Root cysts or gingival granulomas are a common problem today. Neglect of regular examinations, hygiene rules, the development of caries or periodontitis contribute to the development of cystic formations. The disease affects all segments of the population, regardless of gender and age. In fact, it does not matter on which jaw a radicular cyst occurs, because the process of appearance, treatment, and consequences develop according to the same scenario. To eliminate pathology, there are a number of new techniques that can completely eliminate the disease with a guarantee of no relapses.
Radicular cyst as a disease
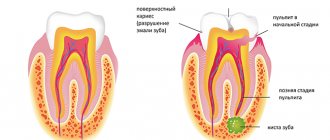
Cyst translated from Greek means “cavity”, “bubble”. In medicine, this bladder is often filled with blood, organic fluid or purulent exudate. The outer layer of the cystic component consists of soft connective tissue, and the cavity itself is filled with epithelium. Diagnosis of a radicular cyst is carried out specifically in the upper segments of the jaw bone. Detection of its signs in the lower jaw is quite rare. At the very beginning, the disease occurs in a latent stage and does not manifest itself in any way. If detection occurs, it is usually through an X-ray of a completely different dental area. Based on size, dentists distinguish two groups of cysts:
cystogranuloma (about 0.5 cm); cyst (more than 1 cm).
Radicular cysts of the jaws (lower or upper) are cavity neoplasms in the periapical dental area with cystic fluid, formed as a result of the inflammatory process of the periapical (root) part of the tooth. There are main forms of the disease:
acute process; chronic form.
Prolonged growth of the cyst can lead to gradual perforation or thinning of the jaw bone, which increases the risk of jaw fracture in the affected segment. A radicular cyst often requires surgical treatment, so if unpleasant symptoms are detected, a visit to the doctor is urgent.
Etiology and provoking factors
The appearance of a cystic component is the body’s response to the inflammatory process in the tooth. Cysts form in patients with a long course of carious destruction, when the lesion reaches the root part of the tooth. But there are other diseases or conditions that can serve as a trigger for the formation of cavity formations:
chronic periodontitis; severe pulpitis; trauma to the tooth and gums: previous illness of an infectious nature; chronic stomatitis; inflammation of the maxillary sinuses; abnormal bite; catarrhal otitis; diseases with a pronounced decrease in immunity; complication during the eruption of wisdom teeth.
A radicular cyst of the maxillary bone is most often formed under the influence of a long-term untreated carious tooth. Sometimes the cause of the appearance of a radicular cyst in the upper jaw is unprofessional treatment of caries, violation of canal filling technology, or lack of competence of a specialist in the treatment of chronic forms of periodontitis. Lack of treatment for a radicular cyst can lead to serious complications not only from the maxillofacial anatomical zone, but also from all organs and systems of the body as a whole.
Clinical picture
The development of the cystic component can develop for about several years and does not manifest itself symptomatically. If unexpressed but unpleasant signs of a cyst appear, treatment should be carried out immediately, since treatment of the tumor after its significant growth will be quite difficult. As the cyst grows, it puts strong pressure on the surrounding connective tissue, so its growth is rapid. In the photographs, the cyst looks like a small spherical formation. The main manifestations are:
the appearance of severe throbbing pain; swelling and redness of the gums in the affected area; feeling of tooth mobility; feeling of fullness in the apical space; bad breath: prolonged persistence of low-grade body temperature.
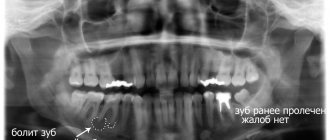
An early cyst can be diagnosed by X-ray examination, and later stages of development are detected by visual examination of the patient’s oral cavity. Usually the suspicion of the presence of a cystic cavity is justified.
Diagnostic methods
After the patient contacts the dentist, a planned additional examination is prescribed, which will help identify the dental cyst in the upper jaw from other maxillofacial tumors and pathological changes. Among the main ones it is worth highlighting the following:
X-ray examination. On an x-ray, the cyst appears as a small oval or spherical shadow with clear outlines. The shadow is located at the top of the tooth root closer to its side. The periodontal gap is not displayed on the image, but significant destruction of the bone structure in the affected area is detected. Electroodontometry. The method is used when it is impossible to differentiate a radicular cyst on an x-ray. The excitability threshold of the affected tooth varies from 90 to 120 μA. Such indicators correspond to necrotic development of the pulp. Puncture. A puncture with a thick needle is performed to reliably exclude the malignancy of the cystic component. The contents of the cyst are sent for cytological examination.
A radicular cyst of the lower jaw bone is almost no different from the flow in the upper segments of the jaw. Often a radicular cyst is similar to osteoblastoma, but the main difference between a cyst is the absence of a cellular structure and the presence of clear contours of shadows in the projection image. Differential diagnosis allows you to reliably identify the disease and treat it according to accepted medical tactics.
Types of cysts
Root cyst
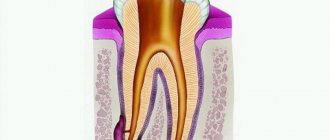
Develops from granuloma as a continuation of pulpal necrosis (death of pulp tissue) and as a result of periapical inflammation. It is located in the apical (apical) third of the tooth root and sometimes has a transverse orientation due to additional canals, the initial paths for the spread of pulpous necrosis.
Root cysts are radiolucent capsules with well-defined boundaries. They can vary greatly in size from 2-3 mm to 2-3 cm. In the absence of secondary inflammation, the roots develop asymptomatically. Even the largest neoplasms do not displace teeth or expand bone tissue.
Once diagnosed, treatment requires eliminating the underlying cause. The most common treatment for pulp necrosis is endodontic treatment. If it is unsuccessful, a decision is made on surgical curettage or enucleation.
Residual
Remains after removal of the pathology. It can form in the granuloma left after tooth extraction or around the left apex of the root.
The residual cyst is clearly visible on x-ray. Its dimensions range from a few millimeters to several centimeters.
Follicular cyst on the gum
A cyst in the gum develops from a follicular sac that encloses each unerupted tooth. This is a capsule clearly visible on an x-ray, most often surrounding the crown of an unerupted tooth. May cause extensive tooth damage. It has a rapid growth rate, can move to adjacent teeth and lead to expansion of the cortical plate.
Clinically, a follicular cyst always occurs in the area where the enamel meets the cementum of the tooth (the place of attachment of the follicle). Due to its growth, adjacent teeth may tilt, and in rare cases, resorption (destruction) of tooth roots occurs. Unerupted teeth can also become displaced due to aggressive growth. If a follicular neoplasm has been identified, its treatment may include surgical curettage (curettage).
Eruption cyst
This is a fluid-filled follicular sac that usually occurs during teething. It covers the erupting tooth and often contains blood. Outwardly it looks like pronounced swelling of soft tissues of a bluish color (due to the presence of blood). Most often it occurs due to slow tooth eruption and can rupture spontaneously. However, in some cases where it is found, treatment may include surgical resection to help the tooth erupt faster.
Primordial (keratocyst)
Develops from the tooth germ as a result of degeneration of the stellate reticulum during tooth development before the onset of calcification of its tissues. Keratocysts can arise from any developing tooth germ, but most often they are localized in the area of premolars and the third molar of the mandible.
Clinically very prone to relapse. If the patient is diagnosed, treatment consists of careful curettage and close follow-up to ensure early detection of recurrence of pathology.
Lateral periodontal
The exact reasons for their occurrence are not fully known. They are rarely large. They are clearly visible on an x-ray and are most often closely associated with the lateral surface of the tooth root. Typically, teeth associated with these cysts have normal pulp. When a lateral periodontal neoplasm (cyst) is detected on the root of a tooth, treatment consists of surgical curettage without compromising the integrity of the tooth. It is important that the removed tissue is sent for histological analysis to rule out more serious pathologies such as early adamantinoma.
Calcifying odontogenic
Their etiology is also completely unknown. They can be found in any area of the supporting surface of the jaws, most often in the lower part. Morphologically they are quite diverse. Clearly visible on x-ray and may contain various opacities depending on the degree of calcification of the tumor. Once diagnosed, treatment consists of surgical curettage or resection.
Treatment process
Treatment of cysts can be therapeutic (conservative) or surgical. The treatment method is determined by the doctor after a visual examination of the oral cavity and the results of diagnostic studies.
Laser treatment
Laser beam treatment is gaining increasing popularity in dentistry. Under the influence of a laser, a tumor can be removed completely painlessly, without the risk of infection. In addition, the laser completely disinfects the affected channels and ensures rapid recovery. The laser treatment algorithm looks like this:
opening and expansion of dental canals; introduction of a laser beam into the canals: disinfection and removal of the cystic component.
The only disadvantages of the method are the relative high cost and the need for special high-precision equipment. Laser treatment also involves following the doctor’s recommendations immediately after the procedure (rinsing with an antiseptic and abstaining from food for up to 5 hours).
Conservative treatment
Therapy for a cystically altered tooth root requires disinfection, tooth cleaning and filling. An alternative treatment method is the introduction of a therapeutic suspension containing copper and calcium, followed by exposure of the tooth to low-power electrical discharges. The main indications for drug therapy are:
absence of fillings on root canals; poor filling in the root canals (not along the entire length); The size of the cyst barely reaches 8 mm.
In treatment, special drugs are used that negatively affect the cyst capsule and its contents. After which, the purulent exudate is completely removed, and instead of it, dental paste is injected into the cyst cavity to restore the bone structure. The manipulations are completed by filling the canal and crown. Cases of relapse of the disease are possible.
Operative method
Surgical treatment is carried out in some cases, since in 80% of cases a radicular cyst is an advanced process. The main indications for surgical intervention are:
presence of a pin in the root canal; early prosthetics of the causative tooth; the size of the cyst exceeds 8–8.5 mm; gum swelling and pain.
Until recently, the cystic component was removed along with the tooth. Alternative methods of surgical treatment are now being used to preserve the natural tooth. A tooth is removed only when the roots of the tooth have become part of a cystic structure or have been destroyed to the very root as a result of disease.
Main methods of surgical treatment:
| Cystectomy. | It is a complex but most effective method of cyst removal. The cavity is completely removed along with the damaged part of the root and the membrane. Indications for surgery are the rapid development of a tumor in the upper jaw to large sizes. |
| Cystotomy. | The procedure involves removing the anterior wall of the cystic cavity. The operation is performed in case of severe destruction of the bone floor of the nose, palatine plate, or with a large cyst. Cystotomy has the longest recovery period. |
| Hemisection. | The simplest method involves removing not only the cyst, but also part of the tooth root, the tooth itself or part of its crown. |
The postoperative period can take a long time. For the entire recovery period, antiseptic rinses are required, and sometimes antibiotics are required. You should not take aspirin, as it provokes bleeding. Recovery takes about a day, and swelling and slight soreness persist for several more days. If unpleasant symptoms persist or their intensity increases, it is important to immediately consult a doctor.
Traditional methods of treatment
Separately, it is worth mentioning the possibility of treating a tumor of the apical part of the upper jaw tooth with traditional healing recipes. Infusions of herbs, compresses and various poultices are good when the patient is in the postoperative period. Herbal treatment for tooth root cysts helps only as a local disinfectant along with traditional treatment methods. There are main herbs that heal gums faster:
Oak bark; pharmaceutical camomile; swampy cudweed; plantain and others.
If you start treatment only with herbs and compresses, you may not only fail to help your body cope with the cyst, but also lead to complications in the form of rupture of the cystic contents. Purulent exudate quickly spreads through the bloodstream and carries all bacterial microflora to vital organs.
Treatment
Treatment is surgical. Only with a small (up to 8 mm in diameter) radicular cyst (cystogranuloma) is it sometimes possible to cure it by filling the tooth canal with cement (see Filling teeth) with the obligatory removal of cement beyond the apical opening into the cavity of the cyst.
The operations consist of either complete removal of the cyst with its membrane (cystectomy), or partial excision of the cyst membrane and the formation of a connection with the oral cavity (Cystotomy). Cystectomy is indicated for cysts that are a malformation of odontogenic epithelium. Cystotomy can be recommended only for cysts of inflammatory origin (radicular), or as a temporary measure for a large follicular cyst, when complete enucleation of the cyst is associated with the risk of damage to adjacent cavities (maxillary sinus, nasal passages) or exposure and damage to the neurovascular bundle on the lower jaw. As a rule, the operation on the upper jaw is performed under infiltration anesthesia, and on the lower jaw - under conduction anesthesia. During surgery in the area of incisors and canines on the lower jaw, infiltration anesthesia can be performed (see Local anesthesia). Before the operation, using electroodontodiagnosis, it is necessary to determine the vitality of the pulp of the teeth adjacent to the 3rd junction. If a cystectomy is planned, then the teeth located within the boundaries of the 3rd junction, projected on the radiograph against the background of the contours of the cyst, must be depulped and their canals sealed with cement.
Rice. 4. Schematic representation of some stages of cystectomy: a - line of an arcuate incision (black) in the area of the cyst; b — the mucoperiosteal flap is detached; c — the bone wall is removed, the cyst shell is peeled off; d — cyst removed, root apex resected; the mucoperiosteal flap is sewn; 1 — mucoperiosteal flap, 2 — bone wall, 3 — cyst shell, 4 — root apex, 5 — sealed tooth cavity.
Cystectomy
Surgical access is usually from the oral cavity (Fig. 4). A semilunar or trapezoidal mucoperiosteal flap is cut out in the area where the cyst is located, the base of which should be facing the body of the jaw. The mucoperiosteal flap is peeled off, the exposed bone is trepanned with a spear-shaped bur, cylindrical cutter or chisel, then the entrance to the cyst is expanded with bone cutters. The cyst shell is peeled off with a curved rasp. The roots of the teeth facing the cyst cavity are subject to resection. The bone cavity is washed with hydrogen peroxide and antiseptic solution. Sometimes filling the bone cavity with a hemostatic sponge, a spongy substance of preserved homobone, is used, which, according to some authors, accelerates the process of bone formation. The mucoperiosteal flap is fixed with several sutures of thin suture material. A pressure bandage is applied to the lip or cheek for 2-3 hours to prevent hematoma. Sutures are removed on the 5-6th day after surgery.
If the operation is performed correctly, the cyst cavity is filled with a blood clot, which undergoes the process of organization, and after 3-5 months. complete regeneration of bone tissue occurs.
Rice. 5. Schematic representation of some stages of cystotomy: a - the mucoperiosteal flap is detached and raised, the bone wall is removed; b— the root apex is resected, the mucoperiosteal flap is screwed into the cyst cavity, the cyst cavity is plugged; 1 — mucoperiosteal flap, 2 — root apex, 3 — sealed tooth cavity, 4 — tampon in the cyst cavity.
Cystotomy
The course of surgery until the cyst shell is exposed is the same as with cystectomy. If root resection is expected, the mucoperiosteal flap is cut out with its base towards the edge of the alveolar process. After trepanation, the bone wall and contents of the cyst are removed and the anterior part of its shell is excised. Then the apexes of the roots of the teeth protruding into the cyst cavity are resected, and the resulting bone cavity is packed with iodoform gauze (Fig. 5). After 5-7 days the tampon is changed; in the future, only the entrance to the cavity should be tamponed. Tamponing of the cavity is stopped after 3-4 weeks, then the patient himself daily washes the postoperative cavity with a weak solution of potassium permanganate or hydrogen peroxide, using a rubber balloon with a soft tip. The depth of the cavity gradually decreases; after 6-8 months. in most patients, in its place only a slight bone depression is found, covered with normal mucous membrane.
If the dental cyst significantly pushes back the maxillary sinus, but does not perforate it, it is more advisable to perform a cystotomy. This is especially indicated in young people, because after 6-12 months. a small bone depression remains at the site of the cyst, and the maxillary sinus returns to its normal size. In elderly people, due to a decrease in recovery processes, it is more advisable to connect the 3rd joint with the maxillary sinus to form an anastomosis in the lower nasal passage, as during surgery for sinusitis (see Sinusitis); the wound on the side of the oral cavity is sutured tightly. The combined cavity subsequently exists as the maxillary sinus.
Forecast
with proper treatment, favorable.
Prevention
comes down to timely treatment of permanent and baby teeth affected by caries.
Bibliography:
Vernadsky Yu. I. Fundamentals of surgical dentistry, p. 311 and others, Kyiv, 1970; Evdokimov A.I. and Vasiliev G.A. Surgical dentistry, p. 244, M., 1964; Zedgenidze G. A. and Shilova-Mechanik R. S. X-ray diagnosis of diseases of the teeth and jaws, p. 183, M., 1962, bibliogr.; Rabukhina N. A. X-ray diagnosis of some diseases of the dentofacial system, M., 1974; Guide to surgical dentistry, ed. A. I. Evdokimova, p. 359, M., 1972.
P. V. Naumov; G. A. Zedgenidze (rent.).
Complications and prevention
Complications after surgery are possible if you do not follow the doctor’s special recommendations. A frequent cause of complications is the lack of self-discipline in the patient. The main complications include:
tissue infection during surgery; generalized sepsis; abscess syndrome around the affected tooth.
Rarely, the cause of postoperative complications is considered to be a lack of professionalism on the part of the dentist. Before treatment, it is important to inquire about the quality of services provided and the rating of the dental clinic. Complications include damage to molars in the maxillary sinuses and sepsis. If not the entire volume of purulent exudate is removed from the cyst, then the emergence of a secondary source of infection occurs almost immediately. Pus quickly spreads throughout the body and leads to dysfunction of many organs and systems. With the high-tech development of dentistry today, cases of complications as a result of cyst treatment are isolated episodes.
Preventive actions
When carrying out high-quality prevention, the patient must follow simple rules:
Carrying out regular hygienic teeth cleaning; sanitation of the oral cavity once a year; dental examination - 2 times a year; timely response to unpleasant symptoms in the oral cavity.
Treatment of cysts today is carried out successfully in a number of cases, so before visiting the dentist it is important to collect as much information as possible about the clinic and the professionalism of the specialist. You should not delay treatment, since in advanced cases, surgery is often the only possible way to eliminate the pathology.
For quick post-operative recovery, it is important for the patient to observe a hygienic regime, carry out preventive rinses of the mouth with herbal decoctions (chamomile, celandine, string, propolis) and medications (Miramistin, Iodinol). The patient’s discipline and attention to their own health are the key to oral health and the ability to treat any problems in the early stages using the most gentle methods.
Treatment of follicular dental cyst at Aristocrat-Dent dentistry
During the operation, the formation is carefully opened, cleaned, and subsequently does not prevent the tooth from cutting through the gum and taking its place. Advantages of treatment in our clinic in Moscow:
- qualified doctors with extensive experience;
- diagnosis and treatment of follicular dental cysts are carried out in the most careful and careful manner;
- X-ray examinations are carried out using a modern device with a minimum dose of radiation;
- all manipulations are absolutely painless and comfortable for both adults and children;
- affordable cost of services.
We strive to ensure that patients endure the removal of a follicular dental cyst and all the inconveniences associated with this process as easily as possible.
To make an appointment, contact the manager by phone 8 (495) 638-05-05. If you have a toothache or other discomfort, do not delay making an appointment. At your appointment, you will receive maximum information about modern methods of treating follicular dental cysts, the price of the service and other possibilities of modern dentistry.