Problem: a 65-year-old woman consulted an ENT doctor at the Family Dentistry with complaints of discomfort in the right maxillary sinus. The examination showed chronic sinusitis, mycetoma of the maxillary sinus and the presence of a fistula in the maxillary sinus connecting the oral cavity and sinus.
Solution: joint management of the patient by an ENT specialist and an implant surgeon was developed - problematic teeth were removed, a mycetoma was removed from the maxillary sinus, the fistula was sutured, the patient is preparing for dental implantation in the upper jaw.
Why can an implant “go” into the sinus?
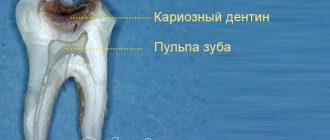
The maxillary sinus or sinus is a paired nasal sinus. It is a volumetric cavity above the upper jaw, which is connected to the nose by a thin septum, and is separated from the teeth by a narrow alveolar ridge (jaw bone). The inside of the cavity is lined with mucous membrane. The lower wall in the molar area is thin, which often leads to penetration of dental roots, filling material, and odontogenic infection.
Perforation of the maxillary sinus by a dental implant can occur:
- Upon implantation . Restoration of the upper chewing teeth is accompanied by the risk of damage to the maxillary cavity by the implant. Therefore, before implantation of the structure, a sinus lift is performed (building up the jaw bone by raising the bottom of the sinus and filling the resulting space with bone material). Neglecting the procedure leads to sinus perforation. Other reasons include the lack of professionalism of the doctor, the use of excessive force when screwing in the artificial root, incorrect placement of supports, and the presence of previously untreated perforation.
- In the postoperative period. It occurs as a result of a violation of the osseointegration of the implant with the tissues of the jaw due to inflammation, sinusitis, diseases of the bone tissue of infectious origin and other pathologies, such as osteoporosis.
- After installing the crown. Rarely seen. Among the reasons: premature prosthetics (up to 3 weeks after implantation of a titanium root), increased tension in the area of implantation, excessive chewing load on the structure, fracture of the rod.
Odontogenic sinusitis: traditional and endoscopic surgical treatment methods
Errors by a dentist during endodontic treatment of maxillary teeth often lead to the removal of filling material into the maxillary sinus [1, 3, 6]. Mechanical effects, as well as the cytotoxic and sensitizing effect inherent in almost all types of modern pastes for obturation of the root canals of teeth, lead to inflammatory and purulent-necrotic changes in the mucous membrane of the maxillary sinus. As a result, an isolated chronic pathological process gradually develops, exerting a pathogenic effect not only on surrounding tissues, but also on the body as a whole [5, 7, 8].
The relevance of research
Current treatment methods for the above category of patients are often associated with surgical trauma to tissues not involved in the pathological process: bone, mucous membrane, soft tissues of the cheek. Some authors propose rather contradictory approaches. Some experts believe that the filling material in the sinus will dissolve over time, others believe that its presence does not have a harmful effect on the sinus mucosa and its functional state. This approach certainly leads to the progression and spread of the inflammatory process from the maxillary sinus to other paranasal sinuses and the orbit.
Some experts believe that the filling material in the sinus will resolve over time, others believe that it does not cause serious harm to the mucous membrane of the sinus and its functional state. A number of authors note that rhinogenic infection often exacerbates the latent odontogenic process, and this combination of sources of infection can lead to to hematogenous dissemination of infection with damage to individual organs and systems of the body [4, 5, 7, 10]. Carrying out only conservative treatment for odontogenic sinusitis caused by the removal of filling material in the maxillary sinus does not ensure complete recovery of the patient; moreover, after physiotherapeutic procedures, most patients experienced increased pain and exacerbation of clinical manifestations [1, 3, 9].
In this regard, complex treatment of patients with this pathology is impossible without surgical removal of the root sealant [1, 3, 11] as soon as possible [2, 3], however, such an intervention is associated with surgical trauma.
A number of studies analyze clinical situations with different localization of filling material in the maxillary sinus - in the cavity, near the lower, medial walls of the sinus, in the lateral corner, in the area of the lower wall of the orbit. The nature of the foreign body, its localization, volume, prevalence, as well as the severity of pathological changes in the mucous membrane of the maxillary sinus, of course, require the selection of an adequate surgical technique and tactics for surgical access to the sinus [1, 4, 9].
Purpose of the study
A comparative study of the effectiveness of various methods for removing filling material from the maxillary sinus, including the use of endoscopic techniques, depending on the location of the root sealant in the sinus.
Material and research methods
A total of 72 patients were observed, including 27 men and 45 women, aged from 26 to 54 years, who had filling material in the maxillary sinus from 1 week to 18 months.
46 people (64%) presented with clinical manifestations of exacerbation of chronic maxillary sinusitis; 26 patients (36%) had no complaints during the initial examination, but a foreign body in the maxillary sinus was determined by x-ray. Clinical examination of patients began with a detailed X-ray examination. If necessary, computed tomography (CT) was performed, which made it possible to accurately determine the location and size of the foreign body located in the sinus.
Depending on the surgical technique used to remove filling material from the sinus, patients were divided into 2 groups. In the first group (52 patients), operations were performed using standard surgical instruments and a straight saw. In the second group (20 patients), endoscopic techniques were used.
The surgical intervention using standard surgical instruments was carried out according to a method described in sufficient detail in the literature [1, 3, 4, 9, 11], and is a modification of the Caldwell-Luke operation, the essence of which is as follows: appropriate conduction anesthesia is performed, then an arcuate incision is made in the mucous membrane and periosteum from the canine to the molars (Fig. 1), after partial peeling of the mucoperiosteal flap using a straight saw, a bone window is formed in the anterior wall of the maxillary sinus, over which the mucosa and periosteum are preserved. A window measuring 1.5x1.5 cm is cut out at an angle of 45?. After opening the sinus, the filling material and polyposis-altered mucosa are removed (Fig. 2).
Rice. 1. Detachment of the mucoperiosteal flap, preserving the periosteum and soft tissues (drawing by the authors). Rice. 2. Filling material in the sinus (drawing by the authors).
Then the bone fragment with the periosteum and soft tissues attached to it is returned to its place and fixed with a 5.0 vicryl suture (Fig. 3, 4).
Rice. 3. The bone window is fixed with sutures (drawing by the authors). Rice. 4. The wound is sutured (drawing by the authors).
Depending on the changes in the sinus mucosa, a “gentle” or “radical” maxillary sinusotomy was performed with mandatory complete (under X-ray control) removal of the filling material. 33 and 19 patients were operated on using the “gentle” and “radical” maxillary sinusotomy methods, respectively. Then, over the course of a week, all patients were prescribed 5-7 sessions of physical therapy using the Optodan laser device. By the end of the week, the stitches were removed.
Research results
When performing an X-ray examination, the accumulations of filling material brought into the maxillary sinus had a different appearance: single, clearly defined round intense shadows, many round shadows, clusters of irregularly shaped bodies of various sizes. The localization of these shadows was different, they were detected near the roots of the “causal” teeth and the bottom of the maxillary sinus in 35% of cases, and in 65% of cases they were located in the projection of the roots of neighboring teeth, in the upper medial corner or center of the sinus, and also near the orbital stack.
The main indication for the use of endoscopic technology was the short period of time the foreign body was in the sinus and the absence of pronounced changes in the sinus mucosa. According to the patients, the removal of filling material into the maxillary sinus was initially not accompanied by any symptoms. Painful sensations characteristic of exacerbation of odontogenic sinusitis appeared within 3 months. up to 1 year. It should be noted that in most patients the first clinical signs of the disease were diagnosed after suffering from acute respiratory viral infection. Patients noted a feeling of heaviness, discomfort in the affected sinus area, impaired sense of smell and nasal breathing, unilateral nasal congestion, pain of varying severity, radiating to the teeth and zygomatic area.
In all these patients, the foreign body and altered areas of the mucous membrane, which were mainly hyperplastic in nature, were removed. The length of the process depended on the length of time the filling material was in the sinus. When revising the sinus, the mucous membrane was preserved completely or individual polyps were excised without exposing the bone walls; sinus tamponade was not performed. In the postoperative period, in addition to traditional antibacterial and anti-inflammatory therapy, vasoconstrictor drugs were prescribed 3 times a day into the nasal passage on the side of the operated sinus, which ensured normal drainage and aeration of the sinus.
In 19 patients, changes in the sinus mucosa were of a diffuse polypous nature, and these patients underwent radical maxillary sinusotomy with the formation of an artificial anastomosis with the nasal cavity. Thus, such pronounced changes in the mucous membrane were observed in patients with a long-term presence of a foreign body in the sinus, even with a small amount of it.
The main indications for the use of endoscopic technology were short periods of presence of a foreign body in the sinus and the absence of pronounced changes in the sinus mucosa. Patients who used this method using endoscopic technology were also divided into two groups, depending on the access.
In the first group of patients, endoscopes were inserted into the sinus through the anterior wall of the sinus (Fig. 5). Eight patients were operated on using this method. In the second group of patients (12 patients), surgical access to the maxillary sinus was carried out through the natural opening in the middle meatus (Fig. 6).
Rice. 5. Maxillary sinusoscopy using endoscopic technology (drawing by the authors). Rice. 6. Endoscopic endonasal maxillary sinusoscopy (drawing by the authors).
This access is more physiological, as it allows to reduce the amount of surgical trauma to a minimum, preserve the “causal” tooth, provide conditions for normalizing the functions of mucociliary clearance into the nasal cavity, and reduce the rehabilitation period of patients by 30% compared to patients of the first group. In the postoperative period, the maxillary sinus was washed daily through the drainage with a Miramistin solution.
During endonasal intervention, correction of intranasal structures and endoscopic monitoring of the condition of the operated area were performed (Fig. 7-8).
Rice. 7. Endoscopic view of the endonasal approach to the maxillary sinus (drawing by the authors). Rice. 8. Correction of intranasal structures and endoscopic monitoring of the condition of the operated area (drawing by the authors).
Complex therapeutic treatment included the use of desensitizing, intranasal vasoconstrictor and non-steroidal anti-inflammatory drugs. The effectiveness of the methods was assessed according to the following criteria: removal of all filling material from the maxillary sinus, absence of complications and relapses of the disease in the postoperative period at regular intervals.
conclusions
As the research results have shown, all the methods used make it possible to completely remove the filling material from the maxillary sinus. However, it is necessary to clearly differentiate the tactics of surgical intervention, based on the results of radiography and CT scans based on the location of the foreign body in the maxillary sinus and the condition of its mucous membrane, with the involvement of otorhinolaryngologists.
In case of total disruption of pneumatization of the maxillary sinus, signs of blockage of the natural anastomosis with the nasal cavity and disruption of nasal breathing functions, after removal of the filling material, the tactics of endonasal maxillary sinus are indicated with the restoration of natural communication and ventilation of the maxillary sinus through the nose.
The list of references is in the editorial office.
Symptoms of sinus injury
The doctor can immediately determine perforation of the sinus during implantation by the following signs:
- failure of the instrument or titanium rod during its advancement;
- a sharp change in the position of the instrument in the hole formed for the implant;
- bleeding with the inclusion of air bubbles.
If the implant pierces the maxillary cavity, and the doctor does not detect the problem in time, it will go into a chronic stage and will be aggravated by additional symptoms that the patient cannot help but notice:
- sharp pain in the sinus area, radiating to the temples and eyes;
- swelling of the face on the side of the implanted tooth;
- runny nose, difficulty in nasal breathing;
- feeling of heaviness in the nose, discharge mixed with blood and pus;
- deterioration in general health, lethargy, increased body temperature.
If these symptoms appear, you should immediately contact the clinic. Otherwise, the situation will become more complicated, a fistula will form in the bone and gum, which will lead to speech impairment, liquid and food getting into the nose.
Related articles:
- Implantation guarantees
- Our advantages
- Press about us
How is it diagnosed?
- Probing the hole . It involves inserting a special thin probe into the hole for the implant to visualize the presence or absence of the bone bottom. If there is perforation, the probe moves inside without hindrance
- X-ray. It is carried out to fix the accumulation of blood in the sinus (darkened areas in the picture), the presence of fragments of dental roots or implants, and remnants of filling material.
- CT scan. Allows you to obtain the most accurate information about the presence of foreign bodies in the sinus and determine the exact location of perforation.
- Blood test. It is prescribed in advanced cases in order to assess the negative consequences for the body as a whole.
Diagnostics and its features
The most effective way to make a correct diagnosis is computed tomography, but this does not exclude the use of other, more traditional methods:
- conducting a patient interview;
- use of rhinotherapy to study the maxillary sinus;
- X-ray examination;
- MRI;
- puncture of the maxillary sinus.
An experienced doctor can reliably assume the presence of such a disease, but it can be confirmed using computed tomography.
What to do if perforation occurs
- If damage to the maxillary sinus is detected by a doctor during implantation, he will stop the bleeding, treat the perforated area of the mucous membrane with medications, apply sutures and cover it with a protective membrane. The decision on the possibility of further installation of the implant is made taking into account the degree of the defect and the reaction of the mucous membrane to the measures taken.
- If the implant fails and remains inside the sinus cavity, and the inflammation becomes chronic, the titanium root is removed, the sinus is opened and the affected tissue is removed. After surgery, the patient undergoes antibacterial and anti-inflammatory therapy.
- If the x-ray showed that part of the implant is in the sinus without damage to the mucosa, treatment is not carried out. This situation is not dangerous. Such a defect is diagnosed only by means of an x-ray when the implant is located in the sinus while maintaining the integrity of the mucosa
Interdisciplinary treatment plan development
This case requires the attention of both ENT specialists and dentists, since adjacent organs are affected. That is why Dial-Dent employs an ENT specialist, Andrey Valerievich Arkhandeev, who is not only well versed in the causes of ENT pathologies, having extensive knowledge and experience in the treatment of ear, nose and throat, but also has experience working with dentists, with the successful solution of complex interdisciplinary cases. Dial-Dent dentists, for their part, have experience in cooperation with ENT specialists, so patients are not driven from doctor to doctor, but develop a joint productive decision on treatment.
To develop treatment tactics, the ENT doctor held a consultation with an implant surgeon, endodontist and periodontist. The purpose of the consultation is to decide whether it is worth fighting to save the tooth, or to remove the tooth and replace it with an implant, and how to plan a joint operation if tooth extraction is unavoidable.
Endodontist's opinion
– teeth on the right side of the upper jaw for removal, since the prognosis for treatment is unfavorable, taking into account previous treatment, long-term chronic inflammation at the roots and the presence of a fistulous tract.
Periodontist's conclusion
– since conservative treatment has already been carried out, and inflammation continues, it is the removal of teeth that will help stop the development of periodontitis.
Conclusion of an implant surgeon
– tooth extraction will be combined in one operation with suturing of the fistula tract. Safe implantation of a tooth in place of the removed one is possible after complete restoration of bone and soft tissues, and elimination of inflammation in the sinus.
ENT conclusion
– surgery on the maxillary sinus to remove mycetoma will be performed through the sockets of the extracted teeth under the control of endoscopic equipment. After removal of the mycetoma, chronic sinusitis will be treated until the health of the maxillary sinus is completely restored.
How to prevent
Preventive actions on the part of the doctor include:
- thorough examination of the maxillofacial apparatus at the preparatory stage for implantation;
- correct selection of rod models;
- checking the condition of the nasal sinus membrane during sinus lifting and implantation.
From the patient's side:
- strict adherence to postoperative recommendations;
- extreme caution when blowing your nose and coughing;
- quitting smoking and drinking alcohol;
- elimination of pressure drops.
Sinusitis as a complication after dental implantation
Sinusitis is an inflammation of the sinus mucosa of infectious origin. With perforation of the maxillary sinus, the disease develops for the following reasons:
- Closure of the gap between the sinus and the nasal cavity due to particles of osteomaterial entering it during sinus lifting, developed swelling, or an incorrectly installed implant.
- Violation of sterility, infection of tissues during surgery.
- Poor-quality sanitation of the oral cavity at the preparatory stage for implantation, the spread of carious lesions.
- Damage to the cilia of the sinus mucosa, which are responsible for removing mucus. Violation of the outflow will lead to stagnation and proliferation of pathogenic microorganisms.
Among the reasons for the development of sinusitis without damage to the sinus:
- violation of nasal breathing;
- bacterial infection in the nasopharynx, which is accompanied by purulent discharge;
- chronic runny nose;
- advanced cold;
- lack of regular oral hygiene.
A joint operation performed by an implant surgeon and an ENT specialist at Dial-Dent
According to the conclusion of the consultation of doctors, it was decided to remove the teeth on the upper jaw on the right, remove the mycetoma from the maxillary sinus through the sockets of the removed teeth, and suture the fistulous tract. It was decided to carry out the operation under sedation – a state of medical sleep. Before the operation, the patient passed the necessary tests and had a consultation with an anesthesiologist.
A family dentist is licensed to provide treatment under anesthesia. Before the operation, the patient takes the necessary tests and undergoes examinations. When using any form of anesthesia (full general anesthesia or sedation), the patient is under the supervision of an anesthesiologist throughout the operation. There is a recovery room where you can rest after treatment.
In this case, the implant surgeon removed the problem teeth. Then the ENT specialist, under the control of an endoscope, removed the mycetoma from the maxillary sinus through the sockets of the extracted teeth. After removing the mycetoma, the surgeon sutured the fistulous tract.
Sinus lift - why do they lift the maxillary sinus?
In conditions of deficiency of bone tissue of the upper jaw, when implanting chewing teeth, a sinus lift is performed, which avoids perforation of the maxillary sinus and securely fixes the implant. The procedure is carried out using an open or closed method. The first is used for severe atrophy and involves complex surgical intervention. The second is less traumatic and is often performed simultaneously with implantation.
The open protocol includes the following steps:
- Introduction of anesthesia.
- Dissection and peeling of the gingival mucosa in the projection of the sinus.
- Formation of a lateral window in the alveolar process that opens inward.
- Raising the bottom of the maxillary sinus with a special tool.
- Filling the resulting void with bone material.
- Fixation of the barrier membrane.
- Stitching.
In this case, implantation is carried out after complete healing of the tissue (after 3-6 months).
The closed method includes:
- Anesthesia.
- Preparing the jawbone for a hole for a dental implant.
- Upward displacement of the bottom of the nasal sinus with a special instrument.
- Filling the resulting space with bone replacement material.
- Implant installation.
- Stitching.
- With extreme care (strictly according to its height), a hole for the implant is created in the bone.
- Using a special instrument, the bottom of the maxillary sinus is shifted upward.
- The resulting space is filled with bone material.
- The implant is fixed and the mucous membrane is sutured.
Neglecting a sinus lift before implantation of the upper chewing teeth can lead to the following consequences:
- further atrophy of the jaw bone;
- loosening of the titanium structure;
- migration of the implant into the maxillary sinus;
- rejection.
Make an appointment with an implantologist
Treatment procedure
Regulations for actions during treatment of a pathological condition:
- The foreign body must be removed; this is the main task of treatment.
- With such a lesion, inflammatory processes regularly develop. They are generated not only by filling material that has found its way into an unusual place, but also by oral microflora that has penetrated into the resulting hole or by swelling from inflammatory processes in the gums. They need to be cleaned.
- The patient needs to undergo treatment of both the maxillary cavities and the oral cavity, eliminating the causes of the disease.
Removal of a foreign body always occurs only through surgery. In this case, the cavity is penetrated through a hole and the object is directly removed. There are two such methods:
- laparoscopic;
- endoscopic.
The first method is more traditional. In this case, an incision is made between the upper lip and gum and the material is removed through the resulting hole. In the second case, the paranasal sinus is punctured in the place where the bone is thinnest and a foreign particle is captured through the resulting hole with a special tool and then brought out.
The operation is performed under local anesthesia and lasts no more than thirty minutes. The second method is most widespread. Laparoscopy is usually used in situations where, for some reason, endoscopy is not recommended.
After this, drug treatment of the inflammatory process is carried out. For this, immunostimulants or antibiotics, as well as other medications, can be used. Additionally, antibacterial solutions or an antiseptic are used to wash the damaged paranasal sinus.
Vitamin complexes are also used in treatment.
Implantation methods to bypass the sinuses
- Installation of ultra-short implants. It is used if there is sufficient bone density. Fixation of shortened implant models (up to 5 mm long) eliminates the risk of sinus perforation. However, such structures unevenly distribute the chewing load, which shortens their service life.
- Zygomatic implantation. Refers to protocols with immediate loading of the prosthesis. Provides for the implantation of titanium rods up to 60 mm long into the zygomatic bone. The operation is complex, risky, traumatic, and is performed under general anesthesia. Possible complications include: impaired mobility of the jaw joint, headaches, chronic sinusitis, decreased vision.
- Basal implantation. Allows you to avoid sinus lifting during bone resorption. Refers to protocols with immediate loading. It involves the implantation of special models of implants into the lower (basal) layer of the jaw bone, which is susceptible to atrophic processes. The advantages of the method include: rapid restoration of the functions and aesthetics of the dentition, minimal risk of rejection, and the possibility of combining it with tooth extraction. However, it should be taken into account that basal implantation began to be used recently, which entails a lack of long-term results. Its disadvantages also include: unsatisfactory aesthetics, the need for special equipment. Plus, not every doctor knows the technique of performing such an operation.
In our Center, the listed methods are not used due to the lack of guaranteed positive results confirmed by clinical studies. Implantation with preliminary sinus lift is a reliable, proven way to prevent perforation of the maxillary sinus during dental restoration by installing dental implants.