Content:
- Features of the disease
- Causes of yeast glossitis
- How it manifests itself 3.1. Other symptoms of candidiasis on the tongue
- Treatment of tongue candidiasis 4.1. Medicines used for candidiasis 4.2. Traditional methods of combating oral candidiasis
- How to eat during treatment
- How to avoid getting sick
For the full functioning of all parts of the gastrointestinal tract, various fungi and bacteria must be present in the body.
They are called opportunistic pathogens. If their quantity corresponds to the norm, the person feels well and does not experience unpleasant symptoms of the disease. But under the influence of negative external or internal factors, bacteria and fungi can begin to actively multiply. Then their activity becomes abnormal - a disease of the oral cavity or stomach or intestines is diagnosed. It is in this scenario that candidiasis develops on the tongue, throat and cheeks. Let's look at how to treat it and what measures to take to avoid relapse after recovery.
Possible complications
This disease has a detrimental effect on the body’s defenses, so a sharp decrease in immunity, especially against the background of its chronic manifestation, makes the sick person even more vulnerable to serious consequences. Flu, viral infections, throat and respiratory tract diseases occur much more often and are more severe.
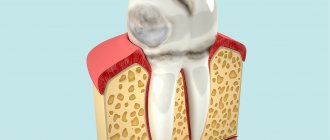
An equally important complication that can provoke a diagnosis is dental diseases that destroy the integrity of the hard tissue of the tooth and ultimately lead to its loss.
Stomach problems, the development of peptic ulcers and gastritis are the most common complication against the background of candidal stomatitis due to the patient’s refusal to eat due to pain.
Features of the disease
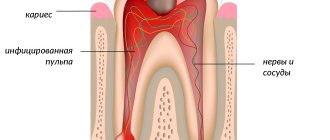
With candidiasis, there is an active spread of fungi of the genus Candida. Most often it is Candida albicans. To identify the pathogen, doctors carry out laboratory diagnostics - microscopic and bacteriological examination of the mucous membranes of the mouth, scraping plaque from the tongue.
Oral candidiasis is usually classified into two types:
- Yeast stomatitis. Affects the cheeks, gums, and palate. The tissues become covered with a characteristic white coating that cannot be easily removed.
- Yeast glossitis. The source of infection is the tongue. His back is affected. Small deep grooves are formed on its surface, in which whitish masses are deposited.
Tongue thrush always has clear clinical symptoms. It leads to swelling and inflammation of the tissues, causing severe pain. It gets to the point that the patient cannot chew food or even drink normally. The situation is aggravated by bad breath, which cannot be masked in any way.
Stages of disease development
Therapy for the disease is largely determined by the intensity of its development and the severity of symptoms at each stage of its course.
- First stage. It is characterized by the formation of single ulcers on the mucous surface of the cheeks, lips, and less often on the tonsils and the middle part of the tongue.
The disease hardly bothers the patient, is not always diagnosed on time and can last quite a long time. The absence of unpleasant sensations does not prompt the patient to go to the clinic - the person hopes that the problem will be solved spontaneously. - Stage two. The ulcers increase in number, and now in the place of their localization you can see white cheesy formations, which are easily removed.
However, after scraping them off, the affected area begins to hurt, and the first redness appears. The patient's temperature may increase, usually very slightly, due to which many do not find a connection between this phenomenon and the developing pathology. - Third stage. The plaque sticks quite firmly to the surface and is difficult to remove. The scraping process is accompanied by severe pain, and the wounds are open to the penetration of bacteria that cause microbial stomatitis - the treatment of which is a costly and lengthy procedure, with more complex symptoms and high fever.
- Fourth stage .
The most severe form, which requires urgent medical intervention. Damage to the upper respiratory organs begins, which is especially dangerous in infancy. Treatment should only be carried out by a specialized specialist. It is at this stage that the likelihood of infecting other people with the disease is highest.
Do you know how to treat canker sores at home? In the next article we will tell you more about this. And in the following review you can find out why a white coating may appear on the tongue.
Causes of yeast glossitis
In most cases, the disease is a consequence of a weakened immune system. Therefore, more often than others, people who have suffered some kind of serious illness encounter it. Pathology also develops due to dysbiosis resulting from long-term antibiotic therapy, taking hormones or immunosuppressants.
Other reasons include:
- ulcerative glossitis/stomatitis not treated in a timely manner;
- frequent mechanical damage to the mucous membrane covering the tongue;
- deficiency of vitamins and minerals;
- liver dysfunction;
- disruption of the normal quantitative relationship between different fractions of blood proteins;
- thyroid diseases;
- oncology;
- frequent consumption of alcoholic beverages, smoking;
- deficiency of potassium in blood plasma;
- pregnancy, breastfeeding.
Tongue candidiasis also occurs as a result of direct contact with a carrier of the infection. This refers to the transmission of the disease during kissing, when using shared utensils. In newborn children, the cause of pathology is the passage of a sick mother through the birth canal.
Diagnostics
Diagnostic measures involve a medical examination by a specialist, a laboratory study of the clinical picture, as well as a serological analysis of the patient’s blood serum.
Based on the examination results, the patient is either treated in a hospital setting or remotely at home.
To monitor the dynamics of treatment, microscopic examination of ulcer fragments for their contents is periodically prescribed. This is how the titres of the fungal infection are determined and it is checked whether the therapy regimen has been chosen correctly.
How it manifests itself
The disease is easily diagnosed, since its symptoms are clear and speak for themselves. Symptoms are the same in adults and children. The pathology develops according to the principle of dermatitis. The skin becomes inflamed, red, and mucous membranes swell. As the number of fungi increases, sores form. They are painful, covered with a white or yellowish coating. When trying to remove the latter, blood begins to flow.
Subjectively, the patient complains of:
- itching/burning on the affected areas of the tongue;
- pain when eating solid foods;
- bad breath;
- discomfort during a conversation.
Plaque found on mucous membranes consists of dead epithelial cells, fibrin, bacteria, and food microparticles. It can be located in small isolated areas or merge into volumetric circles. If measures are not taken in time to eliminate this symptom, the infection will spread to the throat and then to the internal organs.
The danger lies in the fact that candida multiplies very actively. They are able to penetrate into the deep layers of the mucous membranes of the mouth. Then the disease is difficult to treat, and the likelihood of relapse remains high.
As for the painful sensations that appear while eating, they are associated with severe tissue inflammation. The latter turn red and bleed. Any mechanical impact aggravates the situation.
If pain occurs when swallowing, it means that candidiasis has spread to the pharynx. A feeling of a lump in the throat indicates the appearance of voluminous film growths. This should not be allowed. The sooner treatment is started, the lower the risk of unwanted complications.
Other symptoms of candidiasis on the tongue
Other signs indicating the disease include:
- weakness, lethargy;
- increased body temperature;
- proliferation and enlargement of the papillae on the surface of the tongue;
- deterioration of taste or loss of the ability to recognize tastes;
- tissue swelling;
- decreased tongue mobility.
If these symptoms appear, you must make an appointment at a dental clinic.
Herpetic stomatitis
The reason is the herpes virus, which is in the body. It is believed that most of the population is a carrier of the herpes virus, which does not manifest itself in any way. But when immunity decreases, it becomes more active. Most often the disease goes away within 2 weeks. In adults, general manifestations such as fever and weakness usually do not occur. Possible enlarged lymph nodes.
Herpetic stomatitis photo:
First, small bubbles with liquid form, which then burst. Forming small ulcers located in groups. On the inner surfaces of the lips and cheeks, tongue and palate. They often merge with each other, forming irregular shapes. Covered with a white-gray coating.
Priority for treatment in antiviral agents.
Treatment of tongue candidiasis
The treatment regimen is selected taking into account the factor that provoked the development of the disease. The main goal of therapy is not just to destroy pathogenic flora, but also to strengthen the immune system and improve the functioning of the stomach and intestines. If this is not done, the likelihood of relapse will remain high.
If the disease is caused by long-term antibiotic therapy, taking hormones or steroids, as is most often the case, you need to reduce the dosage of drugs from these groups and at the same time start using antifungal tablets. B vitamins and immunomodulators have an excellent effect on the body during the treatment of tongue candidiasis.
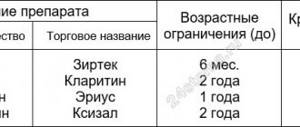
Medicines used for candidiasis
It is impossible to get rid of fungi of the genus Candida that have multiplied on the mucous membranes of the tongue without medications. Medicines should:
- relieve inflammation;
- activate regeneration processes;
- reduce pain;
- destroy fungi;
- heal ulcers;
- reduce swelling.
For this purpose, dentists prescribe the following pharmacological groups:
- Antifungal. They act by destroying the cell membranes of the pathogen. They are manufactured in the form of tablets and capsules for oral administration.
- Antiseptics for mouth rinsing. They destroy viruses, fungi, bacteria, and create conditions for the restoration of healthy microflora.
- Gels and ointments with antifungal activity. Used strictly locally. They treat the surface of the entire tongue. They help remove swelling, minimize itching and burning. Excellent healing of existing wounds.
- Antiseptics in the form of aerosols. Very convenient to use. Suitable for use in public places. Characterized by a wide spectrum of action.
When treating candidiasis in the tongue, it is important to use exactly the drugs prescribed by the doctor. There is no need to exceed their dosage, as this may cause the opposite effect.
Traditional methods of combating oral candidiasis
If you really want to supplement drug therapy with herbal remedies, it is permissible to use:
- decoctions of anti-inflammatory herbs;
- alcohol tincture of propolis;
- soda solution.
These products should be used while rinsing the mouth.
How to eat during treatment
Candida fungi multiply very quickly if a person eats a lot of sweets. Therefore, until complete recovery you need to stop eating:
- sweets;
- ice cream;
- baking.
Any alcoholic drinks are also prohibited.
Meat lovers should give preference to turkey and chicken. Buckwheat porridge is very useful - it contains many B vitamins. In order not to further irritate or injure the mucous membrane of the tongue, you should eat warm and well-chopped food.
Reviews
It is important to remember that candidal stomatitis is easily spread by airborne droplets. Therefore, not only a healthy person should be attentive to his body.
A patient infected with fungal bacteria must understand how dangerous it is for others and take measures to avoid becoming a source of infection for other people.
If you are interested in the problem discussed in this article, you can leave your feedback below – in the “comments” section.
If you find an error, please select a piece of text and press Ctrl+Enter.
How to avoid getting sick
Preventive measures include following simple rules:
- balanced diet;
- elimination of traumatic effects on the tissues of the tongue;
- taking an antifungal drug during a course of antibiotics and hormones;
- course use of immunomodulators;
- maintaining oral hygiene;
- timely treatment of emerging dental diseases.
People who take care of their dental health and visit the dentist twice a year are much less likely to experience tongue candidiasis. This is a proven fact. Therefore, do not ignore your doctor’s requests to come for preventive examinations.
Aphthous stomatitis
It can be acute (from a virus) or chronic. Acute differs from chronic in general manifestations: fever and general weakness.
Aphthous stomatitis photo:
Chronic is often accompanied by the appearance of aphthae in the anterior region of the oral cavity on the inner surface of the lip and tongue.
Ulcers can be single or multiple, up to five pieces. Sizes from 3 to 7mm. It practically does not cause any general ailments. The causes of chronic stomatitis are often gastrointestinal diseases, allergic reactions and a general decrease in immunity. Relapses are possible.