Painful sensations after treatment of pulpitis may be normal or a consequence of complications. In order to differentiate these conditions and determine whether it is worth seeing a doctor immediately, it is important to assess the nature of the pain, the time during which it persists, and general well-being.
It is worth noting that in most cases, one of the most important stages in the treatment of pulpitis is the removal of the pulp or neurovascular bundle of the tooth. Many patients wonder: can a tooth hurt after treating pulpitis with this method? Despite the absence of a “nerve”, pain may be observed, this is a natural reaction to the intervention - removal of the pulp, treatment and filling of the root canals. It is important to know when it is normal and when pain is caused by a complication.
Natural pain after pulpitis treatment
Why does a tooth hurt after pulpitis treatment if there are no complications?
After the anesthesia wears off, pain may appear in the area of the causative tooth, and normally this condition is characterized by the following symptoms:
- the pain gradually subsides - an unpleasant sensation of a certain degree of severity may persist for some time, but it does not intensify;
- already 1–3 days after the procedure, the pain noticeably subsides;
- there are no other symptoms - bleeding, severe swelling and redness of the gums, increased body temperature, general weakness.
It is difficult to predict how much a tooth hurts after treatment for pulpitis; it depends on the individual characteristics, the specific tooth and the complexity of the root system, the presence or absence of concomitant diseases. The norm is that moderate pain persists for up to 7 days. Important: the intensity of pain becomes less over time.
It is difficult to talk about the norm if there are such “indicators” of complications as fever, swelling, too much pain, including increasing pain. There are several possible complications of endodontic treatment of pulpitis.
Removing the filling material beyond the root apex
If, after treatment of pulpitis, the tooth hurts when pressed, perhaps we are talking about the removal of the filling material beyond the root of the tooth, into the adjacent tissues. The intensity of the sensation depends on how much material has gone beyond the apex of the root. Despite the fact that today a doctor has ample opportunities to control the accuracy of canal filling, as well as the use of high-quality materials, this can happen. It is worth noting that X-ray monitoring of treatment is intended to prevent the development of such a consequence - after the filling is completed, an image should be taken in which, in the event of a re-filling, the doctor will be able to notice excess material and choose the tactics for further action. Re-filling or removal of filling material beyond the root apex in itself does not pose a particular threat.
The exit of the filling material beyond the root apex can cause long-term pain immediately after the anesthetic wears off and persists for a long time - up to several months. This is a natural reaction of tissues to foreign material. Removal of material may be due to the following reasons:
- difficulties in determining the length of channels;
- incorrect selection of a pin from materials for the canal;
- lack of apical stop, etc.
However, this is not the only possible treatment difficulty that provokes pain.
Complication after root canal filling
Moderator: Lesya
Complication after root canal filling
Post by Tilda » Wed Aug 28, 2013 2:35 am
I would be very grateful for your help.
A short introduction. This is what I have at the age of thirty: seven teeth are pulpless and half-destroyed, two chewing side teeth have been removed, eleven living teeth have huge and not very filling fillings. Considering this not the most joyful situation, at some point I began to be cautious and immediately run to the doctor, having seen either the initial stage of caries of living teeth, or an alarm bell from pulpless teeth. I lost two teeth due to basal and interradicular inflammation of pulpless teeth. But unfortunately, my newfound habit of being cautious led to trouble.
Bottom dead "six". She didn't bother me at all. Never. But when I saw it in a panoramic photo, I was alarmed that I did not see the filling material in its roots. There was no hilar inflammation at all in the picture. The doctor advised not to touch it, since it doesn’t bother me. But I insisted. She asked me to remove the crown and fill the canals. I decided to play it safe, out of harm’s way. Taught by bitter experience.
This is where the problems started. The tops of the roots were filled and the tooth was prepared for the installation of a metal inlay. While the inlay was being made in the laboratory (within a week), I realized that something was clearly wrong with the tooth. At first, I began to clearly feel a pulsation in the area of this tooth. Then the aching pain joined the pulsation. The pain comes and goes. Obviously, something bad happened during the filling of the canals: either a perforation, or a crack, or an infection occurred (I’m not sure how possible this is), or something else. Of course, I refused to install the tab.
Here is a picture after the described intervention (there are three canals in the tooth, but only two are visible in the picture, unfortunately):
Please comment on the photo. There is inflammation, right? How strong? Do you see any perforations/cracks in the roots? What do you think about this filling itself? In my opinion, it looks somehow strange... I see that gutta-percha (or filling material) has extended beyond the root. I know this is not very good. Could this be the cause of inflammation? Although I have a couple of teeth with the filling material extending beyond the top of the roots. They have been standing like this for 3-4 years now and there are absolutely no problems with them.
The doctor said that she did not see the cause of the pain and did not know what could be done in this case. That, supposedly, it is no longer possible to get to the tops of the roots, because... they are sealed. She advised rinsing with saline solution.
To be honest, I’m not at all ready to lose this tooth. Is there really nothing that can be done? Can I perform an operation to remove the tip(s) of the root(s)? The doctor said that the roots of this tooth are abnormally short and can only get worse. What do you think about it? I bite my elbows: everything was fine. Yes, in the area of this tooth even before this intervention there was a slight loss of bone tissue (possibly due to many years of lack of load - two teeth above it are missing), but at least there was no inflammation or pain.
Olesya, please tell me the algorithm of actions. Where to run? How to save? Should I try to unseal the canals again to put anti-inflammatory medicine or antiseptic there? Or, if gutta-percha or filling material extends beyond the roots, then unfilling is impossible? I heard that there are special devices for unsealing canals. Perhaps such a device could help me?
Should I take an antibiotic? By the way, this is an idea
Almost four weeks have passed since the canal filling. The tooth hurts for three to four weeks. I expected him to calm down, but no. The pain doesn't stop.
Thank you very much in advance, with best regards, Sveta.
Insufficient canal filling
The opposite situation, in which a tooth may hurt after treatment of pulpitis, is insufficient filling of the root canals, the formation of voids at the apex of the root. In this case, often unpleasant sensations do not occur immediately, but as the inflammatory process develops - this can happen either after 1-2 weeks or after a longer period of time.
Here, painful sensations are associated with the proliferation of pathogenic microorganisms in the voids. This process leads to one of the diseases:
- periodontitis - inflammation of the peri-root tissues;
- tooth root apex cyst;
- granuloma.
Depending on the individual characteristics of the body, pain may appear immediately or make itself felt when the cyst or granuloma has reached an impressive size. Its intensity is often low, minor pain is more often observed when biting after treatment of pulpitis, and in the absence of mechanical impact on the tooth there is no discomfort at all.
Errors when filling
Endodontic treatment is a rather complex procedure. For successful implementation, you should remember three principles: proper processing, high-quality asepsis, reliable sealing.
At each stage, the doctor is capable of making a considerable number of mistakes:
Tooth perforation - in the absence of proper instrumentation and expansion, there is a risk of damaging the wall or bottom of the root canal. This happens, in most cases, due to a poor understanding of the anatomical structure of the roots and cavity of the tooth. Poor machining is the result of incorrect tool size selection. If the diameter of the file or reamer does not match the diameter of the canal, it can damage the apical foramen or leave an accumulation of dentinal filings on the walls.
Perforation of a tooth with a tool
Breakage of an endodontic instrument - this complication occurs when the technique and sequence of using files and reamers is violated, or when a blunt, damaged instrument is used. Breakage can occur during both manual and machine processing. To prevent this type of complication, the doctor should check all instruments before the appointment and make sure they are functional.
A piece of instrument in the channel
Incorrect expansion of the canal and its filling. To achieve high-quality obturation, the canal must be expanded to the optimal diameter. To avoid the formation of voids and further infection, the canal must be given a shape that is convenient for filling with material. Do not forget that canals filled with one paste will not have sufficient sealing, and over time, pores will form in the material.
One of the root canals was not processed
This is one of the rarest complications, since before starting endodontic treatment the doctor will definitely prescribe an x-ray diagnosis. It allows you to reliably determine the number of channels and evaluate their structure. But there are cases of abnormal location of root canals or their extremely small sizes, which makes them unnoticed in the image.
This leads to the following situation: the doctor removes the pulp in each canal, but one remains unattended - the inflamed pulp continues to hurt, and pathogenic bacteria continue to multiply. Such pain is difficult to confuse with other complications - the patient simply does not receive relief after treatment, and the pain characteristic of pulpitis itself remains. The sensations are pulsating in nature, the pain intensifies when eating, exposure to temperature on the tooth, and becomes unbearable at night.
The same symptoms can be observed with incomplete removal of the pulp in the diagnosed canal. In both cases, other symptoms may be observed:
- headache, sensations “radiate” to the ear, temple - depending on the specific tooth;
- increased body temperature;
- symptoms of general malaise.
Most complications are related to the complexity of the canal structure, and the following is no exception.
Instrument breakage in the root canal
After treatment of pulpitis, the tooth may also hurt due to a broken instrument. Part of it remains in the root canal, and unpleasant sensations occur immediately or a few days after the visit to the dental office.
The nature of the pain may vary depending on the size of the fragment and other conditions.
It is worth noting that this complication is quite rare. This is explained by the fact that a good dental clinic uses modern, high-quality instruments from reliable manufacturers that are sufficiently durable. In addition, the rules for their use must be strictly observed, including multiplicity, force during exposure, etc. And finally, the doctor will notice the presence of a foreign body in the tooth on a control image, which he will prescribe after treatment.
Features of the selection of filling material
To obtain the desired result when filling, the following factors should be taken into account:
- you need to use the best biocompatible material;
- it is necessary to follow the rules for treating the canal to avoid the spread of infection;
- Not only the main canal, but also its branches must be obturated;
- The filling material should not dissolve in the canal.
Not every material is suitable for such requirements. Until recently, root canals were filled with zinc-eugenol pastes, but this technique had its significant drawbacks. The paste did not allow filling all the branches of the canal, leaving voids. Thus, an infectious process developed inside her, which spread to the periodontal system. In addition, the paste had significant shrinkage, which meant that the root formation would have to be re-treated over time.
To find a suitable material for high-quality obturation, doctors put forward several requirements.
The filling material must:
- be completely biocompatible;
- do not have excessive shrinkage;
- have a bacteriostatic effect;
- be resistant to various types of liquids;
- give good adhesion to tooth tissues;
- create conditions for hermetic sealing;
- be X-ray contrastable;
- easy to remove from the canal cavity (if necessary).
Today, several types of materials are used for filling root formations: root-hardening cements, plastic materials (gutta-percha) and metal pins.
Pain after filling may be due to improperly treated canals
Due to the fact that an ideal material does not exist today, the combined use of pins and pastes is accepted.
Root perforation
Perforation is the creation of an artificial root hole. As a rule, in this case, the pain is sharp, unbearable and makes itself felt immediately after the anesthetic stops working. This can happen during instrumental processing of canals - preparing them for filling.
As in most other cases, the structure of the root system plays an important role here. Narrow, curved canals are a common cause of perforation. In this case, the tool does not move along the canal, but into the root wall.
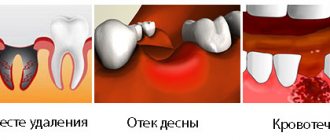
If a tooth hurts for this reason after treatment of pulpitis, the symptom may be accompanied by bleeding. In addition, some patients report pain even with current anesthesia - subjectively it is perceived as the feeling of an injection into the gums. If the tooth was filled after perforation, the filling material may leak beyond the root. Severe pain persists for up to 3 weeks, and the main complication of this phenomenon is the inflammatory process.
Allergy
This complication of pulpitis treatment is easier to differentiate - an allergic reaction is often accompanied by tissue swelling. If it is a consequence of material moving outside the root canal, there may be swelling of the gums around the treated tooth. In some cases, it spreads to other areas - cheek, lip, depending on the specific tooth.
When pressure is applied, the pain becomes stronger, it is difficult to relieve with painkillers, and over time it only intensifies.
What to do if the filling material goes beyond the canal
Due to the inexperience or inattentive work of the doctor, it happens that the filling material goes beyond the canal. The doctor must decide what to do in such a situation based on the complications that have developed. Most likely, this will be an opening of the channel.
If during treatment all the rules for medicinal and instrumental treatment of root formations were followed, then the risk of infection is quite low, and the patient will not be bothered by pain after filling.
If there is excessive removal of material and penetration of microbial organisms, the patient will have to undergo repeated treatment.
To do this, the canal is opened, washed with an antiseptic solution, and then the medicine is placed in it. If severe consequences of the initial treatment are observed, then surgical help cannot be avoided.
What to do?
What to do if your tooth hurts after pulpitis treatment? The most important recommendation if you suspect a complication after treatment of pulpitis is a return visit to the doctor. If this is not possible, you should contact another specialist and explain the situation.
If it is not possible to visit the clinic immediately, you can use a painkiller - give preference to the one that you have already taken, to which there have been no negative reactions. However, it is better to try to consult with a specialist, if not in person, then by phone.
It is difficult to say exactly how quickly the pain will subside in each case. However, on average, after visiting the dentist, relief comes quite quickly:
- When removing the filling material beyond the root apex: a visit to the doctor will allow the specialist to remove excess material, and after 2-3 days the discomfort will subside.
- If the filling is insufficient: the doctor will choose a tactic for further treatment; it is quite possible that several visits will be needed to eliminate the inflammatory process - for larger cysts or granulomas, surgical treatment is also required. This complication requires refilling to prevent recurrent complications.
- If the pulp or part of it is intact: the doctor will remove the remaining pulp and repeat the manipulations that were required to treat pulpitis. The pain in this case goes away within a few days after all measures are completed.
- If an instrument breaks off: the doctor will perform an X-ray diagnostic and, if the presence of a broken instrument is confirmed, will remove it. In rare cases, resection of the root apex is performed.
- In case of perforation: the dentist will treat the canals without affecting the hole. Using modern osteoplastic materials, he will close it, which will save the tooth. If a purulent process occurs, several visits will be required to eliminate the inflammation.
- In case of gum injury: contacting a doctor will allow you to receive recommendations regarding antiseptic and healing agents for treatment at home. Relief occurs on average within 1–3 days.
- In case of an allergic reaction: it will be necessary to refill the root canals using other materials. The doctor will perform the necessary manipulations and also prescribe decongestants that will quickly eliminate unpleasant symptoms.
Why does a tooth hurt after removing a nerve from a tooth?
Pain after treatment of pulpitis can be minor or acute. The appearance of pain can be associated with injury (to a lesser extent), but most often with the development of inflammation.
Trauma to tissues in the area of the apex of the tooth root –
Since the treatment involves the removal of the inflamed pulp (neurovascular bundle) and filling the root canals, it is quite reasonable that minor pain may occur due to the following:
- During the process of pulp removal, the neurovascular bundle is detached at the level of the apex of the tooth roots,
- Instrumental treatment of the root canals was performed. During this process, the tips of the instruments, extending slightly from the root canal beyond the root apex, can injure the tissue in the area of the root apex.
- The root canals were treated with medication by rinsing them with antiseptics. Antiseptic agents can enter in small quantities outside the root canals - into the tissue at the root apex. Because Since dentistry uses very strong antiseptics, they can actually have an irritating effect.
If the tooth was filled correctly, then the toothache after removal of the nerve lasts 1-3 days and disappears.
Poor quality root canal filling –
Poor quality treatment is indicated primarily by symptoms: pain, swelling of the gums. But very often inflammation can develop unnoticed, and then it can only be determined by an x-ray. There are several main signs of poor-quality root canal filling, which you can even independently determine from an x-ray after reading this article.
Signs of poor-quality root canal filling:
- Root canals are not filled to the root apex – Let us recall that pulpitis is an inflammation of the dental pulp associated with the ingress of microorganisms into it. During the process of pulp removal, canal expansion, and medicinal treatment, a certain amount of microflora in the canal, of course, remains. And if the canal is not filled up to the apex of the root or is poorly obturated with filling material (not tightly filled, there are pores), then the infection will multiply in its lumen throughout the unsealed section of the canal.
This infection will enter the tissue surrounding the tooth through an opening at the apex of the root. As a result, a so-called periodontal abscess (purulent sac) will appear at the root apex. This disease is called periodontitis.In Fig. 1-2 you can see radiographs of teeth after unsuccessful treatment of pulpitis. White arrows indicate unfilled areas of the root canals. Black arrows mark the areas where the periodontal abscess is localized (on an x-ray it looks like intense darkening at the root apex).
In Fig. 3 you can see how well-filled root canals should look on an x-ray. Black arrows show the places where the tops of the roots end (up to which the canal should be sealed).
What to do if the root canals are not filled to the root apex: it is necessary to completely re-treat the tooth, and the sooner the better, before inflammation at the root apex leads to tooth loss. To do this, you need to unfill the root canals and fill them again (24stoma.ru). There is also a surgical treatment method that can be used if the root canal is poorly sealed only at the very apex of the root, but the rest of the canal is well sealed. In this case, you can perform a resection of the apex of the tooth root. In this case, there is no need to remove the crown or unfill the canals.
- The filling material is brought out beyond the root apex – if during the process of filling root canals the filling material is removed beyond the apex of the root, this can also cause pain. In Fig. 4-5 you can see radiographs in which the filling material is clearly visible, extended beyond the root apex. The black arrows in Fig. 4-5 show the apexes of the roots (normally, the root canal is filled no further than this point). White arrows show the removed excess filling material (in Fig. 4 this is gutta-percha, and in Fig. 5 this is filling paste).
What to do if the root canals are filled: the issue is resolved individually. If a small amount of material is removed, the pain may subside quickly enough, and in this case there is no need to re-treat the tooth. In extreme cases, the tooth may hurt for up to 1-2 months. The decision about whether to wait two months for the pain to subside can be made based on the dynamics of pain. If the pain is not acute and it gradually decreases, then it is quite possible to do without re-treatment of the tooth.
If a large amount of material is removed, then surgical treatment may be required, which will also involve resection of the root apex. In this case, a hole is made in the bone in the projection of the tooth roots, through which excess filling material is removed. The operation is not very complicated, it lasts about 30-40 minutes.
- Breakage of an instrument in the root canal - during mechanical treatment of the root canal, or during the process of filling it - the instruments used for this may break in the root canal. In some cases it is possible to get them, in some cases, for example, if the tip of the instrument breaks in the apical third of the root, it is not possible to get such fragments. To a greater extent, this is the fault of doctors who violate the technique of using instruments. An exception may be cases where the root canals are severely curved. Naturally, such a fragment will not allow the root canal to be completely sealed, and this will lead to the proliferation of infection in the unsealed part of the canal and the subsequent development of inflammation in the tissues surrounding the tooth. In Fig. 6-8 you can see fragments of instruments in the root canals.
- Perforation of the tooth root – in the process of instrumentation of root canals and screwing pins into them, perforation may occur. Perforation is a “non-physiological hole” in the root wall, which is made by a doctor (Fig. 11). Perforations are one of the most difficult problems in dentistry. Their occurrence is most often associated with medical negligence. But sometimes they arise for objective reasons, for example, when the root canals are excessively curved.
In Fig. 9-10 you can see radiographs that show perforations of the tooth root that were made when installing pins in the root canals. The root canals are straight and not curved, which suggests that in both cases this was an illiterate work of the doctor. In both cases, the pins are inserted through the root wall directly into the bone tissue. In both images, intense shading (limited by black arrows) can be seen in the area of perforations, which indicates the development of a periodontal abscess.Perforations can be predictable when working in highly curved, narrow, difficult to navigate root canals. In this case, it is sometimes almost impossible to perform high-quality instrumental processing of such channels. And this sometimes happens even to very good doctors. But when the channels are “statistically average”, then the occurrence of perforation is associated, as a rule, only with a doctor’s error.
What to do in case of perforations: this pathology is very difficult to correct. To close perforations, special expensive materials are used, for example, Pro-Rut. If perforation occurs due to the fault of the doctor, the clinic is obliged to provide such treatment at its own expense. Filling with Pro-Ruth can be done in some cases both conservatively (from inside the tooth) and (in some cases) using surgical access to the perforation.
Read about quality standards in root canal filling in the article: → “Root canal filling standards”
What not to do?
If, after treatment, a tooth hurts when pressed or without mechanical action, you should under no circumstances resort to folk remedies such as heating, hot compresses, heating pads - if there is an inflammatory process, this can greatly worsen the condition. In case of allergic reactions, heat will also increase swelling.
It is also not recommended to use folk remedies for rinsing, which can cause a burn to the mucous membrane - iodine, tinctures of alcohol or vodka, liquids with the juice of “scorching” plants, etc. Even if there is no gum damage, such measures can worsen the situation.
It is also not worth taking various painkillers uncontrollably - firstly, you need to see a doctor in any case, and the effect of analgesics will not allow you to fully evaluate the clinical picture. Secondly, it can be dangerous to health.
It is important to visit a doctor at the first opportunity and perform all the necessary procedures to eliminate unpleasant consequences and improve the condition.