Infiltration anesthesia is a type of local anesthesia. Patients often call it “freezing.” This method is most often used for drilling carious tissues and treating root canals and removing teeth.
Unlike other types of local anesthesia, infiltration acts almost immediately; anesthetics are used in concentrations that are safer for health and are eliminated from the body quickly.
What is infiltration anesthesia
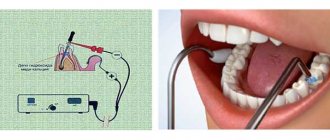
Infiltration anesthesia is a technique that involves the introduction of an anesthetic agent into the skin or mucous membrane in order to block nerve impulses.
In this case, the duration of action of the drug is determined quite accurately. This type of anesthesia is known to clients of dental clinics more commonly as “freezing”. The principle of infiltration anesthesia is to suppress the impulse transmitted from the pulp to the brain. As a result, the patient becomes numb in some parts of the face or mouth (cheek, lip or tongue), which depends on where the anesthetic is administered. As the components of the drug are broken down in tissue cells, sensitivity returns. The recovery process is completely controlled by a doctor.
Differences from other types of pain relief are the immediate effect after administration, the exact time of pain blocking, as well as the rapid removal of active components from the human body. An important factor is the safety of the drugs used, which is due to the low concentration of active substances.
Indications
In modern dental clinics, such anesthesia is used in the following cases:
- Removal of a tooth or row of teeth;
- For an additional anesthetic effect on the vestibular surface after mandibular anesthesia;
- To open purulent foci on the upper jaw;
- For the removal of fixed primary teeth on the upper and lower jaw in children under 8 years of age;
- When removing formations on the mucous membrane of the oral cavity and on the skin;
- For suturing wounds.
Advantages
The infiltration anesthesia method has a number of features that distinguish it from its analogues:
- Simplicity of the technique (no need to observe anatomical orientation).
- Safety (the minimum concentration of the drug can be used).
- Rapid relief of sensitivity of nerve fibers and soft tissues.
Areas of application
An indicator of the effectiveness of anesthesia is blanching of the mucous membrane of the alveolar process.
The scope of application of infiltration anesthesia affects all areas of medicine:
- surgery;
- dentistry;
- urology;
- proctology;
- gynecology;
- traumatology;
- gastroenterology;
- ophthalmology, etc.
This method of pain relief is often used in solving dental problems and in maxillofacial surgery due to a combination of factors that are important for the patient - effectiveness, safety.
Dentistry
The infiltration method is highly valued by dentists due to the operating principle of the anesthetic, which relieves not pain, but the impulse that comes from the pulp.
The drug chosen for the procedure is injected into the tissue, after which it is distributed among the cells. As a result, nervous activity is stopped. The duration of the analgesic effect lasts for one hour.
Jaw surgery
“Lemon peel” with local infiltration anesthesia.
The operated area on the face is injected with a weakly concentrated solution of Novocaine or another drug to create a so-called “lemon peel”, after which a dissection is performed. The patient does not experience any unpleasant symptoms.
Before anesthesia, the body's reaction to the active components of the anesthetic is studied to prevent allergies.
Equally important is compliance with the drug administration technique and dosage calculation.
Release forms
Preparations for topical anesthesia are available in different forms, each of which has advantages for use on a specific area of the skin or mucous membrane. To solve dental problems, gel is considered the most optimal option, since it is more resistant to being washed off by saliva.
In addition to the gel, the following products are available on the market:
- ointments;
- solution (alcohol/water);
- cream;
- spray;
- aerosol;
- powder;
- lozenges;
- film plate.
Before using any product, you must read the instructions for use to avoid side effects resulting from an overdose.
Techniques
The tissue infiltration method is widely used in surgery, with the exception of particularly complex cases that require a longer period of pain relief. There are several ways to perform the procedure:
- under the skin;
- under the mucous membrane;
- to the periosteum area.
According to the method of drug administration, infiltration anesthesia is of two types:
- direct – local anesthetic is injected into the operated area;
- indirect - the drug is administered throughout the adjacent area, with the active components penetrating into the deep layers of tissue (the method is based on diffusion).
Types of infiltration anesthesia in dentistry
In medicine, infiltration methods of pain relief are divided into several types. The main feature of the classification is the area of influence of the drug used.
| Types of infiltration anesthesia | |
| Name | Description |
| Intrapapillary (periosteal, submucosal) | The injection is carried out under the mucous membrane into the papilla of the tooth with a needle depth of up to 3 mm. |
| Spongy intraseptal | The injection is given into the septum located between the incisors. Pain relief occurs instantly, the nerve fibers of bone and soft tissue are reliably blocked from impulses, which makes it possible to perform operations on the gums, remove tumors in the mouth, and perform dental treatment. |
| Intraligamentary | It is used to solve various dental problems, except for cases with purulent formation. The drug is injected between the tooth root and the jaw bone, the anesthetic takes effect after 15-45 seconds, the effect lasts up to 30 minutes. The advantages of this type: no pain, low anesthetic consumption. |
| Intrapapillary | An anesthetic drug is injected into the papilla located between the teeth. It is impossible to achieve the desired effect with a single injection, so there is a need for an additional injection, which is administered from the palate to completely block the nerve fibers. |
| Intrapulpar | This method is additional; the injection is administered into the pulp after intraligamentous anesthesia. The thinnest needle is used for the procedure. |
| Subperiosteal (Subperiosteal) | The drug is administered with a syringe with a shortened needle, placing it between the gum and the base of the root (the control point is the border between the mobile and stationary parts of the mucosa). The amount of anesthetic used should be minimal, and the injection should be administered sharply. |
Other types
There are other methods of pain relief, the principle of action of which is also associated with tissue infiltration:
- “Block field” – appropriate to use in cases where the soft tissues of the jaw are inflamed;
- druk-anesthesia - placing a tampon treated with the drug into the hole resulting from the development of caries;
- plexual - injection into the plexuses of the alveoli (anterior and upper middle part);
- intrapapillary - the drug is injected into the base of the gum papillae located between the teeth.
Pain relief under pressure
When choosing a method of anesthesia under pressure, it is necessary to follow the rules for carrying out this manipulation.
First of all, it should be taken into account that the patient needs preliminary preparation, which includes a psychological component (an explanation of the essence of the manipulations and a conversation to calm the patient) and a medicinal one (an hour before the intervention, the patient is administered analgesic drugs, antihistamines, anxiolytics and other drugs).
After preliminary preparation of the patient has been carried out, the main stages of drug anesthesia are performed:
- A sterile cotton ball soaked in an anesthetic (for example, lidocaine) is placed at the bottom of the carious cavity.
- Then the cavity is pre-clogged with a heated thermoplastic mass, material for temporary fillings or a small piece of raw rubber.
- Using a plugger-trowel, the plug with the drug is gradually and carefully moved into the cavity.
This method of pain relief helps prevent sudden attacks of pain and promotes tight clogging of the cavity.
Thanks to this, the anesthetic under pressure has an infiltrating effect inside the tooth - the drug penetrates into the dental pulp through the dentinal tubules, and after 10-15 minutes the pain impulses disappear.
The effectiveness of this method increases in cases where the carious cavity has a central location. The method is especially effective in cases where the cavity is wide open for access.
It is worth noting that in some cases it is not possible to avoid leakage of anesthetic and a decrease in the effectiveness of anesthesia. This occurs in cases where the contact surface of the tooth is destroyed as a result of manipulation.
Infiltration anesthesia according to Vishnevsky
Anesthesia according to Vishnevsky
The method was developed by the famous surgeon A. V. Vishnevsky. In 1922, it was called “creeping infiltration”. The essence of the development is to combine two types of anesthesia: infiltration and conduction. The drug used ultimately blocks not only the receptors, but also the passage of impulses along the nerve endings located at the operated site.
Anesthesia according to Vishnevsky consists of the following stages:
- injection of the drug under the skin (with the capture of subcutaneous fatty tissue) to obtain a “lemon peel”;
- dissection of infiltrated tissues with a scalpel;
- injection of a syringe with an anesthetic into the fascial spaces in the operated area;
- injection of the drug into the muscles located in the area of manipulation.
An important point is compliance with the technology of drug administration and step-by-step dissection of the subcutaneous layers to achieve a dense creeping infiltrate.
Operating principle
Anesthesia under pressure, or druk-anesthesia , consists of infiltration penetration of an anesthetic drug into the dental tissue.
The mechanism of action is the tight fit of the tampon with an anesthetic to the dental tissues by installing a “plug”.
The drug gradually permeates the surrounding tissues, resulting in a fairly high stable analgesic effect.
The analgesic effect occurs within a few minutes and lasts up to half an hour, which is quite enough for therapeutic measures.
Intrapulpal injection anesthesia is the direct injection of an anesthetic into the pulp of the tooth through the resulting cavity. It also provides fast and stable pain relief results.
Application on the upper jaw
The upper part of the jaw has porous thin tissue; for infiltration anesthesia, this zone is preferable to the lower jaw. After administration, the anesthetic reaches the nerve fibers in a short period of time. Puncture sites are selected depending on the goals:
- to relieve the nerve endings of molars, a needle is placed between the causative tooth and the adjacent molar, the drug is applied to the base of the root;
- when treating incisors, a puncture is made into the transition fold, located slightly above the apex of the roots above the causative tooth;
- For pain relief on the palatal side, a puncture is made into the mucous membrane in the area of the incisor opening.
In the lower jaw, the infiltration method is used for anesthesia during short-term manipulations on soft tissues. If more serious interventions are planned, the anesthesia effect is achieved by combining several types of anesthesia. This approach is explained by the dense structure of the alveolar tissues and low porosity, which creates a certain barrier for the drug to penetrate the nerve bundle.
The anterior section of the lower jaw has the least dense part of the tissue due to micropores, therefore, when manipulating the incisors, the anesthetic is injected into the transitional fold, advancing the needle to the base of the root. To anesthetize all incisors, the needle is placed in the fold between the first incisors. After reaching the tip of the needle at the base of the root, the syringe is positioned horizontally, and when administering the drug, the needle is slowly moved towards the canine. The same procedure is performed on the other side of the lower jaw.
Tooth preparation
In order to choose the right method of anesthesia, it is necessary to carry out preliminary preparation of the tooth.
If during a visit to the doctor the patient experiences acute pain, the dentist immediately performs infiltration or conduction anesthesia to eliminate these sensations.
If at the time of the intervention the patient’s pain from inflammation has subsided, the dentist performs the following actions:
- Food debris is removed from the carious cavity.
- Using a dental bur, overhanging edges of hard tooth tissue are removed.
- The cavity with the affected area of the tooth is opened wide with the help of instruments so that the specialist has access to the localization of anesthesia.
- Using an excavator, softened dentin is removed from the bottom and side walls of the carious cavity.
- Remains of infected dentin are removed from the side walls using a sharp bur.
- The formed cavity is disinfected and dried with sterile cotton swabs and warm air.
Only after all these manipulations, based on the available data, does the dentist decide which method of anesthesia will be appropriate in a particular clinical case.
The main signs of initial pulpitis and the tactics of its treatment.
In this article we will talk about the features of treating dental cysts with depophoresis.
Read here about the effective treatment of dental phlegmon.
Infiltration anesthesia in children
Infiltration anesthesia is the preferred method in pediatric dentistry.
When choosing anesthesia for children, experts give preference to the infiltration technique. This is explained by the low concentration of the active substance in the drug used, as well as the thin porous bone tissue of the alveoli, which facilitates rapid absorption of the injection.
The effectiveness of the anesthetic is also influenced by a well-developed vascular network passing through the soft tissues and alveolar process.
In preschool children, the gingival papillae have a rather loose structure, therefore, when treating teeth, infiltration anesthesia is recommended to be administered from the edge of the gum. Dental tissues also lend themselves quite well to infiltration.
Dentists' opinions
Many dentists refuse to perform anesthesia in favor of injection methods. As the main arguments, they cite patient discomfort during the procedure and the risk of side effects, in particular infection.
According to skeptics, infectious agents enter the wound along with the anesthetic. However, some other experts, on the contrary, are inclined to believe that this method is highly safe with proper preparation for the procedure.
Today, dentistry has a sufficient amount of sterile materials and antibacterial drugs to prevent infection.
How it goes
Regardless of the area of application of infiltration anesthesia (on the skin or mucous membrane), manipulations are carried out according to the same technique:
- Treating the puncture area with an antiseptic drug.
- Convenient placement of the specialist in relation to the patient (on the right side of the client).
- Exposing the transitional fold of the patient's mouth by pulling back the cheek or lip. The specialist performs the action with his hands or using a special tool.
- Place the tip of the needle on the transitional fold, maintaining an inclination angle of 45° (relative to the alveolar ridge). The bevel of the needle should be directed towards the jawbone.
- Carefully insert the needle all the way into the bone tissue. The immersion depth can be 5-15 mm, depending on the jaw area.
- Inject the drug by applying gentle pressure with your finger on the syringe plunger.
Preparations and solutions
The following solutions are used for infiltration anesthesia:
- novocaine;
- lidocaine;
- bupivacaine;
- trimecaine;
- mepivacaine;
- naropina;
- ultracaine;
- articaine, etc.
When choosing a drug for local anesthesia using the tissue infiltration method, it is worth considering that only sterile solutions are suitable. Suitable anesthetics are those that dissolve well in water and are not destroyed during sterilization. The permissible concentration of active substances is 0.25-0.5%.
The needle parameters are determined depending on the objectives of anesthesia:
- length – 16-32 mm;
- diameter – 0.3-0.5 mm.
Quite rarely, needles with the following parameters are used for this type of anesthesia: length - 23 mm with an outer diameter of 0.8 mm; length – 32 mm with a diameter of 0.9 mm. When selecting an instrument, it is worth considering that small sizes reduce the risk of injection getting into the vessel.
Among modern instruments, syringes with the ability to fix the needle at an angle deserve attention. Thanks to this design, it is much easier to reach the desired point in a hard-to-reach place in the oral cavity.
Technique
- Direct - used in the treatment of root canals, gums, etc.;
- indirect - most often practiced when removing teeth.
With the direct technique, the injection is made directly into the tissue in the surgical area. Loss of pain sensitivity is achieved only in this area.
With indirect anesthesia, the anesthetic is distributed in layers: when making an injection, the doctor injects the medicine as the needle moves (deeper or along the surface). This way it gets into different layers of tissue and increases the area of pain relief.
In both cases, the injection is performed with a syringe with a carpule needle with a diameter of only 0.3 mm (twice as thin as a normal one) and is almost painless.
Preparation
First, the doctor finds out whether the patient has any contraindications to the procedure (allergy to the anesthetic). Then preliminary anesthesia is performed - superficial anesthesia at the injection site (gel or spray) or an anesthetic injection into the gum mucosa. When the gums are numb, infiltration anesthesia is performed directly.
Advantages and disadvantages
To evaluate the effectiveness of infiltration anesthesia, it is recommended to familiarize yourself with its advantages, which compare favorably with other options. For completeness, the table also shows the disadvantages of the tissue infiltration method.
| Infiltration anesthesia | |
| pros | Minuses |
| A safe method of pain relief due to the low concentration of the active substance in the preparations. | Limited scope. |
| Quick effect. | The duration of action of the drug is reduced when the pulp is anesthetized (the reason is the rate of resorption of the drug). |
| The active substances of the anesthetics used are eliminated from the body easily and quickly. | Inability to fully use in areas located in the lower part of the jaw. |
| Longer effect of the drug than when using surface anesthesia. | A bitter taste appears in the mouth due to the spread of the drug beyond the anesthesia zone. |
| An analgesic effect is achieved not only on the desired nerve, but also on the endings of neighboring nerves. | |
| A simple anesthesia technique that does not require deep anatomical knowledge. | |
Precautions and possible complications
One of the possible complications is traumatic neuritis of the facial nerve.
Despite the wide range of applications of infiltration anesthesia, the method can provoke serious consequences:
- hematoma as a result of damage to a vessel by a needle;
- rupture of dental ligaments or tooth deviation due to rapid administration of the drug (the rate of drug administration is 1 ml/15 seconds);
- injury to the nerve trunk, resulting in the development of traumatic neuritis;
- injury to the periosteum, followed by pain and swelling;
- infection due to the use of insufficiently sterile instruments;
- injury to muscle tissue located in the infratemporal fossa;
- blockade of the nerve fibers of the face (the condition is temporary, goes away on its own after a few hours, is recognized by a drooping upper lip and the absence of eye reflexes);
- intoxication of the body due to exceeding the dose or introducing the drug into a blood vessel;
- allergic reaction (redness of the mucous membrane, swelling, difficulty breathing).
To prevent the development of complications, you need to follow simple rules before using the infiltration technique:
- pre-test the drug to identify allergies;
- take a responsible approach to choosing a clinic and specialist; a needle in the hands of an inexperienced or incompetent doctor can cause a lot of problems;
- administer the dosage specified in the instructions; if the drug does not give the desired effect, you need to replace it with another anesthetic drug;
- familiarize yourself with contraindications to the drug and type of anesthesia;
- When administering the product, maintain a calm position so as not to cause injury to soft tissues;
- if the patient is nervous at the sight of a needle, then application anesthesia can be used first.
To prevent the needle from entering a large vessel, the specialist pulls the syringe plunger towards himself when puncturing. The appearance of blood indicates an error. In this case, the needle moves slightly.
Gynecology and obstetrics
Gynecology, as an independent medical discipline, dates back only to the 19th century. At first it had a surgical focus. As medicine developed, new directions appeared in gynecology, in particular, such as genetics and human reproduction, contraception, infertility, family planning, sexology, and aging problems. Currently, gynecology covers both biological and, partially, social aspects of a woman’s life. In recent years, endoscopic surgery, gynecological endocrinology, assisted reproduction and in vitro fertilization, and reproductive immunology have been actively developing. Modern gynecology has become one of the most versatile and interesting specialties. In Russia, the first gynecological clinic was opened in 1842 at the St. Petersburg Medical and Surgical Academy. It was successfully led by A.A. Keeter (1813-1879), who wrote the first Russian “Guide to the Study of Women’s Diseases” [1858]. Being a famous surgeon, A.A. Keeter gave gynecology a surgical focus. He performed vaginal hysterectomy for the first time with a successful outcome. The development of domestic gynecology was successfully continued by A.Ya. Krassovsky (1821 - 1898). He became the founder of Russia's first Obstetrics and Gynecology Society in St. Petersburg (1886), and under his leadership the Journal of Obstetrics and Women's Diseases began to be published. AND I. Krassovsky performed the first successful oophorectomy in Russia. He is the founder of domestic operative gynecology. A prominent representative of the St. Petersburg Gynecological School was Professor D.O. Ott (1855-1929), head of the Midwifery Institute. BEFORE. Ott improved the technique of many gynecological operations; he designed new medical instruments for gynecological operations. He is the founder of endoscopic surgery in gynecology. A talented representative of the Moscow School of Gynecologists was V.F. Snegirev (1848-1916), who founded the gynecological clinic of Moscow University (1889), the gynecological institute for advanced training of doctors (1896) and the Moscow Obstetrics and Gynecology Society (1887). V.F. Snegirev developed a number of new gynecological operations. His monograph “Uterine Bleeding,” which was reprinted several times, was a gynecological encyclopedia of that time. It has not lost its significance in modern conditions. V.F. Snegirev was a brilliant surgeon; he was recognized as a major specialist not only in our country, but also in Europe. Understanding the need to study the physiological and pathological conditions of the female body, he was one of the first to come to the conclusion that only the surgical direction in gynecology is certain. The study of functional disorders, as V.F. believed. Snegirev, can help prevent a number of gynecological diseases leading to the need for surgical treatment. A major representative of the Moscow School of Gynecologists was A.P. Gubarev (1855-1931). His work on the study of pelvic tissue, carried out under the guidance of V.F. Snegirev, played a big role in improving surgical operations. For the first time in Russia, he performed radical surgery for uterine cancer, removed regional lymph nodes for vulvar cancer, and developed extraperitoneal approaches for the surgical treatment of pelvic abscesses. A.P. Gubarev is the author of the manuals “Operative gynecology and the basics of abdominal surgery”, “Medical gynecology or gynecology of a practical doctor”. The Kazan school of gynecologists is represented by BC Gruzdev (1866-1938). He was especially involved in the study of benign and malignant tumors of the female genital organs, as a result of which the monograph “Ovarian Sarcoma” was written. BC Gruzdev is considered the founder of gynecological oncology. According to tradition, obstetrics and gynecology are a single specialty dedicated to protecting women's health. This unity is especially clearly represented in the activities of our contemporaries - M.S. Malinovsky (1880-1976) and L.S. Persianinova (1908-1978). Both are outstanding scientists and organizers of obstetrics and gynecology. M.S. Malinovsky founded and headed the Research Institute of Obstetrics and Gynecology for many years. Organized in 1944, the institute was subsequently the first scientific institution of the country’s Academy of Medical Sciences, and M.S. Malinovsky was elected its vice-president. Under the leadership of M.S. Malinovsky, gynecology moved from the morphological to the functional direction, gynecological endocrinology actively developed, and research began on the immunology of reproduction. L.S. Persianinov headed the departments of Moscow universities and was the director of the Institute of Obstetrics and Gynecology of the Ministry of Health of the Russian Federation. Being a brilliant surgeon, he improved the technique of many planned and urgent gynecological operations. L.S. Persianinov is one of the founders of the use of cybernetic research methods in gynecology. Dramatic changes in gynecology began with the rapid development of gynecological endocrinology in the 50s. XX century Biological methods for determining steroid hormones have been replaced by radioimmunological and immunochemical methods. Synthetic estrogens and gestagens, hormonal contraceptives, and gonadotropins were synthesized. The use of gonadotropins, along with the successful treatment of endocrine infertility, has made it possible to carry out drug-induced superovulation. In this case, several follicles mature in the ovaries at the same time. Each of them contains an oocyte, which is extracted by puncture from the ovaries and fertilized in an artificial environment. This technique of in vitro fertilization has been widely developed, which is to a certain extent associated with the development and application of new imaging methods in medicine. Ultrasound research methods make it possible to monitor the maturation of oocytes and puncture follicles under ultrasound control for in vitro fertilization. At the end of the 20th century. a technique for fertilizing an egg with one sperm and using donor oocytes has appeared; preimplantation diagnostics have been developed to prevent fertilization with defective gametes. Micromanipulation techniques with oocytes have made it possible to create the basis for medical cloning and obtaining stem cells from human and animal blastocysts. Knowledge in embryology and genetics of reproduction has advanced significantly. Assisted reproductive technologies can solve many issues in the treatment of infertility. At the present stage of development of civilization, problems have arisen that previously did not have such relevance. The number of patients with sexually transmitted infections has sharply increased, and infections that are dangerous not only for reproductive function, but also for life, such as HIV, hepatitis B and C, have developed. Unregulated sexual behavior, called the “sexual revolution,” has become the subject of study not only in sexopathology as a new science, but also in sexology as part of gynecology. If sexopathology is designed to help the sick, then sexology is designed to help healthy women and married couples rationally build family relationships. Our society, and with it domestic gynecology, is undergoing a difficult and controversial development of the process of family planning, contraception and abortion prevention. For many years, the interests of the family were subordinated to declarative state interests. Neglect of contraceptive methods has led to the spread of abortion as a method of family planning. The large number of abortions forces us to pay special attention to the development and implementation of contraception in our country, while the training of gynecologists and their active position become essential. The first report of the successful use of oral contraceptives dates back to 1956. The further development of “contraceptive pills” led to a significant reduction in the dose of hormonal ingredients in them; with skillful use, contraceptives became harmless. The synthesis of new gestagens, along with reliable contraception and safety, allows the use of hormonal contraceptives as therapeutic drugs for regulating the menstrual cycle, treating hyperplastic processes in the endometrium, ovaries, etc. Modern intrauterine contraceptives reliably prevent the onset of unwanted pregnancy, are convenient to use, and are characterized by a small number complications. At the end of the 20th century. Combined contraceptives have appeared, combining the properties of hormonal and intrauterine devices. Barrier methods of preventing pregnancy are being improved. Emergency contraception has become widespread. The last decades of the 20th century. in gynecology were marked by the rapid development of minimally invasive endoscopic surgery. The development of portable video systems and the transmission of images to a monitor screen have made it possible to move surgery out of the “keyhole” to a wide view with the possibility of enlarging the objects of surgical intervention. Endoscopic surgery uses lasers, power tools, cutting equipment, and modern suture material. The advantages of endoscopic operations are their low invasiveness, the possibility of preserving reproductive function, and dynamic monitoring of the recovery process after surgery. Along with endoscopic surgery in gynecology, the development of traditional methods of surgical treatment continues with the use of modern suture materials, antibiotics, and medical rehabilitation in the postoperative period. For many gynecological diseases, vaginal access is widely used. With traditional approaches, predominantly organ-preserving operations are performed. In recent years, much attention has been given to preserving the health of women during perimenopause and after the end of menstruation. The pathogenesis of menopausal and postmenopausal syndromes has been studied. Hormone replacement and alternative therapy for estrogen deficiency, prevention of osteoporosis, etc. have been developed. Precancerous diseases of the female genital organs are being actively studied, prevention and active therapy are being developed in risk groups. In the near future, genetics, immunogenetics, and cellular technologies will take a leading place in gynecology.