Most dental patients want to have not just a healthy, but also an attractive smile. Unfortunately, not everyone can boast of this.
Back in 1984, some components that are necessarily inherent in a “beautiful smile” were identified:
- The smile should expose almost 100% of the coronal part of the tooth and the gingival papillae, while the gum itself should not be visible (otherwise, when the gum is exposed, we are talking about a “gummy smile”).
- The gingival contour should be symmetrical, smooth, the edges of the gums at the central incisors and canines should be located at the same level, and at the second incisors - 1-2 mm lower.
- The length of the tooth crown should not be less than 11 mm, and the width should correspond to the “golden ratio”.
- The gum contour should be in harmony with the smile line.
If the patient's smile does not fit into these standards, then it can be significantly improved by changing the edge of the gingival contour and increasing the length of the dental crown.
What is lengthening of the clinical crown of a tooth?
Lengthening the crown of a tooth is a tooth-preserving dental intervention, as a result of which the required amount of subgingival tooth tissue is exposed and a new gingival contour is formed.
A radical alternative to this manipulation is to remove the problematic tooth and install an implant of the required length in its place, forming the most aesthetically pleasing gum contour. But do not forget that not a single most beautiful artificial tooth can compare in functionality with your real teeth, so resorting to such a radical method is only in exceptional cases.
Short review
This article examines the concept of biological width, particularly its clinical implications for treatment options and decision making in light of modern dental treatment approaches such as the biometric approach and minimally invasive procedures. Previously, due to the need to maintain the principle of maintaining biological width, clinicians needed to excise periodontal tissue, bone and gingiva around deep cavities so that the boundaries of the restorations were located at a distance from the epithelial and connective tissue attachments, thereby preventing tissue loss, root exposure, and proximal opening ( leading to the formation of black triangles) and deterioration of aesthetics. In addition, no material was placed in the subgingival area if this would result in periodontal inflammation and loss of attachment. Today, with a more conservative approach to restorative dentistry, previous resective procedures are being replaced by additive ones. In this regard, subgingival margin elevation (DME) instead of surgical coronal lengthening could be proposed as a paradigm shift in the treatment of deep subgingival caries cavities. The purpose of this study was to review the literature in search of scientific evidence on the effects of subgingival margin elevation using different materials, especially the effect on the surrounding periodontal tissue, from a clinical and histological point of view.
A new approach is to extrapolate results obtained during root recession closure procedures on restored roots to suggest tissue healing patterns at the proximal attachment on composite resin placed using an adhesive protocol when raising the deep subgingival margin. The three clinical cases presented in this article demonstrate these procedures. The premise of this study was that although surgical coronal lengthening is a useful procedure, the indications for it should decrease over time given that although deep subgingival margin elevation is a difficult procedure, it is well tolerated by the surrounding periodontal tissues clinically and histologically.
In what cases is it necessary to lengthen the clinical crown of a tooth?
Lengthening the clinical crown of a tooth may be prescribed to a patient for the following reasons:
- Aesthetic
- "Gummy" smile.
- Violation of the gum contour of one or more teeth.
- The natural crowns of the teeth are too short - after eruption the gums did not rise and remained “lowered” on the tooth.
- Under-eruption of one or more teeth in the dentition.
- To improve dental hygiene.
- Tooth-preserving
- The need to restore the length of teeth that was lost as a result of pathological abrasion (bruxism, increased tone of the masticatory muscles can lead to this).
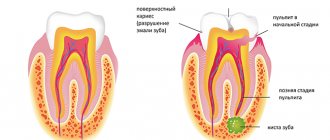
- The presence of caries in the subgingival part of the tooth, i.e. below the gum line.
- The need to carry out and maintain high-quality tooth restoration using any of the methods, because to maintain periodontal health, such restoration should not go below the gum level.
- For high-quality prosthetics, in case of complete destruction of the tooth crown, for reliable “full” capture of the hard tissues of the tooth and to prevent future problems with the crown.
- As one of the components of complex surgical treatment of periodontal diseases for the removal of periodontal pockets.
Methods for lengthening the clinical crown of a tooth in modern dentistry
In modern dentistry, there are 4 methods of lengthening the clinical crown of a tooth:
- Orthodontic – involves “pulling” a tooth from the bone using a brace system, which can be installed on several teeth or on the entire jaw. This method is used when there is free space between antagonist teeth, mainly to lengthen the crown of one “under-erupted” tooth, the length of which differs from the rest. The disadvantage of this method is the need to wear braces, a long treatment time - 2-3 years, and the presence of a retention period.
- Surgical - is an operation to remove part of the gum and/or bone and give a new shape to the gingival contour. The main types of surgical intervention are gingivectomy or gingivoplasty, as well as bone resection.
- Orthopedic - involves building up the crown of a tooth using orthopedic structures - veneers/lumineers or dental crowns, due to the installation of which the bite is raised, i.e. the tooth is lengthened from the cutting edge, without involving the gingival zone. This method of lengthening dental crowns is used in the presence of an erased cutting edge and in the restoration of significant defects in damaged and chipped teeth. The doctor will also choose this technique if the patient has short teeth, but at the same time an ideal gingival contour.
- The therapeutic method is composite augmentation of the incisal edge. Effective for minor chips and chips on single teeth.
This technique is used to “raise” the gum level when correcting a gummy smile, and before caries treatment and restoration that need to be performed below the natural gum level.
What does a patient need to know about lengthening the clinical crown of a tooth?
In order for the tooth crown lengthening procedure to be successful, it must be carefully and comprehensively planned - this applies to all methods of its implementation. In planning such treatment, depending on the chosen intervention technique, several specialists will take part - a periodontist, a dental surgeon and/or an orthodontist, a dental therapist and/or an orthopedic dentist.
When planning to determine the volume and type of intervention, the following are taken into account:
- Current and future health status of periodontal tissues.
- The proportions of the tooth itself, the aesthetics of the patient’s smile.
- The structure of the roots of the tooth and the ratio of the length of the root and crown. It is IMPORTANT that its root part is no less visible.
- Condition of the jaw bone.
- Biological width is the distance from the bottom of the gingival sulcus to the crest of the tooth-bearing bone, and in order for the tooth to be stable in the future, its value must be at least 3 mm.
Therefore, lengthening the clinical crown of a tooth requires a very careful diagnosis, because the procedure should not disrupt the stability of the teeth on which it will be performed.
Diagnostics before tooth crown lengthening includes:
- Assessment of periodontal condition (diagnosis by a periodontist).
- Diagnosis by a surgeon – if a surgical lengthening method is proposed.
- Consultation and diagnosis with an orthopedist – in case of need for extensive restorations, prosthetics or the use of an orthopedic lengthening method.
- Consultation with an orthodontist and orthodontic diagnosis, if the crown will be lengthened by installing a brace system
One of the mandatory studies during diagnosis will be a 3D CT scan - computed tomogram, to determine the length, location of the tooth root and the condition of the jaw bone tissue.
Lengthening the crown of a tooth
The positive result of prosthetics largely depends on proper treatment and treatment of periodontal tissues. If the edges of artificial crowns are placed apical to the gingival margin, this can lead to damage to the periodontal ligaments. To avoid this problem, they resort to an operation to lengthen the tooth crown, which makes it possible to bring the edge of artificial crowns coronal to the gingival edge or to its level.
An operation to lengthen the crown of the tooth is required before prosthetics, which may be due to the specific structure of the dentogingival system.
The dentist must determine the height of the bone crest and the width of the gingival attachment before taking impressions and making artificial crowns to prevent violation of the biological width.
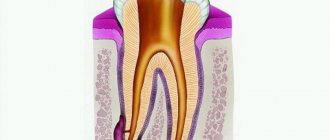
Biological width is the complex of gingival tissues around the tooth, which is located above the alveolar bone. For the first time, the dimensions of biological width were established by Gargiulo A. et al. As a result of the studies, the average dimensions of the biological width were recorded, which consists of attached connective tissue of 1.07 mm and attached epithelium of 0.97 mm, which is 2.04 mm. The size of the gingival groove was 0.69 mm and some scientists include this size in the biological width.
What can happen when placing the crown margin within the biological width? If the alveolar bone is too thin, bone atrophy and gum recession may occur with restoration of normal biological width. If the edge of the crown is located deeper, then constant inflammation of the gum tissue occurs while the level of bone tissue is preserved.
Crown lengthening is a surgical procedure that involves releasing enough tooth structure to allow adequate tooth restoration.
An operation to lengthen the crown of a tooth is also performed for cosmetic defects. Such defects include:
- unhealthy gum condition, when the aesthetics in the area of the front teeth are impaired, i.e. the gingival contour is uneven and asymmetrical;
- exposure of a large area of gum when smiling (“gummy smile”), when the crowns of the teeth appear short.
The method of lengthening the coronal part of the tooth allows you to move the gum surrounding the tooth and the underlying bone in the coronal direction. Then the gum edge is given the correct physiological shape. Moreover, after the operation the ratio of the crown and root parts of the tooth practically does not change.
Before the operation begins, it is necessary to conduct a thorough diagnosis, which includes determining the depth of the periodontal pockets and x-ray examination to determine the shape of the root and its position in the bone. Pay attention to the patient's smile line.
+7
Back call
Working hours
| Mon-Fri | 10:00 — 22:00 |
| Sat-Sun | 10:00 — 20:00 |
Ivanova Yulia Evgenievna Cosmetologist - esthetician
LATEST ARTICLES
Sinus lifting in dentistry: risk or help? Bone grafting during implantation: indications, types Hemisection of the tooth: indications, methods of implementation Methods for lengthening the coronal part of the tooth Painless removal of baby teeth
What awaits a patient undergoing a clinical crown lengthening procedure?
Read about the orthodontic, orthopedic and therapeutic method of lengthening the crowns of teeth in the relevant sections - on orthodontics (installation of braces), prosthetics with crowns and veneers, and restoration. In this article we will focus on surgical lengthening of the crown of one, and more often, several frontal teeth.
Basically, in this case, they resort to gingivoplasty - a surgical operation during which part of the gum is removed along the gingival contour, often this intervention also requires the removal of part of the bone.
This manipulation is performed by a dental surgeon in a surgical office, on an outpatient basis, under local anesthesia and, sometimes, sedation.
Such an operation is prescribed after a thorough diagnosis, in most cases - as a stage in complex treatment and the formation of an aesthetic smile.
- Before any surgical intervention, professional hygiene and sanitation of the oral cavity are carried out to reduce infection in the oral cavity and speed up healing.
- The patient is given anesthesia.
- After which, if resection (removal) of a part of the bone is required, the mucoperiosteal flap is peeled off and an osteotomy is performed. A new gingival contour is formed, which is located above the previous one.
- The wound is sutured and a gum bandage is applied.
- In the postoperative period, for a speedy recovery, the patient is prescribed antiseptic rinses and painkillers, and a course of antibiotics may be prescribed. It is necessary to limit physical and chewing activity.
- The stitches are removed after about 7-10 days.
- Immediately after the wound has healed, a temporary restoration or prosthetics is performed, and after a few months the temporary structures are replaced with permanent ones.
- Complete restoration of the new natural gum margin occurs in 1-3 years.
What type of connection does Biological Width like?
What is the difference between implants and teeth?
What is “platform switching” and why is it needed?
I’ll say right away that BS doesn’t like connections at all. And in this sense, all implants can be CONDITIONALLY divided into 2 large groups:
one-piece implants
– solid implants or so-called ITI implants, Straumann
two-piece implants
– consisting of two parts – these are all the rest
This division has been formed since the very first days of the development of modern implantology. Brannemark and his group in Sweden came up with an implant consisting of 2 parts, and the group of prof. Schröder, completely in parallel, developed a one-piece implant in Switzerland, which became the prototype of the modern Straumann implant
Numerous studies show that after installing an ITI implant with a rough part below the bone crest and a polished part above it, the biological width is formed within 6 weeks and, in its anatomical and digital values, is almost identical to that of a natural tooth. And most importantly, it is stable for a long time - after 0.5 years, and after 1 year, and after 15 years. The only parameter that sometimes changes its values is the depth of the sulcus - it decreases from 1.5-1.0 mm to 0.8-0.5 mm within 1 year.
And if we try to answer the question in the title of the topic, then this is the design where the connection with the abutment and crown is located ABOVE the biological width, this is exactly the design that BS “loves”.
How is the BS formed on implants of the Brannemark type or consisting of 2 parts? And there are 2 answers to this question, depending on what type of healing is chosen after installation of the implant.
Option No. 1 - as it was done, basically, before - by submersion, with complete suturing of the edges of the wound over the implant and closing the shaft with a screw and plug for the period of osseointegration of the implant. And after 3-6 months, the implant is opened and the gum former is installed. In this case, the SB will begin to form only after the implant is opened, i.e. in 3-6 months.
The picture below shows a classic scheme for forming a BB on a Brannemark-type implant using a 2-stage protocol. Left - Installation of the implant and suturing tightly. After 4-6 months, the implant is “opened” and the former is installed. On the right is a view one year after implant placement and final prosthetics.
Here we come to the most important function of the dentogingival junction or JJ. This function is protective, separating sterile bone from the non-sterile environment of the oral cavity. And as we know today, the process of formation of SB starts in the presence of a stimulating effect of the aggressive environment of the oral cavity, i.e. In order for the formation of BS to begin, the implant should be carried out according to the 2nd type of healing, namely No. 2 in a non-immersed method with partial suturing of the wound and installation of gum formers immediately during the operation.
How and where the BS is formed on different systems depends on the type of two-part implant and the shape of its neck. Research and development in this area is ongoing and a final “ideal” solution has not yet been found.
To understand the process of formation of bone marrow, in addition to the above knowledge and concepts, it is also necessary to understand that depending on the surface roughness, bone and soft tissue will behave differently. Today we mainly encounter a minimally rough (0.5-1 micron) surface - this is how it looks after milling - this is what all the first implants were like, and a moderately rough (1-2 micron) surface - this is what the surface looks like after sandblasting coarse sand and etching. There is also a coarsely rough one (the middle one in the picture), but today this is no longer relevant. And there is polished - this is when it shines like a mirror.
The BS preference table looks something like this:
Sulcus - it forms on both the polished and rough parts, but it is healthy only on the polished part. It is known that this part of the BS is variable and more predictable on a milled and polished surface.
The epithelial attachment is the most unstable element of attachment in terms of size - it can be 1 mm, or maybe 6 mm. The best texture for EP is milled, then polished and medium rough. Very bad - coarsely rough.
Connective tissue attachment is the most stable element of the BS! It is this that determines the quality of “sealing” and delimitation of two environments. Practice shows that fibers are better attached to a moderately rough surface and it is on this surface that perpendicularly oriented fibers are found. SP also favors the milled part and does not “like” the polished part at all.
Osseointegration occurs best and fastest with a medium rough surface.
The bone does not “grow” to the polished surface!
What is the difference between implants and teeth?
What is “platform switching” and why is it needed?
Contraindications to lengthening the clinical crown of a tooth
In some cases, after weighing all the pros and cons, the dentist may refuse to lengthen the patient’s dental crowns.
The following reasons may serve as the basis for this:
- After tooth crown lengthening, the appearance and health of adjacent teeth will deteriorate.
- Regardless of the lengthening, restoration of this tooth is still impossible.
- Insufficient biological width.
- A tooth with a short crown has a short root.
- During orthodontic lengthening, there is no space between the tooth that is planned to be lengthened and the opposing tooth.
- The ratio of the effort required to lengthen the crown of a tooth and its value is not in favor of preserving the tooth.
- The patient is unable to maintain the required level of periodontal health.