In this material we will try to discuss how to prepare for wisdom tooth removal, basic recommendations, what is and is not possible before wisdom tooth removal, the postoperative period and possible consequences.
All this will help you prepare mentally and make it easier to endure the operation itself.
- When is it better to delete
- What you can do before tooth extraction
- What not to do before tooth extraction
- Recommendation before tooth extraction
- Recommendations after tooth extraction
- Postoperative period and possible consequences
Remember, you are the one who makes the decision to preserve or remove a tooth; if you don’t understand something, ask questions and don’t be shy with the doctors, because you are also responsible for the decision.
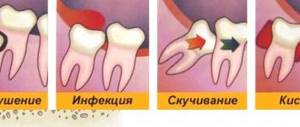
Removal of wisdom teeth due to caries
Why are wisdom teeth most often affected by caries?
Most often, caries of wisdom teeth develops due to the fact that they are located far enough away and do not participate in the act of chewing.
And if the teeth are not involved in the act of chewing, then it is extremely difficult to clean them due to the fact that the teeth are cleaned not only during hygiene, but also during each meal - on their own. On the picture
– what caries looks like on the bottom eight.
You can see how the lower wisdom tooth is removed due to caries HERE. By the way, there, in clinical cases, you can see how the removal of an upper wisdom tooth occurs.
Often the patients themselves neglect these teeth, brush the eights less carefully and caries develops quite quickly, the wisdom tooth begins to hurt, so it will be easier to remove such a tooth than to treat it.
Can caries cause wisdom tooth removal?
Should wisdom teeth with caries be removed? Yes. Removal of the figure eight, if there is caries, is carried out due to the inappropriateness of its treatment.
In most cases, we do not chew with these teeth, and treating wisdom teeth is quite difficult and problematic. And most importantly, this makes absolutely no sense.
Removing the bottom eight can be seen HERE
There is also a situation when the wisdom tooth is strongly inclined, “lying” and covered with caries. In this case, there is also absolutely no point in treating wisdom teeth.
.
If your wisdom tooth gets injured: chipped or cracked?
Should it be removed? A chip, crack, or injury to a wisdom tooth is a 100% indication for removal
wisdom tooth There is absolutely no reason to fight to save him.
The most frequently asked questions from our patients
What happens if the tooth root is left in the gum?
If the root of the tooth is left as is, it becomes a source of infection, and after some time serious complications may develop, for example:
- inflammation of the tissues surrounding the tooth, including bone;
- penetration of infection into the wound surface;
- periodontal disease.
What is a root canal and can it be treated rather than removed?
The root (or dental) canal is an anatomical space inside the root of a tooth filled with pulp. Cleaning and treatment of dental canals is a mandatory stage of dental fillings and prosthetics. In our clinic, for this purpose, we use self-adapting files of the SAF system, which carefully clean the canals from dead and diseased tissue, pus, and accumulations of bacteria, without injuring healthy areas of the tooth. Thanks to their hollow structure, the doctor can simultaneously treat the root canal with disinfectants and anti-inflammatory drugs. Root canals are preserved only if the tissues surrounding the tooth are not affected by pathological processes, and in the future the root can be used for prosthetics.
If the tooth can still be restored, root canal treatment (roots) of the tooth is performed. It can be successfully completed in our Moscow clinic.
Wisdom teeth during orthodontic treatment
Removal of wisdom teeth before orthodontic treatment
During the period of orthodontic treatment, when the bite is being corrected, the figure eights are also most often removed. Why?
Before orthodontic treatment, we need to remove teeth that are preventing all the remaining teeth - 28 teeth - from moving into place. As a rule, wisdom teeth do not provide freedom for such activities. We remove them and then perform orthodontic treatment.
In what cases are wisdom teeth not removed during orthodontic treatment?
In the case of large jaws, when the wisdom teeth are in an absolute row and they close correctly, in the correct occlusion, we do not need to remove them. We can leave them, we can also treat them, take care of them, like other teeth.
Treatment methods
Treatment of pathological tooth wear may include therapeutic and orthopedic techniques. In the first case, there are two options:
- Drug therapy (includes the application of gels and solutions, the use of special toothpaste).
- Restoration (special filling material is used).
Orthopedic treatment involves the manufacture and installation of onlays, dentures or crowns, which restore the normal appearance and functionality of teeth.
Currently, dentists do not agree on the timing of initiation and specific treatment methods in different situations. Most often, drug treatment is used in patients in the early stages of the disease, when the teeth are not yet seriously damaged. For more severe pathology, restorative and orthopedic treatment is indicated.
Impacted and dystopic wisdom teeth
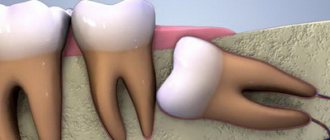
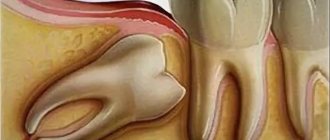
Impacted wisdom tooth
- this is a tooth that has not erupted; it is located in the bone tissue, in the gum. The general practice is that few dentists decide to remove an impacted figure eight, since it is a complex procedure.
In the clinics of the German Implantology Center, removal of impacted wisdom teeth is carried out as planned; our experience allows us to perform surgery of this level.
Why don't wisdom teeth erupt?
The wisdom tooth does not erupt due to the fact that it is dystopic: there is a neighboring tooth in front of it, which is in the way.
This wisdom tooth is usually tilted. Or there is absolutely no room in the jaw, it is located at the corner of the jaw: there is no place for it to cut through, there is no way.
Dystopic tooth
A wisdom tooth is a tooth that is erupting or has erupted incorrectly. Or it cannot erupt and occupies the wrong position in the jaw.
Typically, such teeth displace other teeth, deforming the jaw. It is impossible to treat them, and straightening them is also extremely difficult. In these cases, we remove the dystopic wisdom tooth. As a result of dystopia, cheek injuries may also occur due to chronic biting. Therefore, it is better not to postpone the removal of the dystopic eight “for later”.
Causes of pathological abrasion
There are several main reasons for the development of abrasion pathology, and in the first place among them are bad human habits. For example, the habit of gnawing seeds, holding small objects in the mouth (pins, cloves, pipe mouthpiece), love for foods with high acidity may well become catalysts for the process.
Often the cause of increased abrasion is diseases: bruxism, diseases of the gastrointestinal tract, nervous, cardiovascular, endocrine systems, from the side of the TMJ - malocclusion. The cause may also be improper dental treatment - an incorrectly manufactured orthopedic design can provoke severe abrasion of the antagonist tooth.
Sometimes the cause of pathology may be the chosen profession. Some employees of the metallurgical, cement, granite industries, and representatives of the mining workshop suffer from increased abrasion.
Removal of wisdom teeth in pregnant and lactating women
Removal of wisdom teeth in pregnant and nursing mothers
Is it possible to remove wisdom teeth during pregnancy? Pregnant and lactating women can have their wisdom teeth removed only in case of exacerbation of one of them or necessity, when it is impossible to solve this problem conservatively. In a planned manner, it is better to remove wisdom teeth after the end of the feeding period.
Are there any special features of removing wisdom teeth during pregnancy?
We try to perform tooth extraction on all our patients as carefully, comfortably, and carefully as possible. Therefore, as a rule, there are no technical features. But if any intervention in the form of wisdom tooth removal is urgently required (because there is no other alternative), we must consult with the attending physician - a gynecologist and, accordingly, coordinate all our actions.
What anesthesia is used when removing wisdom teeth in pregnant and lactating women?
In pregnant and lactating women, after consultation with a gynecologist, we, as a rule, perform anesthesia with a reduced level of adrenaline, so as not to provoke the onset of labor in the later stages, and not to provoke a miscarriage in the early stages.
Extraction for acute and chronic inflammation
Quite often, the removal of a problematic tooth is accompanied by the presence of purulent foci, gum inflammation or periodontitis. In such cases, the doctor prescribes intensive therapy with the use of antibacterial drugs, and only after the inflammatory process has been suppressed is surgery to remove the tooth performed.
There are also situations when a tooth needs to be removed urgently. Only an experienced, highly qualified doctor can perform surgery in such cases.
Removal of a wisdom tooth near the maxillary sinus
If the wisdom tooth is located near the maxillary sinuses, there is a certain difficulty in such removal. Why?
If a wisdom tooth is located close to the maxillary sinus, there is a risk that during removal the tooth can be pushed into the maxillary sinus. If you make incorrect technical movements when removing a tooth, or work roughly in some way, you can harm the person and, accordingly, you will then need expensive long-term treatment to remove this tooth.
Are there any specifics to removing wisdom teeth?
Of course, there are some peculiarities when removing wisdom teeth. The doctor’s task is to make the removal process as accurate as possible, as atraumatic as possible - in principle, like the rest of the teeth. But in the case of a wisdom tooth, there are some peculiarities of anatomy.
The peculiarities are that the figure-eight tooth is located quite far away and quite well hidden. But at the same time, using modern equipment, modern materials and having experience, you can remove wisdom teeth quickly and accurately enough without consequences or injuries.
In what cases is dental surgery difficult?
Complex manipulations regarding tooth extraction include the following situations:
- with disconnected roots that are excessively curved inward or directed in different directions;
- when the problem tooth is located in the affected bone;
- in the complete absence of a crown, when there is nothing to grab onto with forceps;
- if a filling was previously installed in the tooth, which can crack under the mechanical influence of forceps;
- when the tooth is impacted or dystopic;
- removing the "eight"
These are the main clinical features in which it is impossible to get rid of a diseased tooth using a standard simple procedure. Moreover, in each specific case the reasons for complex extraction may be individual.
Competent removal of wisdom teeth
How to remove a wisdom tooth in the least traumatic way?
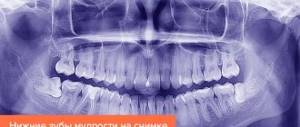
The wisdom tooth is removed atraumatically after carefully evaluating the computed tomography scan, talking with the patient, and assessing his clinical case. The tooth is separated - divided into parts if it has any bends, slopes, or several roots. And, accordingly, with the help of elevators, luxators - special dental instruments, it is carefully and carefully dislocated.
There is no need to worry about the appearance of some blood after wisdom tooth removal. The removal is carried out under the full supervision of a doctor; the wound after tooth extraction is sutured and sutures are applied. What follows is a standard rehabilitation protocol without any surprises for the patient. The only thing is that after the removal of a wisdom tooth (wisdom teeth), swelling of the mucous membrane is possible.
Why is atraumatic tooth extraction more preferable?
With this removal, the doctor takes care of the health of the patients. So that the healing takes place as comfortably as possible, so that there are no consequences after this, so that the patient in the near future, after 7-10 days, forgets that he had his wisdom tooth removed. It is after this time that possible swelling and pain after removal are completely removed.
How is tooth root resection performed?
The meaning of the resection operation is to cut off the apex of the tooth root with a drill along with the “purulent sac”. And many patients are therefore immediately interested in the question of how long the tooth will last after resection. It must be said that the operation does not affect the service life of the tooth in any way, because The size of the root part to be removed is very small.
Tooth root resection is a fairly simple operation and usually lasts from 20 to 40 minutes. The front teeth are operated on faster, which is due to the convenience of visual control of the operation, but the lateral teeth (6-7 molars) require more effort and time from the doctor. In the animation below you can see all the main stages of the operation.
Tooth resection: animation
Preparing for surgery –
Tooth resection can be carried out only if there is no active purulent inflammation in the area of the root apex. If there is swelling of the gums or pain when pressing on a tooth, you must first remove the active inflammatory process.
The essence of preparation for surgery is high-quality filling of the root canal (Fig. 4). If resection is planned as the final stage of therapeutic treatment of chronic periodontitis, then the root canal is filled no more than 1 day before surgery (24stoma.ru). It is important that the canal is very tightly filled with a filling substance (for example, gutta-percha), because if the obstruction of the canal is not dense, the granuloma/cyst will then appear again.
If the operation is planned on a tooth where the root canals have already been filled, then the strategy may be different. For example, if the canal of this tooth is well sealed along its entire length (except at the very top of the root), it is not necessary to unseal such a canal, because the top will still be cut down. In all other cases, root canal refilling will be required.
Operation technique –
The operation is performed under local anesthesia and is absolutely painless. Moderate pain occurs only after the operation is completed, which will require taking painkillers. Below you can see the progress of the operation in detail on schematic images and videos, but first we will draw your attention to the main points during the operation.
Main stages of the operation –
Creating access to the root apex - the gum is dissected and moved away from the bone in the projection of the root apex of the causative tooth. After this, a “window” is drilled into the bone with a drill, through which the apex of the root is cut off and the granuloma or cyst is scraped out (Fig. 4b).- Root resection and cyst removal - through a hole created in the bone, the surgeon cuts off the tip of the root and scrapes out a chronic source of inflammation (this can be a granuloma or a cyst). The latter differ from each other only in size. The cyst shell must be removed completely, because if you leave even a small fragment of it, the cyst will form again.
- Suturing the wound - after antiseptic treatment of the wound, the edges of the gum mucosa are put in place and the wound is sutured. In good clinics, immediately after the operation the patient will be given ice to hold, pressing it to the cheek in the projection of the operation (this will reduce the amount of swelling). The stitches are removed after 8-10 days.
Operation diagram (Fig. 5-10) –
If the cyst was large, then bone healing can be stimulated with special osteoplastic materials based on synthetic hydroxyapatite - the preparations “Kolapol” or “Kollapan”. In some cases, retrograde root canal filling may also be used during resection surgery (see below).
Pain after wisdom teeth removal
How long does pain last after wisdom tooth removal?
Pain after the removal of wisdom teeth lasts differently, depending on the sensitivity of the person and how the healing proceeds in general. It hurts after removing the figure eight from several days to, maximum, 7-10 days. Naturally, all pain, all painful symptoms from wisdom tooth removal subside over time.
What should you do if the wound hurts for a long time after wisdom tooth removal?
If you experience prolonged pain after wisdom tooth removal, you should contact your doctor as soon as possible, and he will adjust his prescriptions. If any problems arise, he will solve them.
When should wisdom teeth not be removed?
What can serve as a contraindication to wisdom tooth removal? A contraindication to wisdom tooth removal may be a person’s health condition, as a result of which we cannot subject him to such a surgical intervention.
For example, if the patient suffers a heart attack in the near future, within six months. Or he has some kind of uncompensated disease. In these cases, we first prepare the patient, consult with related specialists, and after that, as planned, we carry out removal procedures.
Preparing for dental surgery
If a patient is faced with the removal of a complex tooth, then an experienced doctor will not perform such manipulations without prior preparation. An x-ray is required before the operation. This is necessary to clarify the location of the tooth in the bone, as well as to evaluate the tissues surrounding it.
When a patient has an inflammatory process, it is first cured by taking antibiotics.
Complications after pulling out problem teeth rarely occur, but to avoid them, the procedure should be trusted to a highly qualified doctor.
Complications after wisdom tooth removal
What may be the cause of complications after removal of figure eights?
Complications after removing the figure eight - yes, they exist. Complications are different: they occur directly during the removal procedure, there are delayed ones, blood vessels may be damaged, and bleeding may occur. There may be a fracture of the jaw, a breakage of a section of bone tissue that is located in close proximity to the wisdom tooth.
Long-term complications – for example, wound infection in the case of unsterile instruments. If the doctor did not warn the patient that he needs to take antibiotics prophylactically for an impacted wisdom tooth.
What are the complications after wisdom tooth removal?
After the removal of a wisdom tooth, there are complications of different etiologies: they can either arise immediately or be delayed. Bleeding may immediately occur, your jaw may break, a piece of bone may break off (both small and large) - then your jaw will begin to hurt. You can tear the mucous membrane, injure a neighboring tooth, break a neighboring tooth, etc. Your gums or throat may begin to hurt.
Delayed complications are oral infection, periostitis, alveolitis, inflammation of bone tissue.
Can the temperature rise after wisdom tooth removal?
After the removal of a wisdom tooth, the temperature may rise in people who are very nervous or have suffered a lot of stress. This will be a vegetative-vascular reaction, and once the temperature can rise to 38.5-39 degrees. Once. It can be brought down by the use of antipyretic drugs and, accordingly, it should no longer be present. There may be a low-grade fever of 37 degrees, 37.1-37.2, for several days after removal. This does not have any consequences, this is normal, but you should, of course, inform the doctor about this so that he takes this fact into account and adjusts his prescriptions.
Can gumboil appear after wisdom tooth removal?
After wisdom tooth removal, gumboil may appear. This can happen as a result of a wound becoming infected. For example, the use of non-sterile instruments, non-sterile materials. This can also be a result of the removal of an impacted wisdom tooth, for example, if the doctor “sutured it in tightly”, and there are a lot of bacteria in our oral cavity, and did not prescribe antibiotic prophylaxis. In this case, flux is likely to occur.
Crown as a way out
Pathological tooth wear can be eliminated with the help of crowns. They can be installed both on the front teeth and on the chewing teeth and restore the aesthetics and functionality of the oral cavity. Crowns can be made from various materials, each of which has its own advantages and disadvantages:
| Material | pros | Minuses |
| Metal ceramics | Durability, high aesthetic qualities, not the highest price | Depulpation of the tooth and grinding of a large amount of hard tissue are required. |
| Metal-free ceramics | The best aesthetics that are not lost over time, high strength, durability. | High price. |
| Metal | High strength, durability, low cost. | Lack of aesthetic qualities. |
When choosing a certain material, the patient must understand that he will need to replace a large number of crowns (perhaps even all). Therefore, it is worth giving preference to those materials that have good aesthetic qualities and a long service life.
After all the nuances of prosthetics have been agreed upon, we proceed directly to the procedure itself. At the first stage, the oral cavity is sanitized and teeth are prepared for crowns. Next, the doctor takes impressions of the jaws, based on which the dental technician makes a prosthesis. These operations may take some time, so the patient may be offered temporary plastic crowns. They will protect prepared teeth from the aggressive environment of the oral cavity and help adapt to new teeth. After the final version of the prosthesis is ready, it is tried on again and fixed with permanent cement.
Dry socket syndrome during wisdom teeth removal
Dry socket syndrome in wisdom teeth
The wisdom tooth refers to the concept of dry socket, or more precisely, dry socket syndrome. A dry tooth socket is alveolitis. Dry socket syndrome after the removal of figure eights can occur in this area, especially in the area of the lower wisdom teeth due to the fact that as a result of swallowing, as a result of opening the mouth, muscles tense, which aggravate the occurrence of alveolitis.
What can dry socket syndrome lead to and what to do?
A dry socket after the removal of figure eights can lead to very severe pain that radiates to the temple and ear. This is a very great torment: a person cannot, even if he is not sensitive, he cannot tolerate it, he will definitely take painkillers 4-5 or 6 tablets. And as a result of this, he will still go to the dentist. A dry socket, if it has formed after removal, will not go away on its own. Alveolitis can only get worse - up to inflammation of the jaw. There may be dire consequences.
Extirpation of tooth pulp
Extirpation of dental pulp: indications, methods, possible consequences Pulp pathologies are treated with medication whenever possible, but if the patient postpones a visit to the dentist “for later,” therapy may be powerless, and extirpation of the dental pulp is prescribed. There is no point in waiting for a miracle and hoping that advertised remedies will help; it is better to consult a specialist in a timely manner to avoid serious consequences, including tooth loss and inflammation of the nerve canals throughout the jaw.
Pulpectomy: causes and symptoms
The indication for dental pulp extraction is damage to the connective tissue that fills the tooth cavity. 20% of patients go to dentistry with varying degrees of pulpitis, half of them are recommended for such an operation. There is no need to be afraid; modern methods and equipment allow surgical treatment to be carried out as safely and painlessly as possible. It is necessary to devitalize the “nerve bundle” when:
- irreversible cases of pulpitis, when therapy does not have a positive effect and is not able to stabilize the situation;
- periodontal pulpitis;
- fracture of the dental crown, with complications on connective tissues.
Symptoms of acute and chronic pulpitis are sometimes confused with signs of caries. The main difference from carious manifestations is that there are no prerequisites for the appearance of painful sensations, i.e. The tooth hurts greatly without touching it or eating hot or cold.
Important! If pulpitis has become chronic, symptoms may change. Discomfort due to temperature contrast, mild aching pain. It seems that a miracle happened and the disease went away. This is wrong. A subsided pathology is dangerous due to exacerbations, when painful sensations intensify tenfold and possible complications: periodontitis, cyst, necrosis of the jaw.
Do not forget that dental pulp extraction is a surgical intervention, so there are certain contraindications for the operation. Modern techniques used in professional clinics with high-quality equipment minimize the list of prohibitions, but doctors do not recommend removal if:
- complete obstruction of the tooth canal;
- the presence of an atypical (unformed) tooth root;
- severe disorders of the nervous system during exacerbation;
- immunodeficiency pathologies;
- individual intolerance (allergy) to any type of anesthesia.
Important! Pulp extraction may also be recommended if the pulp is in a healthy condition. The intervention is prescribed if preparations are underway for tooth implantation, and nerve-fibrous connections can cause pain after the implant is installed.
Methods for removing “problematic” pulp
The most effective and safest methods today are:
Vital
The main advantage is that it is carried out in one visit and does not require the use of devitalizing drugs. The method is popular both among patients and among dentists and is as follows:
- upon examination, pathology is revealed;
- the affected tooth is professionally cleaned;
- anesthesia is administered according to the person’s predisposition; if necessary, pulp extirpation can be performed under general anesthesia;
- special instruments are used to cut off the arch of the dental cavity;
- a pulpectomy is performed;
- the length of the channel is measured and given the correct shape;
- antiseptic treatment is carried out;
- The canal is filled with a permanent filling.
Devital
The traditional method is when the pulp is removed immediately after its killing using arsenic or parapharmamaldehyde paste. In some cases, electrochemical necrosis is used to kill the pulp in hard-to-reach places. This technique is not applicable if there is a purulent form of pulpitis or the tooth root is not fully formed. The process looks like this:
- dentist consultation, diagnostics;
- tooth brushing;
- opening the dental cavity and applying devitalizing paste;
- installation of a temporary filling.
After the nerve connection ceases to exist, the temporary filling is removed, the tooth canal is cleared of pulp, disinfection is carried out and a permanent filling is installed.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
To eliminate the risks of complications, it is better to perform dental pulp extraction in dentistry with modern equipment and a high level of sterility. Infection can reduce all the doctor’s efforts to zero. “32 Dent” uses only proven and safe methods for treating pulpitis, so we are confident in the effectiveness of the procedures.
Sources:
- Personal experience as a dentist;
- E.V. Borovsky. Therapeutic dentistry, - M.: 1997;
- N.V. Kuryakina, N.A. Savelyeva. Preventive Dentistry, - M.: 2003;
- Khomchenko L.A., Bidenko N.V. Practical endodontics.-Moscow. Book Plus, 2005;
- Practical therapeutic dentistry: Textbook / A.I. Nikolaev, L.M. Tsepov. — 6th ed., revised. and additional - M.: MEDpress-inform, - 2007;
- Borovsky E.V. Clinical endodontics. — 2nd ed., add. And correct. / E.V. Borovsky. - M.: JSC "Dentistry", 2003;
- Bir R. Endodontology: Atlas. Per. from English / R. Beer, M.A. Baumann, S. Kim. - M.: MEDpress-inform, 2004;
- Iordanishvili A.K., Kovalevsky A.M. Endodontics plus. - St. Petersburg: Normed-izdat, 2001;
- B. Basrani - Endodontic Irrigation. Chemical Disinfection of the Root Canal System (2015);
- Peter Murray - A Concise Guide to Endodontic Procedures (2015).
Recommendations after wisdom tooth removal
What medications should you take after wisdom tooth removal?
The following medications are used after wisdom tooth removal: painkillers, mouth rinses - special, with a strong antiseptic content. Often, an antibiotic is prescribed as therapy after the removal of the figure eight, and we also prescribe probiotics to restore the intestines after taking antibiotics.
Recommendations after wisdom teeth removal
In general, the recommendations are the same as in the case of removing simple teeth. But they should be performed more carefully.
Physical exercise
–
exclude
. Try not to disturb the extraction site, because the wisdom tooth is located in an awkward/unfortunate area where swallowing and opening the mouth will affect the surgical site.
Of course, wisdom tooth removal is incompatible with subsequent alcohol consumption for several days. Smoking is also strictly not recommended.
Brushing your teeth after wisdom tooth removal
Is it necessary to brush your teeth after wisdom tooth removal or can you wait a few days? You should definitely brush your teeth after removing a wisdom tooth. This needs to be done quite carefully, but at the same time carefully. It is not recommended to rinse your mouth after wisdom tooth removal. That is, the question “what to rinse your mouth with” in this case disappears. Using an irrigator is also not recommended.
Restoration of worn teeth
Restorative treatment is carried out while preserving at least half of the hard tissues of the tooth. The technique takes place in several stages:
- Preparation. Necessary to identify the causes of diseases and their elimination or minimization, as well as the protection of remaining teeth. During preparation, an occlusal splint is made and installed if the patient suffers from bruxism. If necessary, the doctor prescribes consultations with various specialists, explains the rules of oral hygiene, and sanitizes foci of infection.
- Evaluation of the preparatory stage. After some time, the patient comes for an appointment, and the doctor assesses the condition of the teeth, checks whether the patient followed all the recommendations correctly, and discusses the upcoming treatment with him.
- Restoration. It is carried out in a certain order. First, the teeth are prepared, then the teeth on the upper jaw are restored, and only then on the lower jaw. Using a table of anthropometric data for each tooth, the doctor gives the patient's new teeth a certain length and shape.
- Observation. After successful treatment, the doctor observes the result for some time. In the first year, the patient should come for an appointment once a month, then less and less, but not less than once every 12 months. If any defects are identified, they are repaired or other treatment methods are applied.
This type of treatment, like any other, requires the patient to strictly adhere to all recommendations, give up bad habits, eat right, regular examinations by a specialist, and carefully observe hygiene skills.
Removing 2 wisdom teeth at the same time
Removal of two wisdom teeth from one side of the jaw. Pros and cons of this approach.
Two teeth at once on one side is a very good technique. In this case, we immediately remove two teeth and the healing process takes place only once. Accordingly, the pain also disappears once. The healing is in no way burdened by the fact that we remove two of them at once. It’s a good, even excellent approach, and that’s what we do in most cases if the patient doesn’t mind.
An example of removing two wisdom teeth at once - HERE
When to start treatment
The problem does not appear suddenly; it is characterized by a long course with gradual progression. The sooner treatment begins, the shorter and less radical it will be. That is why you should contact your dentist when the first signs of the disease appear, which include:
- Increased sensitivity of dentin.
- Reaction to hot and cold food.
- Changes in the color and shape of teeth.
- Early abrasion of enamel.
It must be remembered that there is also physiological abrasion of teeth. It is characterized by a long and slowly progressive course and is a consequence of the natural aging processes of the body. If a patient experiences rapid wear of enamel and dentin at a young age, then it is necessary to immediately contact a specialist for professional help.
Implantation in the wisdom teeth area
Is implantation performed in the area of wisdom teeth?
In the area of wisdom teeth, implantation is not performed in any cases. Due to the fact that there is no space in the jaw to install implants in this area. And, if we look at the jaw, it opens more in the anterior section, and in the posterior section it opens least. If we place an implant, we will not be able to make a normal-sized crown and, accordingly, use these implants for chewing.
During implantation, in case of bone tissue deficiency, the tubercle of the upper jaw or the retromolar space in the lower jaw is used to fix the outermost implants. If there is an impacted eighth tooth in this area, it is removed regardless of the complexity of the operation, since it interferes with the installation of the implant.
Cost of wisdom teeth removal in Moscow
The price of removing one wisdom tooth in Moscow clinics, if we talk about low-traumatic removal of both lower and upper wisdom teeth, can start from a price of 15 thousand rubles
and higher. The fact is that when removing a figure eight, the cost of bone material, which is used for small bone grafting, can be added to the price of the removal itself, since after removing a deep-lying figure eight, a void may form, which, you see, needs to be eliminated due to fears of the development of atrophy bones in this area.
But many doctors, both in Moscow and in the regions, neglect bone grafting and simply suturing the wound, thereby reducing the cost of wisdom tooth removal to 8-10 thousand. The choice of price always remains with the patient, but the patient also needs to evaluate the risks of such removal, look a little into the future and understand that saving 5-10 thousand rubles at this step may result in future problems with the 6th and 7th chewing teeth ... But this is a completely different story.
How is pathology determined?
Only a specialist can detect a violation during tooth wear. Of course, the general picture among the population is taken as the norm, but the doctor also takes into account individual factors:
- general condition of the enamel;
- presence or absence of exposed dentin;
- work of the temporomandibular joint;
- condition of the mucous membranes of the tongue and cheeks;
- degree of severity of nasolabial folds;
- sensitivity of the masticatory muscles.
It is interesting that in addition to all the individual characteristics, the doctor is interested in the sound with which the jaws close. A sharp, clear and short sound indicates that there are no problems. A long-lasting sound accompanied by a squeak indicates deficiencies in the functioning of the TMJ or problems with the nervous system.
You can understand that teeth are subject to increased abrasion by the first sign - increased sensitivity. It is sharper when the upper hard layer of enamel is significantly abraded.