What is dystonia?
Dystonia of the tongue muscles causes involuntary movements of the tongue and uncontrolled mobility of structures adjacent to the tongue, which can lead to problems with chewing food and articulating sounds. As experts note, this may result in weight loss and loss of the ability to speak. In particularly severe cases, for example, when a patient may suddenly choke on food, tongue dystonia can provoke the development of more serious health problems.
According to observations, musicians who play wind instruments are more susceptible to spasms of the mouth muscles.
Symptoms and treatment
The main symptoms include the following:
- incomprehensible, slurred speech;
- spastic manifestations in the articulatory muscles (neck, lips, face, tongue are constantly tense, articulation is limited, lips are tightly closed);
- hypotonia of the articulatory apparatus (lips do not close, tongue lies motionless in the mouth, mouth is slightly open, increased salivation);
- dystonia of articulatory muscles (when a child tries to talk, his muscle tone goes from low to high);
- slurred pronunciation;
- in difficult cases, the child misses sounds, replaces them or pronounces them distorted; Source: O.Yu. Fedosova Features of sound pronunciation of children with mild dysarthria // Speech therapist in kindergarten, 2005, No. 2, pp. 36-41
- slowness of conversation;
- inability to speak (in severe forms);
- nasal voice without signs of a runny nose;
- change, omission, replacement of some sounds with others;
- fading of a phrase towards the end of its utterance, rapid breathing during a conversation due to lack of air;
- very high, almost “squeaky” voice;
- a fast or very slow flow of words, while the child cannot change the tone.
What causes dystonia?
Since tongue spasms are not a disease, but only a symptom, it can be difficult to name a specific cause for this phenomenon. Experts distinguish three types of dystonia: primary, or idiopathic (sudden spasms of unknown etiology), hereditary (through at least one parent) and secondary, or symptomatic (acquired as a result of illness or injury). Both Russian and foreign scientists believe that all three types of dystonia are associated with the same part of the brain, the basal ganglia, which control muscle contraction.
Types, levels and forms of speech dysarthria in children
Table of types of disease by location of the lesion
| Name of the pathology form | Peculiarities |
| Cerebellar | Occurs when the cerebellum is involved in the process. Speech is drawn out, slurred, slow, the volume constantly changes, the child’s tongue trembles, he speaks with shouts, as if chanting slogans. Additional symptoms: poor balance, unsteady gait. |
| Bulbarnaya | It is caused by paralysis of the articulatory muscles, as well as the nerves - vagus, glossopharyngeal, ternary, sublingual and/or others. Children lack some reflexes, sucking and swallowing, facial expressions are impaired, and it is difficult for them to chew solid food. There is also increased salivation, simplification (all consonants “merge” into one fricative) and slurred sounds, a nasal, hoarse sound of the voice, sometimes its absence. |
| Pseudobulbar | Occurs with centralized paralysis (spastic) of muscles and their hypertonicity. Speech becomes monotonous, it is difficult for the child to lift the tip of the tongue, move it to the side, or hold it. There is increased salivation, soreness, and swallowing disorders (increased reflex). Speech is slurred, nasal, the pronunciation of hissing, whistling and tone sounds is sharply impaired. |
| Extrapyramidal | It occurs when the function of the subcortical nuclei is disrupted, and therefore received a second name – “subcortical”. Speech is slightly nasal, slurred, and slurred. There are involuntary muscle movements, facial expressions, and articulatory spasms. The timbre and strength of the voice changes, the pace of conversation is disrupted, and there are occasional guttural cries. |
| Cortical | Damage to those areas of the cerebral cortex that are responsible for articulatory muscles. Children pronounce words correctly in structure, but with impaired pronunciation of syllables. There is difficulty breathing during conversation and voice. |
| Cold | Manifests itself as one of the symptoms of myasthenia gravis (fatigue and weakness of striated muscles). Speech disruptions occur when the air temperature in the room where the child is located increases or decreases. |
Classification according to the degree of development of pathology:
- I (erased) - only a speech therapist can identify incorrect pronunciation during examination and examination, almost complete recovery is possible;
- II – pronunciation is clear, but defects are noticeable;
- III – the child is understood only by close people, strangers rarely;
- IV – even relatives do not understand the pronunciation or there is no speech, most often considered within the framework of cerebral palsy.
Important! The erased form is characterized by difficulty chewing solid food. Parents should not change their child's diet because of this. It is necessary to gradually accustom him to chew on the same basis as other people. Source: E.F. Arkhipova Erased dysarthria in children: a textbook for university students // M.: AST: Astrel: KHRANITEL, 2006, p.319
Treatment of tongue spasms
But how can all this help people suffering from tongue spasms? Since dystonia greatly affects the lives of patients, many researchers are busy developing various methods of treating it. The most conservative approach is offered by speech therapy. Repeated exercises strengthen the tongue muscles, and the patient learns to properly tense and relax them when speaking and swallowing food, experts explain.
A more radical method is Botox injections. Botulinum toxin temporarily paralyzes the facial muscles, preventing spasms, but such injections must be done every two to three months when the effect of the drug wears off. Despite a number of disadvantages, this method of treating dystonia is the most effective today, clinicians note.
Treatment of dystonia involves the participation of a whole group of doctors from various specialties. The approach to treatment will depend on the nature of the symptoms that bother you, as well as on your desire to use the treatment method suggested by your doctor. Tongue spasms can cause a lot of trouble, but once the correct diagnosis is made and the appropriate treatment is chosen, patients can expect to return to normal life.
Neurogenic suffering of the tongue
Neurogenic suffering of the tongue
Neurogenic suffering of the tongue is divided into motor and trophic; This also includes sensitivity disorders.
Motor neuroses of the tongue are predominantly lesions of the hypoglossal nerve (n. hypogloesus). Disease of the central tracts of the hypoglossal nerve causes unilateral paralysis of the muscles, in which the act of swallowing is not impaired. Nuclear lesions mainly cause bilateral paralysis, leading to complete disruption of the act of swallowing, if the accessory nucleus of the hypoglossal nerve is not preserved.
When diagnosing these lesions, it is necessary to carry out a special neurological examination, as well as determine the involvement of other cranial nerves and pyramidal tracts. Diagnosis of traumatic injuries of the hypoglossal nerve is relatively simple.
Bilateral damage to the hypoglossal nerve nuclei is often observed with bilateral bulbar palsy. First, movement disorders occur, then tongue atrophy and lingual dielalia (speech damage), followed by impaired swallowing and lip movement. A similar symptom complex can occur with tabes dorsalis.
Similar, but unstable symptoms of motor paresis of the tongue can occur as a result of encephalitis during the phenomena of pseudobulbar paralysis. We observed a case of paralysis of the hypoglossal nerve of gunshot origin.
Unilateral damage to the hypoglossal nerve causes the tongue to deviate in the opposite direction when the tongue is at rest in the oral cavity. When protruding, the tongue usually deviates in the healthy direction.
Tongue spasms can occur with epilepsy, tetanus, rabies, hemiplegia, and motor semiparalysis.
A professional tongue spasm has been described among clarinetists, similar to the spasm of the fingers of scribes.
With tabes and cortical lesions in the center of movement, significant speech disorder may occur due to tongue ataxia.
Trophic neuroses of the tongue sometimes find their expression in angiospastic phenomena, in the phenomena of focal desquamation of the papillae.
Sensitive disorders of the tongue represent the most common neurotic lesions; they are usually accompanied by similar lesions in other parts of the trigeminal nerve. Pain sensitivity of the mucous membrane varies in different parts; this must be kept in mind when performing a comparative study of individual areas and take into account the relativity of the indicators and the topography of pain sensitivity in the zone of physiological hypalgesia and analgesia. With the exception of the lips and the tip of the tongue, pain points are very poorly distributed in the oral cavity (see table).
Anesthesia can be a consequence of various diseases. More often, anesthesia of half the tongue is observed - with lesions of an anatomical nature (cerebral and bulbar, damage to the tympanic plexus, lesions in ear diseases) and functional nature (hysteria). Clinically, this type of anesthesia does not always occur quite clearly, since sensitivity in the tongue is partially preserved in areas innervated by other nerves; the main part of the back and tip of the tongue is innervated by the lingual nerve, which belongs to the III branch of the trigeminal nerve; in addition, the superior laryngeal nerve (n. Iaryngeus superior) and the lingual branches of the glossopharyngeal nerve (n. glossopnaryngeus) also provide sensitive innervation of the tongue.
Hyperesthesia of the tongue constitutes a very important group of disorders of the sensitivity of the tongue in practical terms. This group includes neuralgia and glossodynia.
Neuralgia of the tongue is a disease caused by damage to the lingual nerve, which is a manifestation of trigeminal neuralgia, mostly together with neuralgia of the mandibular nerve. The pain is of a typical paroxysmal nature; they arise spontaneously or under the influence of minor external irritations of a physical (eating, talking) and sometimes mental nature.
Due to the fact that patients with neuralgia of the lingual nerve protect their tongue and try to use it little, upon external examination the tongue often appears coated with a gray or brown coating. The presence of plaque is not, of course, an objective sign of neuralgia, but should be considered as a symptom indicating the presence of reasons that reduce the self-cleaning of the tongue. In case of complaints of neuralgic pain isolated in the tongue without damage to the mandibular nerve, it is necessary to look for objective signs of damage in the tongue itself or at the location of the lingual nerve.
Therapy - neuralgia - X-ray irradiation, galvanization, diathermy of the cervical nodes, novocaine blockade and injection of alcohol into the lingual nerve or resection of the lingual nerve. The last two operations are undesirable, since they cause loss of sensitivity of the back of the tongue, and injection of alcohol, in addition, is often accompanied by loss of sensitivity in the area innervated by the inferior alveolar nerve.
For injection into the lingual nerve, 80″ alcohol is sometimes used, which is administered in an amount of 0.5 ml. Large quantities should not be administered for fear of damage to the mandibular nerve. Novocaine is injected in a 0.25% solution in an amount of 3-5 ml.
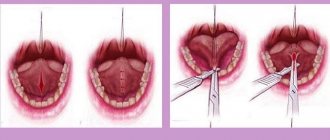
The injection technique is the same as for mandibular anesthesia, with the difference that the needle should not be brought to the mandibular foramen. For this purpose, the tip of the needle is deflected 0.25-0.5 cm to the midline from the bone. It is more convenient and accurate to inject behind the lower molars at the point of transition of the mucous membrane from the side surface of the tongue to the floor of the mouth, which corresponds to the place where the nerve enters the tongue. Injection is carried out one or more times, depending on the observed effect. In order to inject alcohol into the lingual nerve, the latter can be previously exposed in order to carry out alcoholization under eye control. Exposing the nerve gives more accurate results. It is also performed for resection or twisting. The technique for exposing the lingual nerve is as follows. The lingual nerve is exposed from the side of the oral cavity. The nerve enters the tongue between the ascending ramus of the mandible and the anterior arch of the pharynx and lies under the oral mucosa at the large molars at the junction of the mucosa from the lateral surface of the tongue to the floor of the mouth. At this point, the lingual nerve can be exposed from the mucosal incision.
Glossodynia. A disease characterized by an increase and change in the sensitivity of the tongue, but in its manifestations significantly different from neuralgia of the tongue (neuralgia of the lingual nerve), is called glossalgia, or, in the terminology of some authors, “glossalgia”. Glossodynia should include lingual itching (pruritus linguae) and other similar diseases.
The etiology of glossodynia, or glossalgia, is different and is associated with a number of general changes in the condition of the body, such as, for example, stomach diseases accompanied by impaired secretion, blood diseases (anemia), helminthic infestation, decreased function of the gonads, menopause, hysteria. Locally existing pain can be activated by irritation of the carotid sinus. Carotid stigmatization (intensification) of pain may be accompanied by broad repercussiveness, i.e., the presence of separate pain reflexes evoked from different areas of the body. Therapy aimed at eliminating or reducing the manifestations of one of the diseases such as those listed above often gives positive results in relation to glossodynia.
Clinical manifestations of the disease are expressed mainly by subjective disorders. Patients complain of a burning or tingling sensation in the tongue. The localization of this feeling is uncertain, although patients often point to the tip and root of the tongue. Sometimes patients define their sensations as itching or a feeling of awkwardness in the tongue, heaviness, clumsiness, and fatigue of the tongue. The appearance of these sensations is independent; Sometimes patients associate it with general fatigue, length of speech, ingestion of meat foods or spicy foods. In general, these sensations are rarely acute or painful. The duration of the unpleasant sensation varies: minutes, hours, days; the longer it lasts, the less pronounced it is. Sometimes these sensations disappear for a long period, do not appear for several months, and then reappear.
Most of these patients suffer from a fear of cancer (cancerophobia). They look for manifestations of cancer, examine their tongue themselves and, without knowing the anatomy, find signs that supposedly confirm the diagnosis of cancer: a tumor, especially at the root of the tongue. There are also frequent cases of intragenic diseases when the doctor mistakes the lymphatic follicles of the tongue for ulceration, which is what the patient is assured of. One way or another, it is necessary to remember that those suffering from glossodynia often have a traumatized psyche, which requires close attention from a doctor and special care when determining their condition. Visible objective changes in glossodynia, or glossalgia, are usually absent. Sometimes hyperplasia of the lymphoid apparatus of the tongue is detected, sometimes the phenomenon of atrophic glossitis. However, in most patients, significant deviations from the normal appearance of the tongue cannot be detected. The manner of showing the tongue is very typical in a number of cases. Some patients so often examine some side of the tongue where they suspect the presence of a lesion that they teach the tongue to turn only in one direction when protruding. This “one-sided display” of the tongue is very typical for patients with glossalgia and gives an idea of the patient’s mental experiences. When making a differential diagnosis, one should keep in mind arthritis of the maxillotemporal joint.
Treatment of glossalgia primarily requires general intervention, depending on the suspected diseases of other systems. In women in the premenopausal period or with symptoms of dysmenorrhea, good results are obtained from the administration of ovarian preparations (ovarin, folliculin, sinestrol). For vagotonic patients with symptoms of increased acidity of gastric juice, it is sometimes useful to prescribe atropine preparations. On the contrary, for complaints of dry mouth, small doses of pilocarpine orally (1% solution from 4 to 8 drops two to three times a day) have a beneficial symptomatic effect. In some cases we were able to achieve improvement in this way. It is useful, according to our observations, to prescribe liver preparations internally in cases where anemia is not detected. The patient's psyche should also become the object of therapeutic intervention. In some cases, according to our observations, diathermy of the cervical nodes has a good effect.
Local therapy of the tongue is not required. Neutral interventions, not of an irritating nature, can be prescribed only for psychotherapeutic purposes. Particular attention should be paid to the environment, mainly teeth (natural and artificial). When assessing the possible effects of teeth and dentures on the tongue, it should be taken into account that with glossodynia, the doctor is dealing with an organ whose sensitivity to irritation, in particular mechanical, is exacerbated, and sometimes perverted. Therefore, first of all, it is necessary to eliminate all possible sources of mechanical irritation in the oral cavity. Despite the lack of instructions from the patient, his worn-out fillings should be replenished, poorly placed fillings should be replaced, and missing ones should be restored. The surface of the fillings should not have the slightest roughness. Not a single rotting root, not a single cavity, not a single sharp protrusion should be left in the oral cavity. The same strict requirements must be made! to prosthetic structures. Old dentures with porous rubber should be removed immediately. Poorly fitted crowns with edges lagging behind the neck, with worn chewing surfaces, so-called saddle-shaped bridges, bridges with “sticks”, etc. - all this must be removed in a certain sequence.
Particular attention should be paid to the presence of different metals in the mouth (metal filling - gold crown). Due to the potential difference between dissimilar metals, electrical phenomena may occur that irritate the highly susceptible mucous membrane of the tongue. Poorly chrome-plated metal prostheses should also be considered a source of possible irritation. There is no reason to consider the prognosis for glossodynia to be unfavorable in the sense that this disease is not complicated by any severe disorders. However, it is sometimes difficult to cure this suffering, since those general disorders that cause glossodynia cannot always be eliminated.
Taste disorder. Neuroses of the tongue include various taste disorders. Disorders of the sense of taste can be of a different nature: ageusia (ageusia) - loss of taste, hypogeusia (hypogeusia) - decreased taste, parageusia (parageusia) - perversion of taste. Those changes in taste that arise as a result of putrefactive processes that occur during stomatitis should not be confused with neurogenic disorders of the sense of taste. In these cases, there is not a taste disorder, but the emergence of sources of unpleasant taste that mask or distort the usual taste sensations when eating food.
Lesions of the lingual nerve cause disturbances in the sense of taste in the anterior part of the tongue, while lesions of the glossopharyngeal nerve cause disturbances at the base of the tongue. Ageusia occurs with lesions of the trigeminal nerve (Gasserian ganglion, lingual nerve, chorda tympani) and with central lesions (tabes, progressive paralysis). A transient disappearance or decrease in taste is observed during an epileptic attack: during an aura, after an attack, parageusia - sometimes during hysteria.
What to do? Treatment methods for the disorder
The child must undergo additional classes with a speech therapist (at home or in a special institution) on:
- development of motor skills;
- forming a conversation;
- honing diction;
- correcting the pronunciation of distorted sounds;
- expanding vocabulary;
- development of phonetic hearing;
- memorizing grammatical structure.
Against this background, drug therapy is carried out using nootropics. Medicines in this group specifically affect brain functions: stimulate mental activity, cognitive functions, increase learning abilities, and improve memory.
The package of measures also includes exercise therapy - articulation gymnastics to strengthen the facial muscles, massage, exercises with the hands and fingers.
Sources:
- E.F. Arkhipova. Erased dysarthria in children: a textbook for university students // M.: AST: Astrel: KHRANITEL, 2006, p. 319.
- L.I. Belyakova, Yu.O. Filatova. Diagnosis of speech disorders // Defectology, 2007.
- 3. O.Yu. Fedosova. Features of sound pronunciation of children with mild dysarthria // Speech therapist in kindergarten, 2005, No. 2, pp. 36-41.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
What not to do
All manipulations regarding moving the victim in space and changing the position of his head and neck are contraindicated if the person is suspected of having a cervical fracture. Any careless movement towards the victim can harm him even more. In this case, changing the position of the jaw forward and down will suffice.
It is also worth noting that some citizens have a myth firmly entrenched in their heads that it is necessary to remove the tongue and pin it with a pin or needle to the victim’s collar or cheek. Doing this is absolutely contraindicated and pointless. Moreover, first aid for tongue retraction should not be provided by such barbaric methods. To fix the tongue, a regular adhesive plaster attached to the chin will do. Moreover, fixation itself is necessary in extreme cases; changing the position of the head and neck is usually enough.
How can I help?
First of all, the person whose tongue has shifted needs to be placed in a horizontal position. After performing this manipulation, it is necessary to tilt his head back: the left hand is placed on the victim’s forehead, and the right hand at this time raises the neck, and a retainer (pillow, bolster) is placed under it. After throwing back the head, you need to extend his lower jaw. To do this, its right and left corners are taken with both hands, shifted down and then raised forward. If breathing is restored, the person should be turned on his side to prevent relapse.
If these measures do not help to restore the patency of the airways when the tongue is retracted, then you need to move on to a proven and guaranteed method of ending the state of suffocation by getting rid of the causative factor. In this case, this is removing the tongue from the oral cavity and fixing it outside. Manipulation involves pulling the tongue out of the mouth using cloth-wrapped fingers, tweezers, forceps and, in fact, any instrument capable of capturing and holding the tongue. The next step is to secure it at the chin with an adhesive plaster or bandage.
If the displacement of the root of the tongue occurs due to a fracture of the lower jaw, then assistance should immediately begin with removing it from the mouth and subsequent fixation at the chin. Subsequent manipulations, such as matching and connecting fragments of a broken jaw, can only be provided in a specialized institution. Also, in ambulances called, doctors can provide professional assistance with tongue retraction, as they have devices for artificial ventilation of the lungs. A special air duct is placed between the root of the tongue and the wall of the pharynx, providing the lungs with air flow.
Causes of tongue retraction
The main reason for the development of this pathological condition is relaxation of the root of the tongue and the muscles of the lower jaw, which partly control the position of the tongue in the oral cavity. So, for example, if a victim has a broken lower jaw on both sides, then the likelihood of the tongue root being displaced is quite high.
However, in medical practice, such a cause of tongue displacement as a broken jaw is rare. Much more often, this phenomenon occurs during a long coma, during which many muscles, including the tongue, atrophy. A patient's tongue may become retracted after anesthesia is administered before surgery. Pathology is also observed in victims of accidents and other accidents, which entail severe pain shock.
Prevention of tongue root displacement
When a person loses consciousness, the muscles of his body relax, including the tongue, which can fall to the back of the larynx, causing an attack of suffocation. This does not happen so often with ordinary fainting, but a number of measures should still be taken, the purpose of which is to prevent tongue retraction. Its main principle is to tilt the victim’s head back by raising the neck and placing a cushion under it. You can also secure the tongue with an adhesive tape or bandage passing through the bottom of the lower jaw and securing it around the forehead. If the jaw is broken, then you need to act differently: you need to put the person on his stomach, face down.
Epilepsy as one of the reasons
There are still many myths about tongue swallowing during an epileptic seizure. Some people ignorant of medicine try to open the mouth of an epileptic during a seizure with a spoon, pens, or their own fingers, simultaneously fixing the unclenched jaws with a stick or other objects. It should be noted here that such measures not only will not help the patient, but can also break his teeth and damage the oral mucosa.
The only thing a passerby can do to help a person suffering from an epileptic seizure is to try to make the space around him as safe as possible: remove hot and sharp objects to prevent head injury, put soft clothes underneath. During an attack, a person may bite his tongue, but he will never swallow it for another reason: during an epileptic seizure, all the muscles of the body are extremely tense and hypertonic.
However, tongue retraction can actually happen, not during an attack, but after it, when the muscles, on the contrary, are in a state of hypotonicity. In this case, relaxation of the root of the tongue can cause it to move from its usual position and subsequent blockage of the larynx.
Conclusion
Tongue retraction is a rather dangerous phenomenon, which consists in displacement of its root and clogging of the airways. A similar condition occurs when the muscles of the body, including the tongue, relax during unconsciousness, coma and anesthesia, as well as during fractures of the lower jaw.
When the tongue moves, the person begins to choke, the veins in his neck swell, his breathing becomes hoarse, and his face gradually turns blue. You can help a person by tilting his head back and changing the position of his jaw. It also helps to fix the tongue outside the mouth by attaching it to the chin, but in no case with pins or needles.