the tooth in the jaw (inclination, shape, configuration, structure, how it grows), an orthopantomogram is used.
OPTG is a high-quality panoramic image of all teeth on both jaws. Another diagnostic method that will help you understand why your wisdom tooth hurts is visiography.
Consequences of pathological growth
If such a process is left to chance, the complications can be very serious. Since the “eight” is forced to push and put pressure on the root “sevens”, which are already tightly seated in their places, such a confrontation can cause inflammation of the periosteum (periostitis), and this, in turn, can provoke osteomyelitis, pericoronitis, and phlegmon.
It is important to know! Mechanical rubbing of the cheek mucosa provokes the formation of a non-healing wound, where infection will sooner or later penetrate. This threatens the formation of a purulent abscess in the soft tissues, which will have to be removed surgically. In addition, an abscess is dangerous because the infection can travel through the lymphatic or bloodstream to any other area of the head and cause inflammation, for example, of the maxillary sinuses, middle ear, and even meningitis.
Another danger is the resorption or destruction of the roots of the “sevens”. When squeezed, blood and, consequently, nutrients stop flowing to them. The roots and tissues of the tooth become weak, leading to early loss of the unit. The pathological growth of the eighth crowns leads to deformation of the gums, which contributes to the growth of plaque and the development of cervical caries in the seventh teeth.
There are cases when inflammation during pathological eruption of wisdom teeth leads to inflammation of the trigeminal nerve. It passes close to the edge of the jaw, so there is a high probability of infection spreading to the nerve fibers.
How to relieve pain at home
Of course, if serious symptoms occur that indicate improper growth of the third molar, you should seek medical help from a dental clinic. But what to do if a “attack” of pain during the eruption of a wisdom tooth growing into the cheek caught a person, for example, on the road? Or for some other reason he cannot urgently see a doctor.
Important! If a wisdom tooth grows into the cheek and hurts, then under no circumstances should you use warm compresses or otherwise warm the area of inflammation. It is also dangerous during this period to visit baths, saunas, solariums, and carry out procedures aimed at warming up the body.
The following measures will help relieve discomfort and temporarily alleviate the situation:
- brushing your teeth: during teething, you can perform oral hygiene after each meal to prevent particles from being carried under the hood of the swollen gums,
- rinsing: you can use both medications (chlorhexidine, furatsilin, Miramistin) and herbal decoctions (calendula, sage, chamomile, celandine). Rinsing with a baking soda solution (1 teaspoon per glass of warm water) helps relieve pain.
- At night you can take non-steroidal anti-inflammatory drugs: (nimesulide, meloxicam, Nise, etc.) or simple analgesics, but not aspirin - it thins the blood, and if the doctor removes it the next day, the healing process will last longer .
Clinical researches
Repeated clinical studies have proven that the two-component mouth rinse ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component rinses - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The role of hygiene products in the treatment of periodontal diseases (S.B. Ulitovsky Honored Doctor of the Russian Federation, Honored Dentist StAR Prof., Doctor of Medical Sciences, Department of Preventive Dentistry of Pavlov Pavlov State Medical University, St. Petersburg) S.B. Ulitovsky - Honored Doctor of the Russian Federation, Honored Dentist of StAR, Prof., Doctor of Medical Sciences; E.S. Alekseeva - associate professor, candidate of medical sciences; A.A. Vasyanina - associate professor, candidate of medical sciences; V.A. Grigoriev - Associate Professor, Ph.D.
- The use of drugs from the Asepta line in the complex treatment of inflammatory periodontal diseases (N.V. Berezina E.N. Silantyeva S.M. Krivonos, Kazan State Medical Academy. Kazan.) N.V. BEREZINA, E.N. SILANTIEVA, S.M. KRIVONOS Kazan State Medical Academy
How is removal carried out?
The “eights” that grow toward the cheek must be removed. Doctors consider it inappropriate to use other methods that are usually used to treat dystopic teeth - for example, treatment with braces. The fact is that the root canals of “wise” units are almost always strongly curved and narrowed, which makes high-quality endodontic treatment impossible.
In addition, when brushing, most people rarely treat their eighth crowns as thoroughly as their other teeth because they are difficult to access, and therefore this is where caries most often occurs. It is undesirable to have a “time bomb” in the oral cavity, so it is better to remove third molars that have pathologies. The stages of wisdom tooth removal are given below.
1. X-ray examination
First, an X-ray is taken: targeted and sometimes panoramic (and in difficult cases, a computed tomography is performed) to understand whether the molar is growing correctly, whether it is advisable to leave it and what obstacles may arise during removal.
Treatment in the presence of foci of inflammation
This includes purulent abscesses, ulcers on the mucous membrane, etc. If the eruption of the third molar causes severe pain, then removal and treatment of dental disease are carried out in parallel. And if you can wait a couple of weeks to remove it, then you first need to cure the inflammation so that the infection does not get into the open wound.
Surgical stage
The technology for performing the surgical stage when removing 1 third molar is not universal and is classified depending on the clinical picture:
- if the roots of the “eight” are not intertwined: the patient is given anesthesia (an injection with an anesthetic is given in the gum), and then the tooth is slightly loosened and removed with special forceps,
- if the roots are intertwined and touch neighboring ones: first, anesthesia is also given, then the tooth is drilled out with a drill, the interroot septa are removed, and the roots are removed one by one. After removing all the debris (in this and the next case), the wound is treated with an antiseptic, the bleeding is stopped and stitches are applied. After which the patient is given recommendations for the rehabilitation period,
- if the tooth is impacted: that is, not fully erupted, then removal turns into a full-fledged operation. After anesthesia, the surgeon makes an incision in the gum to gain access to the crown. If the crown has already erupted a little, but is growing into the cheek, then the tooth can be fixed with forceps and immediately removed, but if the entire molar is immersed in the bone, then you will have to drill it into pieces (possibly cut the bone as well) and extract the tooth in fragments.
Attention! In advanced cases, when the pathological growth of the “eight” has caused complications (for example, the development of phlegmon), an operation to remove it and eliminate complications is carried out in a maxillofacial hospital under general anesthesia.
Possible complications after removal - and their differences from the norm
Three conditions are considered normal after surgery: pain, swelling and bleeding. Let us consider the characteristics of normal and pathological conditions in detail.
Pain in the intervention area
Painful sensations may persist for 2-3 days, and to get rid of them, you can take NSAIDs (Ibuprofen, for example) or any painkiller. If the pain intensifies or is poorly suppressed by analgesics, you should consult a doctor.
“When I first heard the name of the film “The Hateful Eight,” I thought that it was just about my long-suffering eight))) But, of course, I was the sufferer here. The eruption lasted for years, and the surgeon probably periodically opened the gum cap four times, until I decided that that’s enough, I’m waiting for Monday and going to ask for removal. They took an x-ray and scheduled surgery in 2 days. And, no matter how afraid I was, everything went perfectly - the injection froze the jaw longer than the removal itself lasted. I had to take sick leave, though, because on the first evening it felt as if a truck had driven into my jaw. But gradually everything returned to normal, the main thing is to listen carefully to what the doctor advises while the wound heals.”
Valentina88, review from otzovik.com
The appearance of swelling and hematoma on the cheek
Swelling can also last for two days. As a rule, it subsides as soon as blood circulation in the injured area improves. If the swelling increases, the temperature rises, or other signs of inflammation appear, then you need to urgently go to the dental clinic. A hematoma (or bruise) on the cheek appears on the 2nd day after complex removal and can persist for up to 7-14 days, gradually turning pale.
Bleeding from the wound
Bleeding after removal is a natural protective reaction of the body. As a rule, within 2-3 hours after surgery, a blood clot forms and closes the socket. After this, the bleeding either stops altogether or remains in the form of so-called ichor for several more hours. If light bleeding continues a day later or within 3-4 hours after removal heavy bleeding persists, then this is a reason to seek medical help.
What does the appearance of pus and temperature indicate?
If purulent discharge appears around the hole, if the body temperature rises to 38 degrees, pain from the removal site begins to spread to the eye, ear, neck, nose, signs of intoxication appear (headache and muscle pain, weakness, dizziness, etc.) These are signs of a developing complication. A quick visit to the dentist will avoid their negative consequences.