Adhesion - what is it?
In general, the word “adhesive” translated from English means “adhesive substance, adhesion.” This “glue” is used in dentistry to connect materials of different compositions to tooth tissue (not to be confused with adhesion and cohesion - this is a physical term).
The filling material itself does not have chemical adhesion, that is, the ability to stick to naturally moist dentin, so an “intermediary” is needed here to ensure reliable adhesion of two dissimilar tissues. During polymerization, the composite material shrinks, so if adhesive systems are not used, the desired adhesion quality cannot be achieved. And this is a direct road to the development of repeated caries or even pulpitis under the filling.
“Since childhood, I have been bothered by my diastema, the gap between my front teeth. About 5 years ago I heard that there is such a technique as adhesive dental reconstruction, in which no painful grinding is needed and the material literally “sticks” to the teeth. The doctor simply polished the enamel of the front teeth and covered the unattractive gap in layers with composite. The enamel remained intact, and the smile became open.”
Elena Salnikova, review on the website of one of the Moscow dentists
Innovative light-curing adhesive systems are used for filling teeth with composites, for fixing bridges, as well as for installing braces, veneers, and skypes.
Opinion of Alexey Olegovich Sazonov
In the video, Sazonov’s technique:
Alexey Olegovich Sazonov graduated from MGMSU - Moscow State Medical and Dental University named after. A.I. Evdokimov, majoring in Dentistry. Doctor - dentist-therapist, orthopedist, chief physician of the Art-pro clinic. Work experience - 19 years.
He does not use Chlorhexidine, because he considers its action useless: “MMPs are needed for the transition of altered dentin to sclerotic types.” This is necessary in the presence of deep caries, to strengthen the affected but healthy tissues. Chlorhexidine, according to the doctor, can prevent this. Sazonov uses 95% alcohol. For different generations of adhesives, the operating algorithms are different. More often, Alexey Olegovich adheres to the following sequence (4th generation: acid, primer, adhesive):
- Selective dynamic etching of enamel 15 sec with phosphoric acid, dentin 3-5 sec.
- Rinse with water, DO NOT dry, add 95% alcohol (water from a syringe for 30 seconds), do not dry.
- Rub in the primer 3 times, dry well (1 time).
- Rub in the adhesive and inflate.
- Apply the fluid-flowing composite in a thin layer.
- Polymerization - 10 sec.
There are many articles and studies on this topic, they often contradict each other. First of all, you need to understand the causes of the problems, and not blindly accept recommendations on faith. The relevance of the alcohol adhesive protocol in dentistry will only be confirmed by the long-term durability of restorations.
Classification of adhesive systems
Essentially, the composition of the adhesive system is represented by a group of liquids consisting of an etching component, a bond, and a primer. Together they provide micromechanical bonds between artificial materials and dental tissues.
Since the structure of enamel and dentin is heterogeneous, the adhesive systems used for them are also different. In the classification of adhesive systems, options are distinguished separately for enamel and separately for dentin.
Modern adhesive systems differ in the following characteristics:
- the number of components that are included in their composition (1, 2 or more),
- filler content: if acid is present, it is a self-etching adhesive system,
- curing method: self-curing, light-curing, and double-curing.
Thus, enamel adhesives contain low-viscosity monomers of composite materials. The important point is that enamel adhesives do not work on dentin. Therefore, it is important to either install insulating spacers for the hard part of the tooth, or use a special dentin adhesive - a primer.
Adhesive dentistry: 50 years of progress
Adhesive dentistry is an integral part of dental practice in general today. Although Buonocore and colleagues first introduced the concept back in the early 1950s, adhesive dentistry has undergone many conceptual changes before becoming what we know it in 2015.
Ideas of mechanical connection to tooth structures have been replaced by the principles of adhesive techniques that provide strength and durability to the contact interface.
Although the industry has seen progress for 50 years, the last 10 years have seen key modifications and changes.
Numerous products such as primers, adhesives, and self-adhesive cements have been developed by manufacturers with an emphasis on ease of use.
Despite their best efforts, dentists today are perplexed and somewhat uncertain about the “what, where, when and how” to use given the clinical applications and numerous variations of bonding systems.
As is known, predictably strong adhesion is possible only with enamel tissues, so it makes sense to maximize the bond strength in this area.
Dentists' risk tolerance for adhesion depends on the treatment goal, taking into account the influence of associated factors.
Clinical problems
Today, dentists use two main adhesive systems for bonding composite materials: step-by-step total etch (etch-rinse-prime-bond) or single-step self-etch (etch-prime-bond). These same systems can also be used with adhesive cements for indirect bonding of glass ceramics, polymer ceramics, polycrystalline ceramics and metal structures.
Also used for indirect procedures are self-etching self-adhesive cements, which combine the properties of acid primers and conventional cements to provide, so to speak, a “no-hassle bond.” These two categories of products - adhesive system + composite cement and self-adhesive composite cements - are among the most popular in almost every dental office.
In addition to the direct and indirect bonding procedures mentioned above, the issue of adhesion is relevant when using filling materials, fiberglass endodontic posts, repair of ceramic or composite dentures and dentin desensitization.
During the bonding procedure, dentists must take into account the volume of residual enamel, the qualitative characteristics of the dentin structure, and the possible difficulties of adequate preparation.
Additional chemicals such as silanes or 10-methacryloxydecyl dihydrogen phosphate (MDP monomer) are required for bonding when considering alternative materials and treatments.
With so many components involved, it is not surprising that dentists often find it difficult to argue the appropriateness of using a particular adhesive technique in a particular clinical situation.
Mechanism of action
Total etching
Total etch systems continue to provide the best results, providing a strong bond when enamel is retained and regardless of which specific brand of adhesive is used.
The occurrence of postoperative sensitivity when using phosphoric acid is usually associated more with the bonding technique than with the effect of phosphoric acid itself.
38% phosphoric acid gel is applied to the tooth tissue for 10-15 seconds, after which the application area is washed for the same time and lightly dried with air. This procedure allows for deep etching of the enamel, demineralization of the dentin surface (removal of the “smear” layer), exposure of collagen fibers and opening of dentinal tubules.
A dual-action monomer in a solvent structure (ethanol or acetone) binds hydrophilic dentin and hydrophobic adhesive resin. This promotes the infiltration of demineralized peritubular and intertubular dentin with monomer and adhesive resin substances, increases the wettability of the conditioned dentin surface and improves the contact between dentin and resin.
Partially filled adhesive resin in combination with primer monomers forms strands in the dentinal tubules, and the so-called “hybrid layer” with a thickness of 5 to 15 microns. The latter is the basis for attaching methacrylate groups to cement or composite. The quality of bonding directly depends on the degree of destruction of collagen fibers as a result of excessive drying of dentin when using the total etching technique.
The creation of a thin or no hybrid layer can also lead to postoperative sensitivity caused by incomplete sealing of the dentinal tubules. This factor allows fluid to move in the structure of the dentinal tubules under the influence of temperature stimuli.
Self-etching systems
When using self-etch systems, acidic hydrophilic primers are applied to the tooth structure to partially demineralize the smear layer of dentin, open up the network of collagen fibers and penetrate exposed dentin.
Resin infiltration occurs when the acidic primer becomes hydrophobic, which is necessary to prevent excessive moisture absorption from the dentin. In addition, this can significantly degrade the quality of the clutch. Since the dentinal tubules do not open at all, the incidence of postoperative sensitivity is significantly reduced. This fact is also positively influenced by the use of a not too aggressive acid.
In addition to these benefits, there are fewer procedural steps, which reduces the likelihood of physician errors. The adhesion strength to dentin when using self-etching systems approaches the adhesion strength of the total etching technique, but still it cannot reach the level of similar indicators when bonding to enamel due to the lower pH of the acid primer (pH ~ 0.9-2.8) compared to phosphoric acid (pH ~ 0.6).
The lower the pH of the acid primer, the weaker the etching of the prepared enamel, and the lower the possibility of etching intact enamel compared to phosphoric acid.
Since the bond to enamel is known to be stable over time, unlike the bond to dentin, which degrades over time, it is logical to focus efforts on increasing the strength of contact with this particular structural tissue.
Selective etching
For the above reasons, a combination of selective enamel etching with phosphoric acid and self-etching of dentin is reasonably considered the most suitable option for achieving adhesion. However, the problem remains that through the application or removal of the etching gel, there is the possibility of contamination of the dentin, which in turn leads to a decrease in the effectiveness of the use of acidic primers.
Simply put, given that self-etch systems were developed to reduce bonding steps, such a method defeats the intended purpose of their development.
Self-adhesive cements
Popular self-etch adhesive cements, referred to as "all-in-one" adhesive cements containing acidic primers, do not provide a strong bond to enamel equivalent to that which can be achieved using traditional approaches to adhesive technique (using separate primer and resin cement).
But even with this in mind, it is difficult to find studies that prove that self-adhesive cements are clinically ineffective.
Such cements are practical for indirect restorations, but are not universal. Their use should be based on the characteristics and nature of the preparation of tooth tissue, the quality of the dental substrate and the selected materials that need fixation.
Communication with materials
Up to this point, the discussion has focused on adhesion to dental tissue, but not to restorative or prosthetic materials. Basic materials for direct restorations, such as composites, do not require special attention due to their original chemical compatibility with adhesive systems.
Ceramic materials for indirect restorations, such as silicate-based glass ceramics, polycrystalline ceramics such as alumina and zirconia, and hybrid polymer ceramics, all require specific bonding protocols with the additional use of chemical primers.
To achieve a bond with the ceramics and the quartz glass particles located in its structure, some of them must be dissolved with hydrofluoric acid for micromechanical retention. However, such a bond may not be sufficient to ensure strong adhesion due to the relative weakness of micromechanical retention and the inherent chemical incompatibility between the adhesive composite cement and the glass ceramic.
In this case, silanizing agents must be used as they increase the level of adhesion between the silica ceramic and the resin cement. Silane is a volatile substance with a short shelf life and degrades quickly when exposed to air, so its use must be extremely delicate. It should be noted that its correct use is simply necessary.
Polycrystalline ceramics contain no glass particles and, therefore, micromechanical retention by etching with hydrofluoric acid is out of the question. Bonding of these materials and metal alloys is achieved through chemical bonding alone using primers such as MDP monomer (10-methacryloxydecyl dihydrogen phosphate), which also forms a chemical bond with calcium and hydroxyapatites due to the presence of a phosphate group that enhances bonding strength with tooth tissues. Newer polymer ceramics (Vita Zahnfabrik or Lava Ultimate (3M ESPE)) require the use of silane, and are either etched before use (Enamic) or put through an air abrasion process (Lava Ultimate) to improve adhesion.
Future 2015: All-in-one adhesives
It is obvious that the problem of adhesion in dentistry does not have a single approach to solve all clinical cases, unless, of course, all determining factors are taken into account. But technology does not stand still, and recent developments and advances in chemical engineering are at the forefront of progressive changes.
Self-etching systems remain relevant, total etching systems are “viable”, and self-adhesive composite cements occupy their specific niche. The process of simplifying techniques is still relevant, as is the development of chemical agents for effective adhesion to all filling materials. But what are the real prospects for such improvements, and what is the reliability of their use?
A completely new category of adhesive products, which are superior to all previous ones and are called “universal”, implies the following properties and characteristics:
- all necessary bonding chemicals in all clinical situations are contained in one bottle;
- simple protocol of use for both the doctor and the assistant;
- high adhesion force to any surfaces, be it dental tissues or restoration materials;
- stability in solution;
- remain effective with or without the use of phosphoric acid, depending on where conditions actually allow it;
- extremely low incidence of postoperative sensitivity, regardless of the etching mode;
- low cost as a result of the exclusion of other adhesive systems from clinical practice.
The first product of this type, Scotchbond Universal (3M ESPE), was introduced in early 2012, marking the beginning of the trend toward a “universal” category of adhesives. The number of laboratory and clinical results supporting the belief that bonds in this category represent a breakthrough in adhesive dentistry continues to grow, demonstrating the effectiveness of these simple and effective systems.
At the same time, it should be remembered that the results of laboratory examinations are sometimes very difficult to interpret in relation to clinical results, therefore, the role of long-term practical studies increases.
On the other hand, single-vial chemical agents that have previously been used in rotation and have proven success for many years make it difficult for the clinician to understand the practical application of the concept of “universal.”
Scotchbond Universal and all subsequent products (for example, Adhese Universal, Ivoclar Vivadent; All-Bond Universal, Bisco; Futurabond M+, Voco Dental; Prime&Bond Elect, DENTSPLY) may well change and improve what dentists have been fighting for all these years, especially if take into account the current trend towards their widespread use, based on the results of their effective use both in clinical practice and in laboratory conditions over 5 years.
It is important for dentists to understand that representatives of universal adhesive systems are not identical to each other, and cannot be used in the same way in all clinical situations. There are differences in overall chemical composition, concentration, and recommendations or specific application techniques.
For example, some systems contain HEMA, various solvents, and unique additional constituents such as polyalkenic acid copolymers similar to those found in glass ionomer cements. Some universal bonds react universally with all resin cements in a dual-cure mode, while others require the additional use of an activator.
There are corresponding reasons for such variations in composition and indications, identified by the manufacturers and justified by research results.
However, how to justify the simultaneous need for a universal adhesive and a self-adhesive composite cement for either direct or indirect restoration remains an unresolved question.
To deeply understand the principles of operation of a particular adhesive system, you first need to familiarize yourself with the manufacturer’s website, the technical characteristics of the material, independent user assessments and the manufacturer’s internal data.
This volume of evidence confirming the effectiveness of the universal category of adhesives, compared with the clinical observations of other doctors, requires dentists to review existing bonding protocols, taking into account the duration of their use.
Scientific evidence must provide solid evidence of the quality of each system, taking into account the subtle nuances of each individual product that the physician must take into account. At this stage, dentistry is heading towards a level of reduced risk tolerance, which in turn is good news for both practitioners and their patients.
Author: Daniel J. Poticny, DDS
What are the types of adhesion?
There are several types of adhesion: mechanical, chemical, and their combinations. The simplest is mechanical. The essence of the system is the creation of micromechanical bonds between the components of the material and the rough surface of the tooth. To ensure high quality adhesion, the natural micro-grooves on the surface of the dental tissues are thoroughly dried before applying the adhesive.
Interesting! Dr. Buoncore 63 years ago experimentally discovered that phosphoric acid makes tooth enamel rough. This helps strengthen the adhesion of the composite to the tooth tissue. The technique of etching tooth enamel with acid, which appeared more than half a century ago, became the foundation for modern adhesive restorative methods.
The chemical bonding option is based on the chemical bond of the composite material with enamel and dentin. Only glass ionomer cements have this type of adhesion. Other materials that dentists use have only mechanical adhesion.
How the composite “sticks” to the enamel surface
As noted above, in dentistry the mechanisms of adhesion to enamel and dentin differ. The protective outer shell of teeth is transformed by acids. If you examine the enamel after acid etching under a microscope, it will resemble a honeycomb. In this case, the acid works to strengthen the bond with the composite. As a result, viscous hydrophobic adhesives more easily penetrate deeper layers of enamel and provide strong adhesion to the composite.
Interesting! Enamel is considered the hardest tissue in our body. It contains the largest amount of inorganic substances - approximately 97%. The remaining 2% is water, 1% is organic matter.
How enamel is etched
This processing method involves removing part of a layer of 10 micronewtons (µN) from the enamel. As a result, pores with a depth of 5–50 μN appear on its surface. Often, for etching, enamel is lubricated with orthophosphoric acid, but for dentin, organic acids can be used, but in low concentrations.
The etching process lasts from 30 to 60 seconds. The individual structural features of the enamel surface, in particular its initial porosity, are of decisive importance. If you overexpose the acid, it will inevitably affect the structure of the enamel and weaken the adhesion. So if the patient’s dental tissues are quite weak, then etching should last no longer than 15 seconds. The acid is removed with a stream of water, and for the same amount of time as it is kept on the enamel.
Stages
For high-quality restoration, the working field is isolated from saliva with a rubber dam or other system. Protocol:
- Etching of enamel - 10-15 seconds, dentin - 3-5 seconds.
- Washing off the acid with a stream of water or a water-air spray. Must be equal to or greater than the etching time. By no means less. Do not dry.
- Rinsing the cavity with alcohol (from 70%, preferably 95%) or an alcohol solution of Chlorhexidine from a syringe for 60 seconds. You can rinse one at a time - first with Chlorhexidine, then with alcohol. Dry slightly, you can remove excess moisture with paper pins.
- For 5th generation bond and higher: apply adhesive, rub it into the cavity for 10-15 seconds. Dry slightly. Then a second layer is applied (the same as the first) and blown until the “waves” disappear. For 4th generation bond: apply primer at least 2 times, each layer must be rubbed in and inflated! Apply the bond in the same way.
- Applying a thin layer of flowable composite to the bottom of the cavity.
- Polymerization according to the instructions for the adhesive.
During the adhesive preparation process, the cavity must be constantly moistened! Do not overdry fabrics.
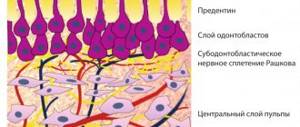
How the composite “sticks” to the dentin surface
The properties of dentin are such that its outer layer is wet. The fluid in this part of the tooth is renewed quickly, so it is very difficult to dry it out. And so that moisture does not affect the quality of adhesion of dentin to the composite, special water-compatible (in scientific terms - hydrophilic) systems are used. Also, the strength of bonds is directly influenced by the so-called “smear layer”, which arises as a result of instrumental processing of dentin. There are 2 approaches to using binding mechanisms:
- the smear layer is impregnated with water-compatible substances,
- the smear layer is artificially dissolved and cleaned off.
It is worth noting that the latter method, which involves removing excess microparticles from the surface of the enamel, is used today much more often than the first.
How dentin is etched
Japanese dentist Fuzayama was the first in history to use the dentin etching technique 39 years ago. Today, before the procedure, special conditioners are applied to the dental tissues - they help hydrophilic substances penetrate deeper into the dentin tissues and adhere to the water-repellent composite. The smear layer partially disappears, the dentinal tubules open, and mineral salts come out of the upper layer. After this, the conditioners are washed off with water. Next comes the drying stage, and the main thing is not to overdo it, otherwise it will affect the clutch.
Next, a primer is applied, which helps hydrophilic substances pass into the tubules and adhere to the collagen fibers. As a result, a kind of hybrid layer is formed, which contributes to the effective bonding of the composite to dentin. It also serves as a barrier against the penetration of chemicals and microbes into the internal structures of the tooth.
4th generation adhesives in dentistry are applied in three stages.
- The dentin of the tooth in the carious cavity is treated with an etchant - most often phosphoric acid. After 15 - 20 seconds, it is washed off with running water, and the treatment area is thoroughly dried.
- The primer is applied for a few more seconds and dried with a thin stream of air. This substance penetrates into the demineralized area of dentin and forms a hybrid layer.
- After this, the surface is ready for the addition of adhesive, which will securely hold the filling. At the end of the procedure, the substance is polymerized using a lamp.
Representatives of 4th generation adhesives are still used in dentistry today. These include products such as Pro Bond from the American brand Dentsply; Scotchbond MP Plus from 3M, another well-known company in the dental market from the USA; Syntac produced by Ivoclar Vivadent, based in Switzerland, and others. These solutions are still considered the standard today.
Further developments have introduced one-component and self-etching adhesives onto the market, which are applied in one step. The latest, seventh generation systems eliminate the occurrence of tooth sensitivity.
Dental adhesive is often confused with composite. However, these two substances have different compositions and purposes. Composite is a type of restorative material that is used in dentistry to restore teeth. It has high aesthetic values and allows you to achieve the desired shade that matches the color of natural enamel. Composite fillings and inlays are fixed using adhesive.
Adhesive systems for enamel
If we are talking about enamel, then adhesion here is ensured on the basis of micromechanical coupling. For this, hydrophobic liquids are used, but they will not provide the necessary “adhesion” to wet dentin, so a primer is also used. Handling enamel adhesives having a one-component composition is based on the following steps:
- etching of enamel with orthophosphoric acid - about half a minute,
- removal of etching gel with a water jet,
- drying enamel,
- connection in the same proportion of substances of the adhesive system,
- introduction of adhesive into the tooth cavity with an applicator,
- leveling it with an air stream.
Only after performing all of the above manipulations does the doctor introduce the composite material.