Diagnostics
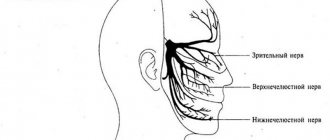
The neurologist makes a diagnosis based on the clinical picture, the patient's medical history, the results of a neurological examination and a physical examination. The doctor must rule out diseases that may manifest as facial pain (herpes, headaches). An accurate diagnosis is necessary in order to choose the right tactics for treating neuritis. With neuritis, palpation of the exit points of the trigeminal nerve is accompanied by painful sensations. Diagnosis includes MRI. This is necessary in order to exclude tumors and demyolinating diseases. The diagnosis can be confirmed by the positive effect of low-dose anticonvulsants or tricyclic antidepressants.
Possible complications during the development of wisdom teeth dystopia
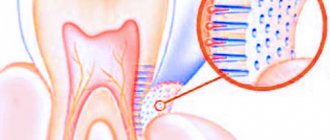
Third molars are extremely problematic teeth. If teething occurs with tolerable pain and the patient does not rush to the dentist, then the following complications are possible:
- Pericoronitis – inflammation of the gum mucosa;
- A follicular cyst is a “sac” of fluid pressing on the roots;
- Periostitis is inflammation and suppuration (abscess) of the periosteum.
The appearance of these complications will lead to longer, more painful and expensive treatment, so you should not put off going to the doctor if you feel that your wisdom tooth has begun to erupt.
Treatment of trigeminal neuropathy
Treatment may include drug therapy, surgery, and complex treatment.
Drug therapy is aimed at relieving pain symptoms. Treatment can be long-term (six months or more).
Drugs for the treatment of trigeminal neuritis:
- antiepileptic drugs (carbamazepine, pregabalin, gavapentin), prescribed to reduce pain
- muscle relaxants
- tricyclic antidepressants in small doses (amitriptyline)
- B vitamins (B1, B6, B12)
- antihistamines
- antibacterial (if there are contraindications)
- NSAIDs (non-steroidal anti-inflammatory drugs)
- sedatives
- antiviral drugs (if there are indications for their use).
Physiotherapeutic methods can be used to treat pain:
- antiepileptic drugs (carbamazepine, pregabalin, gavapentin), prescribed to reduce pain
- UFO, UHF
- phonophoresis with anesthetic (lidocaine)
- diathermic currents.
Treatment is carried out on an outpatient basis, sometimes peripheral nerve root blockade is used, but it does not always have a positive effect.
According to indications, radiosurgery and the Gamma Knife technique can be used, but in this technique the treatment result appears after 4 months or more.
One of the last treatment options may be the destruction of the trigeminal nerve - rhizotomy.
Possible complications
There are several reasons why complications arise after the removal of the eighth molar: improper oral care, inexperience or negligence of the surgeon, complex removal with severe trauma to the gums. The most common complications include:
- Paresthesia.
If the nerve endings are damaged, the cheeks, lips, tongue and chin become numb. Possible diction problems. Symptoms may last up to two weeks.
- Alveolitis.
The most common complication after removal of the eighth molar. Development is provoked by an incompletely removed tooth or an open socket, without a blood clot. The “true friend” of such a complication is bad breath, which does not go away for a long time.
- Hematomas.
The reasons for the appearance are damaged blood vessels during removal.
- Flux.
If hygiene is not observed, bacteria enter the wound, which provokes inflammation of the periosteum. Symptoms: pain, fever, redness and swelling of the gums.
If severe pain after the removal of a wisdom tooth does not subside, but rather intensifies, symptoms such as swelling, bruising and edema progress - this is already a pathological process that requires the intervention of a specialist.
Prevention
Prevention measures:
- balanced diet;
- limiting alcohol consumption, quitting smoking, reducing factors that lead to intoxication of the body;
- active sports;
- do not overcool;
- increase stress resistance;
- avoid injury;
- timely treatment of respiratory and infectious diseases;
- preventive examination at the dentist several times a year, dental treatment;
- timely contact a neurologist if pain occurs.
Extraction (removal) of wisdom teeth
Horizontal growth of the extreme molar is a situation where the only correct solution is often its removal. The intervention of a dental surgeon helps to avoid serious consequences caused by abnormal dental growth. The extraction itself goes like this:
- Anesthesia. Having determined the position of the tooth, the doctor selects the appropriate anesthesia: local in mild cases or general anesthesia if serious surgical intervention is necessary.
- Antiseptic treatment. The surgical field is prepared - the gums and teeth are treated with an antiseptic solution that will destroy all bacteria and microbes living in the oral cavity.
- Gum cutting. Using surgical instruments, a flap of soft tissue is carefully cut and peeled off from the neck of the tooth, root and bone. After the operation, the gum is returned to its place and fixed with sutures.
- Molar extraction. Using forceps and an elevator (a specially shaped wedge), the tooth is loosened and removed from the socket. If a piece of the root breaks off during removal, then an excavator (special medical hook) is used.
- Processing the hole. After removing the molar, the doctor examines the resulting hole and treats it with special drugs that prevent infection.
- Stitching. The cut gum is held together using medical materials, which after some time dissolve on their own, leaving behind fused soft tissue.
Traditional medicine recipes
To treat the trigeminal nerve, doctors recommend trying special recipes from traditional medicine. Of course, they cannot help everyone and at the same time they will only relieve pain, but will not cure it completely. Therefore, if you experience any pain, you can try to relieve it at home and immediately go to the dental clinic for help.
So, the following recipes can help relieve pain:
- Compresses from boiled beets, which are grated on a coarse grater, add black radish juice and use the resulting mass to make a compress on the trigeminal nerve.
- Make a rinse using an infusion of chamomile and honey. Rinse your mouth with the prepared solution.
- Lotions made from horseradish grated on a coarse grater. You need to wrap the resulting mass in a clean cloth and apply it to the place where the pain occurs.
If pain occurs in the temporal part of the face, you should immediately make an appointment with a neurologist, who can determine the cause of the trigeminal nerve disease and prescribe appropriate treatment.
Simple and complex removal
How complex the operation will be directly depends on the location of the eighth molar, the correctness of its growth, the complexity of the root system and the integrity of the tooth being removed. For example, if there is severe caries damage, the doctor will have to cut it into several pieces and only then remove it.
Easy removal
Simple extraction is the extraction of a tooth using forceps, without the help of any other dental instruments. During a simple extraction, the molar is easily removed from the gums, usually without complications. Most often, figure eights of the upper jaw are removed this way, because they are clearly visible and their roots are located exactly in the gum. In rare cases, there is a problem with the removal of upper molars. Accordingly, tissue regeneration also occurs quickly. On the 3-4th day, instead of a blood clot, young connective tissue forms, after 2-3 weeks filling the entire depth of the hole. On average, bone tissue is formed after 3 months.
Complex removal – what to expect?
Complex removal is one that requires drilling out the jawbone or cutting through soft tissue. This is mainly required when extracting figure eights from the lower jaw, since the root system here is more complex. Often there is abnormal growth (impacted or dystopic tooth), in which case only complex extraction is indicated. In the area of the lower jaw, the vessels pass close to the root system and there are more nerve endings, so it is always more difficult to remove lower molars. If the doctor considers it necessary, stitches are applied after the operation.
How long pain and healing last after wisdom tooth removal depends on the following factors: the presence of an inflammatory process during the procedure, the complexity of the operation, the degree of trauma after removal, the characteristics of the body, proper hygienic care, and taking medications after surgery. A timely operation is accompanied by rapid tissue regeneration, without the need for antibiotic therapy.
Attention! A wisdom tooth hood is a soft tissue that covers an impacted tooth. This is an “extra” formation in the oral cavity, and it is very important to remove it before inflammation begins. The hood is an additional source of inflammation. If it is not excised in time, an inflammatory process may begin and antibiotics may be required.
Types of jaw nerve injuries
- Neuropraxia is a minor injury: benign course, favorable prognosis. In the absence of damage to the integrity of the nerve bundle, independent regeneration occurs within a month and a half.
- Axonotmesis is partial degeneration of the myelin sheath: restoration of nervous tissue is incomplete, possibly 1.5 months after damage. Medical attention is required.
- Neurotmesis - complete damage: degenerative changes in biophysical, biochemical parameters of nervous tissue. The prognosis is poor: high risk of irreversible loss of sensitivity .
Therapy results
The prognosis of microsurgical and therapeutic treatment is influenced by:
- age, health status of the patient;
- skill and experience of the surgeon;
- the duration of the period between injury and surgery.
In 80% of cases of neurotmesis operated on in the first 5 months after injury, partial restoration of the function of the mandibular nerve was observed. Delaying surgical intervention systematically reduces the chance of recovery. Seeing a neuromicrosurgeon a year or more after injury has only a 10% chance of success.
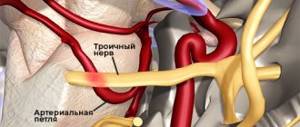
Causes of inflammation
The installation of a dental implant should be carried out taking into account the parameters of the jaw, size, characteristics of the alveolar process and bone tissue of the implanted area. The relief of the canal through which the mandibular nerve bundle passes must be thoroughly studied.
Lack of preparation for implantation and lack of professionalism are the main causes of damage to the mandibular branch.
You can touch or damage the neurovascular bundle:
- needle during anesthesia;
- direct pressure with a long implant;
- tool when forming a dental bed.
Damaging factors include a long period of flap retraction and bone graft harvesting. Restoring sensitivity is a long and problematic process; the task of implantologists is to reduce potential risks to a minimum .
Symptoms of the lesion
You can assume that the mandibular nerve is affected by the following signs:
Numbness of the face and pain symptoms are signs of damage to the mandibular nerve
- numbness of the face from the implantation side: lower lip, chin, tongue, lower teeth, cheeks;
- pain in the implant area;
- the appearance of profuse salivation;
- choking when eating or drinking;
- the occurrence of facial expression and articulation disorders.
A person feels discomfort when caring for facial skin (unpleasant sensations during shaving, applying makeup). Clinical manifestations depend on the type of injury and the depth of the lesion.