Treatment of dental diseases caused by HIV
The presence of the immunodeficiency virus requires complex treatment that can maintain the necessary vital functions of the body.
It is based on taking various antiretroviral medications. Dental ailments caused by HIV must be treated promptly and thoroughly. Suppressed immunity and internal microflora cannot resist pathogens, so illnesses progress quickly. Therapy includes treatment in the dentist's office and medication (broad-spectrum antibiotics, antiviral, antifungal medications, corticosteroids, etc.).
Dental diseases
Dental clinics provide safe and high-quality treatment. In this case, disposable instruments are used, and reusable ones are carefully sterilized (in the environment the virus dies at temperatures above 60 degrees). Dentists carry out all the necessary manipulations - treat caries, fill teeth, perform prosthetics
However, they approach the issue of surgical intervention very carefully
Doctors often encounter HIV periodontitis. It has all the signs of ordinary periodontitis (inflammation of periodontal tissues), but is characterized by rapid progression. This means that the patient can very quickly lose teeth. The therapy represents classical measures to combat periodontitis, taking into account the patient’s main course of medication.
Gingivitis
Gingivitis in the mouth is an inflammatory process in the gums. Depending on the form and degree of development, the patient develops various signs, including swelling, redness, itching or burning, bleeding, atrophy or enlargement of the gingival papillae, and the formation of necrotic ulcers.
Gingivitis is treated comprehensively:
- sanitation of the oral cavity and professional cleaning (we recommend reading: how is sanitation of the oral cavity carried out?);
- thorough treatment with antiseptic drugs;
- taking antibiotics or antiviral medications;
- taking antihistamines;
- use of healing gels and ointments.
Candidal stomatitis
Candidiasis (thrush) is observed in more than 90% of infected people. Stomatitis in this case can be atrophic, hypertrophic or pseudomembranous. The latter type of candidal stomatitis occurs most often.
READ ALSO: methods of treating candidal stomatitis in adults
Thrush is characterized by classic symptoms:
- dense, curdled coating of white or gray color;
- redness and swelling of the mucous membrane;
- the formation of ulcers or painful erosions that grow together with soft tissues.
READ ALSO: gray coating on a child’s tongue: causes and treatment
For candidiasis, it is recommended to take antifungal drugs that inhibit the Candida fungus, antimycotics, the use of pharmaceutical antiseptics, careful oral hygiene, and diet. For extensive candidiasis lesions, healing agents are used.
READ ALSO: how and how to effectively treat fungus on the tongue?
Other diseases
Almost all HIV patients experience hairy leukoplakia (Epstein-Barr virus). It appears as a permanent white or gray coating on the tongue. The mucous membrane becomes covered with folds and rough plaques. The occurrence of pathology is provoked by malfunctions of the immune system.
READ ALSO: What can cause your tongue to hurt and how to relieve the pain?
That is why the treatment has an immunomodulatory focus:
- antiretroviral therapy;
- immunotherapeutic treatment;
- antiviral medications;
- antimycotics;
- medicines based on retinoic acid;
- in advanced cases, the affected areas are excised surgically or using a laser.
Viral infections
In HIV-infected people, the most common manifestations of stomatitis are caused by the herpes simplex virus. Primary infection with the herpes virus occurs in children, adolescents, and, less commonly, young adults. Since the infection is latent, there is a tendency to recur, and manifestations can be both general (fever, pain when swallowing, swollen lymph nodes) and local. Acute herpetic rashes can be localized in any part of the maxillofacial area. Favorite places are lips, gums, hard palate. The initially small bubbles that form then merge into larger ones. After the destruction of the tire, the underlying tissues tend to ulcerate. In the oral cavity, the bubbles burst very quickly, and usually erosion is immediately detected. On the red border of the lips, the vesicles of the blisters shrink, forming dry or weeping crusts.
The herpes virus can cause generalized lesions up to and including herpes encephalitis.
Recurrent herpetic stomatitis is most often localized on the red border of the lips with the involvement of surrounding areas of the skin. The blisters quickly enlarge, merge, and a secondary infection develops. The contents of the blisters suppurate, resulting in the formation of crusts of a dirty yellow color; after their separation, an eroded or ulcerated surface is exposed (Fig. 5).
Rice. 5. Viral wart.
The lesions on the hard palate and gums are represented by small bubbles that quickly burst, leading to ulcerative lesions of the mucous membrane. Clinical manifestations can be triggered by a cold, stress, or respiratory infection (Fig. 6).
Rice. 6. Hairy leukoplakia on the lateral surface of the tongue.
Shingles (herpes zoster) in the oral cavity and on the face is characterized by asymmetry of the lesion according to the area of innervation of one of the branches of the trigeminal nerve. It is also possible that two or three branches of trigeminus are involved, when elements appear on the mucous membrane in the form of small blisters and then an ulcerated surface. The rash is preceded by burning pain, simulating pulpitis of intact teeth, radiating along the maxillary or mandibular branch of the fifth pair of nerves. These pains may persist even after involution of the lesions (up to 1–2 months).
Viral growths come in the form of warts, papilloma, genital warts and frontal epithelial hyperplasia (papules or nodular lesions with filamentous growths).
Warty formations are localized in the corners of the mouth. They may have the appearance of a papilloma, ridge, or protrusions (Fig. 7).
Rice. 7. Hairy leukoplakia of the ventral and dorsal surface of the tongue.
Genital warts. Depending on the location, the lesion elements can have different appearances: multiple pointed protrusions or rounded, slightly raised areas with a flat surface. When localized on the gum or hard palate, the lesions appear as multiple pointed projections. When located on the cheeks and lips, the elements have a picture similar to focal epithelial hyperplasia: rounded, slightly raised areas with a diameter of about 5 mm with a flattened surface.
Hairy leukoplakia. The lesion is localized, as a rule, on the tongue, having different sizes and appearance. It is found in limited areas of the lateral, dorsal, ventral surface or covers the entire tongue. The mucous membrane takes on a whitish appearance, but hyperkeratosis does not develop. On palpation, the seals are not detected, which served as the basis for designating this form of lesion: soft leukoplakia (Fig. 8).
Rice. 8. Kaposi's sarcoma on the skin of the face.
On the lateral surface of the tongue, elements can be located bilaterally or unilaterally (Fig. 9). The mucous membrane, over a limited or widespread area, becomes irregular and rises in the form of folds (“corrugated”) or projections above the surrounding surface, which may resemble hair in appearance. Hence the name - hairy leukoplakia.
Rice. 9. Kaposi's sarcoma on the palate.
On the lower surface of the tongue, the focus of epithelial opacification may be smooth or slightly folded. Much less commonly, soft leukoplakia occurs on the cheeks, floor of the mouth, and palate.
There are no subjective sensations other than discomfort.
Hairy leukoplakia can be combined with candidal glossitis, confirmed by laboratory methods. However, treatment of candidiasis does not affect the appearance of the lesion.
Histological, virological, including serological, studies give reason to believe that the cause of soft hairy leukoplakia is the Epstein-Barr virus.
Soft leukoplakia must be differentiated from leukoplakia, lichen planus, chemical or electrical burn, and chronic hyperplastic candidiasis.
Complex clinical picture
The presence of an infection in the mouth of any location (stomatitis, cheilitis, glossitis, gingivitis), which is difficult to treat, is an alarming sign and may be a manifestation of HIV. This is a signal that the immune system cannot cope with the infection and the person may be a carrier of immunodeficiency viruses.
You should suspect something is wrong if the listed diseases are protracted and cannot be treated with antibacterial and antifungal medications.
General view of the oral cavity
HIV and AIDS are characterized by various inflammatory reactions in the oral cavity - erosions, ulcers, blisters, which often occur in the mouth and are poorly treated with standard medications. There is often severe odor from the mouth due to the addition of a secondary bacterial infection.
Appearance of the tongue in HIV
The tongue is covered with a white coating, densely populated by a colony of fungi of the genus Candida. It does not clean off on its own; after removal with instruments, a reddened and bleeding mucous membrane is revealed underneath.
The lateral surfaces are affected by leukoplakia. It forms growths of the epithelial layer that look like whitish or light yellow thin villi.
In the photo, the main symptoms on the tongue for HIV are candidiasis, leukoplakia:
Throat view
The mucous membrane of the throat with HIV is hyperemic, covered with erosions and white ulcers, 3-5 mm in diameter. Sometimes abscesses appear on it, which look like yellow blisters with thick contents.
Cheek view
On the mucous membrane of the cheeks in the area where the teeth meet, areas of compaction of the epithelial layer form in the form of a white film. Hemorrhages are observed in the submucosal tissues - multiple red dots with a diameter of 1-2 mm.
Type of gums
Gingival papillae are deformed due to ulcerative necrotizing gingivitis. The mucous membrane is covered with a dense white coating that emits an unpleasant odor.
However, the immunodeficiency virus affects the entire body, not local organs
Therefore, in order to suspect a diagnosis of HIV, it is necessary to pay attention to the following accompanying symptoms:
- sudden unexplained weight loss;
- fever lasting longer than 1-1.5 months, for no apparent reason;
- simultaneous enlargement of lymph nodes in different parts of the body (cervical, axillary, inguinal).
Therefore, all manifestations of HIV in the oral cavity are accompanied by symptoms of general damage to the body.
Classification of common lesions
All diseases that occur in the oral cavity due to HIV can be divided into 2 large groups.
Lesions that almost always occur during the development of infection:
- Kaposi's sarcoma is a malignant tumor that looks like purple or dark blue protruding spots on the mucous membrane, with a diameter of 1 to 4 cm, the surface is uneven, lumpy;
- Non-Hodgkin's lymphoma is a malignant tumor of the dentofacial area, accompanied by enlarged lymph nodes, destruction of bone tissue around the teeth, bulging and redness of the mucous membrane in the affected area;
- hairy leukoplakia – forms on the tongue (on the lateral surface), has the appearance of white villi;
- candidiasis is a fungal infection, manifested by hyperemia of the mucous membrane and abundant white or yellow plaque that does not come off on its own;
- ulcerative-necrotizing gingivitis associated with HIV is of a bacterial nature, occurs suddenly, with acute manifestations, after some time the gum tissue dies, forming a defect, and relapses often occur.
In the photo, Kaposi's sarcoma is a common manifestation of AIDS in the oral cavity. More rare manifestations:
- thrombocytopenic purpura is a disease of the hematopoietic system, manifested by hemorrhages in the mouth, looking like a pinpoint red rash;
- bacterial and viral infections - affect the gums, periodontium, lips, tongue, are resistant to antibiotics and antiviral drugs, and have frequent relapses;
- diseases of the salivary glands.
In the photo, cheilitis is a common lesion of the lips during the development of HIV infection
Symptoms of HIV in the mouth with photos
There is a conditional gradation of HIV symptoms in the oral cavity, depending on the degree of their relationship:
- diseases that primarily indicate an immunodeficiency virus (candidal stomatitis (thrush) in various manifestations, gingivitis, herpetic gingivostomatitis, periodontitis, Kaposi's sarcoma);
- signs that are less associated with the virus (infectious lesions of a bacterial nature; diseases of the mucous membrane or hard tissues caused by viral infections; pathologies of the salivary glands);
- symptoms that do not directly indicate infection, but can be triggered by the virus.
In HIV patients, the painful condition of the oral cavity is chronic with periodic exacerbations, relapses and remissions. Gradually, the situation worsens, clinical symptoms intensify, and periods of rest are practically absent. The mucous membrane suffers even from minor pathogens, which the immune system of healthy people immediately rejects.
In medical photographs, characteristic symptoms can be seen very clearly:
- a dense coating on the tongue, palate, cheeks of a grayish-white or yellow color (we recommend reading: what is it if a yellow coating appears on the tongue?);
- bad breath that does not go away after brushing your teeth;
- the presence on the mucous membrane of ulcers, blisters, seals, adhesions, aphthae or erosions that are of an incomprehensible nature, but cause pain and discomfort;
- bleeding gums;
- unsatisfactory condition of the teeth (they are susceptible to the development of caries, since the body does not recognize pathogenic bacteria).
Tongue with HIV infection photo
The immunodeficiency virus destroys the protective barrier of the human body, making it vulnerable to any infections.
The first to be affected are usually the mucous membrane of the oral cavity and the tongue with HIV - they are affected by chronic diseases with frequent exacerbations and short-term remissions.
These can be either numerous ulcers that heal on their own, or more serious problems that require the help of specialists. Let's try to figure out exactly how HIV manifests itself in the mouth, and what medicine offers to alleviate the patient's condition.
Causes
After infection with HIV, the body remains defenseless against pathogenic bacteria and microbes. The immunodeficiency virus, including the one that causes various pathologies of the oral cavity, is transmitted through sexual, parenteral and perinatal routes.
The exchange of fluids during sexual intercourse is the most common way of contracting HIV, but it is also possible to become infected through a blood transfusion or at the dentist's office.
A baby can get the immunodeficiency virus in the womb of an infected mother or during breastfeeding.
Timely prevention of HIV infection in the oral cavity makes it possible to recognize the symptoms of infection in time and avoid exacerbation of diseases affecting the mucous membranes and tongue. Of particular importance in this regard is the determination of viral load indicators for HIV, which make it possible to estimate the number of virus particles in the patient’s blood.
Symptoms of HIV infection in the oral cavity
The first symptoms of HIV in men and women, as a rule, affect the oral mucosa and tongue. Typical manifestations of HIV infection in the oral cavity are:
- a dense gray-white or yellow coating on the tongue, palate and inner surface of the cheeks;
- ulcers, blisters and erosions on the mucous membrane;
- burning and pain when touched;
- bleeding from the gums;
- poor dental condition.
As the infection progresses, the picture of clinical symptoms worsens - periods of remission become shorter and shorter, and the symptoms of the immunodeficiency virus become chronic.
Stages of HIV infection in the oral cavity
The period from 7-10 days to 2-3 months from the moment of infection is called the incubation stage.
Immediately after infection, there are no manifestations of HIV, so damage to the oral mucosa is typical for a later period of development of the disease.
Further development of infection in the body leads to a transition to the stage of secondary diseases. As the immune system is destroyed, changes in the oral mucosa become typical for HIV - patients suffer from chronic candidiasis, herpes, gingivitis, etc.
Diagnostics
Timely medical examination allows early recognition of signs of AIDS and HIV on the tongue and oral mucosa - diagnosis, prevention and properly selected treatment make it possible to improve the patient’s condition and protect his environment. For this purpose, the following is carried out:
- PCR reaction to immunodeficiency virus RNA;
- immunoblotting for antibodies to certain types of antigens;
- enzyme immunoassay for antibodies to HIV;
- study of immune status.
Differential diagnosis is also carried out with hyperplastic candidiasis, allergic reactions, smoker’s leukoplakia, etc.
Anomalies
Oral diseases associated with HIV are usually divided into several groups:
- Fungal infections, such as candidiasis and histoplasmosis, causing the appearance of plaques on the mucous membrane and plaque on the tongue.
- Viruses, primarily hairy leukoplakia and herpetic stomatitis, a disease with painful sores on the lips and palate.
- Neoplasms, mainly Kaposi's sarcoma and non-Hodgkin's lymphoma.
- Bacterial infections, most often in the form of chronic periodontitis.
Necrotizing ulcerative gingivitis, which causes inflammation and bleeding of the gums, also belongs to this group. Damage to tissue and bone structures in this disease most often ends in patients with rapid loss of teeth.
Important! In the case of HIV-infected patients, compliance with the rules of hygiene and a healthy diet is not enough to maintain an oral cavity in order - they need regular consultations with a dentist and timely treatment of ailments associated with their diagnosis
Diagnostics
Diagnosis of HIV infection should be carried out not clinically, but in a laboratory setting.
The presence of secondary or concomitant diseases allows us to realistically assess the severity of the patient’s condition and the need for hospitalization. In order to confirm the diagnosis of HIV infection, various methods are used: virological, molecular genetic, serological and many others. Antibodies in HIV usually appear within 2 weeks to 3 months from the moment of infection, but in some cases this period can reach 6 months. A careful examination of the medical history in most cases allows us to identify the causes of immunodeficiency. If the patient is diagnosed with immunodeficiency, it is necessary to conduct an HIV carrier test.
What you need to know about the manifestation of HIV in the oral cavity?
HIV is not as rare a disease as it might seem. And it can affect any family, even those leading an active lifestyle and closely monitoring their health. In Russia, the virus causes approximately 80 deaths every day. Finding an effective drug is the task of scientists and pharmacological laboratories around the world. In 2021, a vaccine appeared, the task of which is to “train” the immune system to destroy the cell membrane of the virus. But its testing has just begun.
There are several main routes of HIV transmission: through blood, sexual intercourse and breast milk. Previously, there was another common method of infection - from mother to child. But at this stage of medical development, it is practically excluded. It is almost impossible to become infected through blood from person to person during everyday contact - a number of factors must coincide. But the transmission of the virus through unsterile medical and cosmetic instruments has a basis - such facts are known. At the same time, with blood transfusions, after 1994, the risks of infection have been reduced to zero.
By receiving adequate antiretroviral therapy with high-quality drugs, people with HIV have a chance to live a full and happy life until old age. It is necessary to take into account that the drugs will have to be taken every day at the same time and so throughout life. The earlier the disease is identified and treatment is started, the less harm the virus could cause to the body and the therapy itself will be easier.
Manifestations of HIV in the oral cavity are quite easy to notice. Unlike other organs and systems of the body, it is clearly visible and you can examine it yourself in the mirror. The discomfort that appears over a long period of time should alert any person who monitors their health. Even if there have been no recent potential risk situations.
Everyone should know the nature of the manifestation of HIV infection in the oral cavity. An insidious virus may not reveal itself in any way for several years and become active at one moment. Therefore, at the slightest suspicion, conduct a self-examination and go to the doctor. Be extra vigilant and take a test that will give a negative result - save your nerves and health.
Why does infection occur?
The most common way of transmitting HIV from person to person is through unprotected sex. When the virus penetrates through microtraumas in the mucosa. The second way is through the blood. It is common when using non-sterile syringes. The virus must not only enter the body, but also encounter CD4+ cells there. Both the first and second methods contribute to this possibility, since the contaminated material penetrates quite deeply.
After entering the body, along with the bloodstream, the virus enters leukocytes, embedding its information into their DNA. From this moment its harmful influence begins. It blocks the ability of immune system cells to recognize foreign agents and the person begins to get sick.
Manifestations of HIV infection in the oral cavity are one of the first signs of the disease. Various symptoms appear due to the fact that the immune system cannot cope with bacteria that are constantly on the tongue and teeth. Moreover, the function of leukocytes that is responsible for their destruction is blocked. All this indicates a general malfunction of the immune system.
Causes and course of the disease
Acquired immune deficiency syndrome (AIDS) is caused by a retrovirus called human immunodeficiency virus (HIV).
The following routes of transmission of HIV infection are known: through blood, including through injections, through the mucous membrane during sexual contact, and also from mother to child through the placenta. Clinical manifestations of AIDS infection can take a period of 7 to 11 years, but in some cases the disease develops after 3 years. The cause of the development of the disease is violations of humoral and cellular immunity. During HIV infection, a subpopulation of T-helper cells is affected, and other lymphoid cells and cells of the nervous system are also affected.
When a retrovirus enters the body, it infects cells, and they lose the ability to control fungal, viral, bacterial and other types of secondary infections that enter the body, as well as malignant (malignant) cells. The function of B lymphocytes is impaired, which reduces the ability to reproduce virus-neutralizing antibodies. Due to the fact that too many immune complexes circulate in the body, pathological autoimmune processes develop.
At the initial stage of the disease, the body is still able to produce virus-neutralizing antibodies, which can suppress freely circulating viruses, but they cannot affect proviruses (viruses found in cells). After about 5-7 years, the protective capabilities of the immune system are depleted, and free viruses and secondary infections that have an endogenous (internal) source accumulate in the blood. All this leads to the activation of one’s own microflora: mycobacterium tuberculosis from Ghosn’s lesions, the occurrence of Kaposi’s sarcoma. As a result of the activation of herpes viruses of various types, invasive (penetrating into the tissues) cervical cancer develops, and manifest (obvious) forms of fungal and cytomegalovirus infections develop.
The cytopathic (destructive) effect of HIV affects the cells of the blood, nervous, musculoskeletal, cardiovascular, endocrine and other body systems. This leads to multiple organ failure, which is characterized by a variety of clinical manifestations and constant progression of HIV disease.
At all stages of the development of HIV infection, open manifestations of various AIDS-indicative diseases of the ENT organs are observed. The exception is the incubation period of the disease.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
Symptoms and manifestations
However, the course of the disease and symptoms are similar in HIV-infected and HIV-uninfected people (treatment is also largely similar).
Oropharynx
Symptoms of oropharyngeal lesions include localized burning pain, changes in taste, and difficulty swallowing liquids and solids. Many patients are asymptomatic. There are variants of the course: the most common pseudomembranous form (white plaques on the mucous membrane of the mouth, gums, or tongue) and the rarer atrophic form (hyperemic mucous membrane), chronic hyperplastic form (leukoplakia, but not to be confused with “hairy leukoplakia”) involving tongue, angular cheilitis (inflammation and formation of cracks in the corners of the mouth).
Esophagus
Esophageal localization of candidiasis infection is usually manifested by dysphagia (impaired swallowing) and iodynophagia (pain when making swallowing movements). But 40% of patients are asymptomatic. Occasionally, esophageal involvement may occur in the absence of clinically detectable oropharyngeal involvement.
Vulva and vagina
Vulvovaginal localization of infection, also known as thrush, is usually manifested by severe itching, redness of the skin around the vaginal opening, swelling of the skin around the vagina, swelling and redness of the labia, odorless white-gray vaginal discharge (a change in color or the appearance of an unpleasant odor will indicate addition of a bacterial infection). The cervix usually appears normal on examination. Symptoms usually worsen a week later, and an advanced form of thrush may occur. Previous menstruation brings some relief at the very beginning.
The advanced form of the disease in males is much less common. A common question that arises among men is: is it possible to get thrush from a sick woman? At present, the question remains open. Although it is worth noting that men may experience itching and burning during or after sexual intercourse, there are also cases when a combination of many factors can trigger the occurrence of candidal balanitis, that is, thrush in men.
Sources
- https://parazitsos.ru/kandidoz/kandidoz-pri-vich.html
- https://www.omolochnice.ru/zabolevaniya/kandidoz-pri-vich.html
- https://shabash-magov.ru/%D0%BC%D0%BE%D0%BB%D0%BE%D1%87%D0%BD%D0%B8%D1%86%D0%B0-%D1% 83-%D0%B2%D0%B8%D1%87-%D0%B8%D0%BD%D1%84%D0%B8%D1%86%D0%B8%D1%80%D0%BE%D0% B2%D0%B0%D0%BD%D0%BD%D1%8B%D1%85/
- https://lechenie-molochnica.ru/lechenie/lechenie-kandidoza-pri-vich-infektsii/
- https://EtoGribok.ru/molochnica/vidy/kandidoz-pri-vich.html
- https://VeneroMed.ru/molochnitsa/kandidoz-pri-vich
- https://venerologia03.ru/molochnitsa/u-vich-infitsirovannyh.html
- https://okandide.ru/indicium/kandidoz-pri-vich
Symptoms of thrush
Almost every woman has experienced thrush at least once in her life, so its symptoms are well known and easily distinguished from any others. This is largely due to the structural features of the skin and mucous membranes and the peculiarity of the life cycle of the causative agent of the disease.
Depending on the location of the primary lesion in candidiasis, there are:
- Superficial forms - in which the primary foci of the disease occur on the mucous membranes (oral cavity, genital organs), skin, nails and nail folds;
- Visceral forms - with them there are not only primary foci, but also their spread throughout the body with damage to internal organs;
- Erased and atypical forms - in which the focus of thrush imitates some other disease, most often of an infectious nature;
- Chronic forms - in this case, it is not possible to completely eliminate the manifestations of the pathological process even with massive antifungal therapy.
Depending on the location of the main focus in the superficial form of the disease, the following can be diagnosed:
- Superficial skin candidiasis - in this case, the pathological process develops in those areas of the skin that are constantly exposed to high humidity and temperature. The most striking representative of the disease is diaper dermatitis, which occurs in children in the first two years of life and is manifested by severe itching and the characteristic appearance of the affected areas of the skin;
- Mucocutaneous candidiasis - in this case, the pathological process occurs only with deep suppression of the immune system. Characteristic manifestations of the disease include generalized damage to the skin and mucous membranes of the digestive tract with disruption of their function (malabsorption syndrome);
- Urogenital candidiasis - in this case, the pathological process remains localized on the skin and mucous membranes of the genital organs. The very first symptom of candidiasis is a sharp itching in the perineal area, which quickly increases and practically does not subside.
The severity of clinical symptoms of candidiasis - what does it depend on?
In the genital area, regardless of a person’s age, a huge number of nerve endings are concentrated, so irritation and itching are the most intolerable and problematic manifestations of thrush. Some time after their appearance, a white coating and a cheesy white-gray discharge appears on the mucous membrane of the vagina and genitals. However, not all patients notice this discharge, since itching provokes the need for more frequent and thorough personal hygiene sessions.
This is due to the fact that the body’s local immunity can restrain the penetration of the fungus into deep tissues, but cannot completely get rid of it. Sooner or later, this precarious balance will swing either towards recovery or towards further development of the disease.
Features of the clinical course of thrush in women and men
Some scientists have concluded that a third of patients get thrush through sexual contact, but studies show that only 10% of partners of women who have candidiasis are also infected with fungi. An indisputable fact is that women have thrush 10 times more often than men, while sexual life has a relative influence on the development of clinical symptoms (both young girls and adolescents who have not yet had sexual intercourse can suffer from this disease). contacts). If sexual contact has taken place, then there is a 40% chance that the man will also get genital candidiasis, and if a healthy woman had a relationship with an infected man, then her chance of getting sick is 80%.
There is a reasonable opinion that the degree of disruption of the normal microflora of the vagina is of primary importance in the clinical picture and course of candidiasis - very often the first symptoms of the disease occur while taking antibiotics.
According to some data, the use of antimicrobial therapy without preventing thrush leads to candidiasis in half of the patients.
Forms of urogenital candidiasis
Modern medicine distinguishes three main forms of candidiasis:
- Carriage of the fungus;
- Acute urogenital candidiasis;
- Chronic thrush.
If a person is just a carrier, then he does not and cannot have any complaints or symptoms, but when taking smears, it is quite possible to isolate the fungus. If a suitable environment is created for the active development of the fungus, the disease becomes acute. Even if a carrier woman does not have a pronounced clinical picture, she can transmit the causative agent of the disease to her child during childbirth.
Why does a rash appear with HIV?
The first signs of HIV disease are rashes on the surface of the skin and mucous membranes. As a result of the destruction of the immune system by HIV, the body becomes vulnerable to various infections that manifest themselves in the form of skin diseases. The condition of the skin acts as a kind of indicator, the condition of which indicates certain dysfunctions of organs and systems.
Skin diseases of various types occur with HIV. Their manifestations depend on the stage of the disease, the age of the patient, the pathogen: hemorrhagic vasculitis, Cosh's sarcoma, candidiasis, lichen, seborrheic dermatitis, molluscum contagiosum, warts.
8 days after infection, red spots may appear on the face, torso, genitals, and mucous membranes.
Skin diseases associated with HIV are accompanied by the development of specific symptoms:
- fever;
- weakness;
- diarrhea;
- body aches;
- pain in muscles, joints;
- high body temperature;
- increased sweating.
After infection, skin rashes are chronic. They are practically untreatable and can progress over several years. With further development of the disease, viral, microbial, fungal infections progress: herpes, lichen, stomatitis in adults and children, syphilitic, purulent rashes, mycotic lesions.
Group III: lesions that occur during HIV infection, but are not directly related to it
The category includes diseases such as ordinary periodontitis, gingivitis, fungal infections that are not caused by fungi of the genus Candida, osteomyelitis, sinusitis, inflammation of the submandibular fatty tissue, neurological disorders and many others.
Patients who have been diagnosed with one of the above lesions should be tested for HIV infection as soon as possible. This will make it possible to prescribe timely treatment, thanks to which you can stop the development of the disease and its transition to the AIDS stage.
Treatment of dental diseases caused by HIV
Diagnosed HIV infection in the oral mucosa requires long-term treatment to maintain optimal immune status. Treatment consists of taking a complex of medications: antiretroviral, antibacterial, antimycotic, hormonal.
Dental diseases
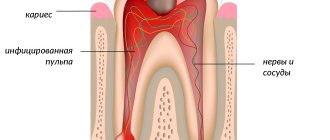
The most common infection of bacterial origin associated with HIV in the oral cavity is considered to be inflammation of the periodontium (periodontitis), a group of tooth-supporting structures (gums, ligamentous and bone structures).
The causes of the disease are:
- High concentration of pathogenic microorganisms resulting from immunodeficiency.
- Orthodontic causes: malocclusion with injury to surrounding structures, abnormal arrangement of teeth, frenulum.
- Tartar deposits are the result of: poor oral hygiene, smoking, and excess consumption of carbohydrate foods.
- Genetic predisposition.
- Diabetes.
- Vitamin deficiency (A, C).
- Hormonal imbalance.
A specific clinic is characterized by the destruction of dental cells and processes of the alveoli. There is pathological bleeding of the gums, exacerbation of their sensitivity, loosening of teeth and their loss, secretion of viscous saliva, and the formation of plaque on the teeth. In advanced cases, necrosis of the mucous membranes and softening of bone structures with the formation of free fragments cannot be excluded.
Further spread of inflammation can be eliminated by surgical removal of dead cells and sanitization of foci of infection with solutions of antiseptics and antibiotics.
Gingivitis
Gingivitis and the presence of HIV infection are closely related. The disease manifests itself in inflammation of the gums: pain, swelling, increased bleeding, thinning or thickening of the edges, and the appearance of areas of ulceration.
Treatment of this pathology is similar to periodontitis therapy.
Candidal stomatitis
AIDS patients suffer from candidal stomatitis in 90% of cases;
The use of agents that inhibit fungal micelles (antimycotics) and thorough sanitation of the oral cavity are indicated.
Other diseases
HIV infection in the oral mucosa can create favorable conditions for inflammation:
- jaw bones with subsequent softening;
- sinuses (sinusitis);
- subcutaneous fat (submandibular cellulite).
Conservative therapy includes taking medications that help maintain the immune system's defenses.
In severe cases, they resort to surgical treatment methods by laser or traditional excision of pathological foci.
HIV infection is a disease caused by the human immunodeficiency virus. Without specialized treatment, it goes into the terminal stage - AIDS (acquired immunodeficiency syndrome) and ends in death.
The virus infects the cells of the immune system, lymphocytes, and leaves the body vulnerable to various infections that are harmless to a healthy person.
Fighting candidiasis in HIV-infected people - where to start?
Candida fungi in HIV can cause the progression of a complex and dangerous disease. As is known, these opportunistic microorganisms are present in the normal healthy microflora of the human body in small quantities. They are localized in the intestines, mouth, vagina and skin. The immunodeficiency virus weakens the protective functions, which leads to the manifestation of the pathogenic characteristics of Candida fungi. Candiosis in HIV-infected people occurs very often (in 90% of patients), especially in the later stages of progression of the fatal pathology.
Candidiasis in HIV: features of the disease
In patients with immunodeficiency, this fungal disease has distinctive features, namely:
- Most often, the disease affects young male patients.
- The disease occurs in an acute phase and is difficult to treat.
- The lesions are localized in the genital area and in the mouth.
- Erosion spreads quickly, causing a lot of discomfort and unpleasant sensations.
Candiosis is the first sign of significant progression of immunodeficiency, in the absence of other factors. Foci of fungal infection are localized in different places in the patient. Most often, erosions appear in the mouth, on the nails, genitals, anal area, and esophagus. This disease can have quite serious consequences. For example, damage to the esophagus leads to the proliferation of the mucous membrane. The lumen gradually narrows or is completely blocked. That is why oropharyngeal candidiasis in HIV-infected people must be treated immediately.
Patients with AIDS are also characterized by debilitating folliculitis. The disease affects the hair follicles on the head and under the arms. Small purulent blisters form on the skin, which eventually burst, turning into ulcers.
Oral candidiasis in HIV
A fungal infection most often affects the oral mucosa. If any changes occur in this area, you should immediately contact a medical specialist and undergo a full examination of the body. Pseudomembrane candidiasis of the oral cavity is accompanied by the following symptoms:
- A gray-white coating forms on the mucous membrane.
- Under the layer of plaque, the surface of the palate, tongue and cheeks is covered with many painful ulcers.
- There is a burning sensation in the mouth.
The signs of the disease are very similar to the symptoms of hypovitaminosis (B, B6, C). Pathology can develop over several months. Oral candiosis with HIV can be localized in the corners of the mouth. In this case, epithelial hyperplasia develops and cracks appear.
Thrush (candidiasis) due to HIV infection
Thrush is a form of fungal disease. Another name for it is bacterial vaginosis. Don't think that thrush is a sign of HIV. In people with immunodeficiency, it occurs much more often, since the body’s protective functions are significantly weakened. However, such a pathology can also occur in completely healthy women.
The disease is accompanied by the following symptoms:
- Vaginal itching.
- Vaginal irritation.
- Pain when urinating, burning.
- White discharge.
Before you find out how to treat candidiasis in the mouth with HIV, you need to undergo a full medical examination and pass all the necessary tests. Most often, doctors prescribe complex medications, antibiotics. It all depends on the stage of development of immunodeficiency.
Treatment of candidiasis in HIV
Do not panic if you notice a white coating on your tongue; this does not indicate the presence of the disease. You can first see what oral candidiasis with HIV looks like in the photo. If the symptoms coincide, you should immediately contact a medical facility. Laboratory diagnosis of this disease is carried out in several stages:
- A blood test and biopsy material are examined to detect Candida fungi.
- A filamentous form of the microorganism is detected.
- Fungal infection in lesions is being studied.
- A urine test is collected.
Epitropic treatment of candidiasis in HIV infection is quite effective. The main goal of doctors is to destroy the cause of the progression of the pathology. Most often, special drugs are used to maintain immunity, as well as antifungal medications (Clotrimazole, Nystatin).