Ideal teeth size
In dentistry, teeth of a certain size and anatomical shape are considered normal, depending on the size of the jaw and their location in it. They must be smooth, fit tightly to each other and have a thickness within certain limits: for example, the height of the lateral incisors in an adult is normally 7 - 11 millimeters. Of course, this does not mean that they need to be measured with a ruler - overall aesthetics and proportionality are much more important (for example, for people of short stature and fragile build, a small teeth size is appropriate). Many parents are interested in why their child has small teeth, but usually there is no reason to worry: normally, the baby incisors are small and located at a distance from each other.
However, if the patient really has very small teeth, you should definitely consult a dentist to confirm or exclude the diagnosis of microdentia.
Installation of a bridge
The use of fixed orthodontic structures is a modern way to fill wide gaps in the dentition.
In order for the prosthesis to be securely fixed, it is necessary to have supporting dental units. It is on them that the entire structure is attached.
The best option is to make a bridge from metal ceramics. The service life of this design is 7 years or more. At the same time, the bridge retains its original shade and does not differ from adjacent natural teeth.
Contraindications to installing a prosthesis on rare teeth:
- Acute periodontitis.
- Parafunctions of the masticatory muscles.
- Insufficient height of supporting teeth.
If there are absolute contraindications, the doctor makes a decision regarding the advisability of using a different treatment method.
Diagnosis of microdentia
According to statistics, about 5% of people face the problem of microdentia – abnormally small teeth in an adult. There are several signs that allow you to distinguish microdentia from other dental pathologies.
Symptoms of microdentia
- teeth of regular shape, but with a significantly reduced crown;
- distances between teeth visible to the naked eye;
- damage mainly to the front teeth;
- wavy or jagged shape of the cutting part of the affected tooth.
In most cases, the presence of microdentia can be determined by visual examination of the patient, but for a more accurate diagnosis, hardware diagnostics are performed. For example, the doctor can measure the overall width of the incisors of both jaws using a special instrument, as well as resort to x-rays. A deviation is considered to be a reduction of teeth by 1.5 mm or more relative to the norm. Based on the results of the examination, one of three types of microdentia is determined.
Isolated
If the patient has one or two small teeth, then we are talking about isolated microdentia. Most often, the front incisors (mainly the lateral incisors) are underdeveloped.
Relative
Relative microdentia is said to occur when the patient has an abnormally enlarged jaw. On such a jaw, even normal-sized crowns can look disproportionately small. Thus, relative microdentia is an overly large gum and small teeth on it.
Generalized
In the most severe cases, when small teeth are located throughout the jaw, the patient is diagnosed with “generalized microdentia.”
Preparing for treatment
Elimination of the defect requires a comprehensive examination of the oral cavity and selection of optimal treatment. In particular, the doctor assesses the size of the pathological holes. An x-ray examination is also prescribed, which allows you to identify the presence of hidden injuries. Regardless of the chosen scheme, before starting treatment of rare teeth, therapy for caries and other pathologies of the oral cavity is prescribed.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
The most difficult operation to correct a malocclusion is implantation. Before it is performed, a panoramic photograph of the jaw is taken, which allows you to select the appropriate pin size.
Implantation is contraindicated in many cases. It cannot be used in the presence of oncological pathologies, tuberculosis, a number of chronic diseases and allergies to anesthesia. Implantation takes several hours. During the procedure, tooth extension is carried out in three projections: width, height and length.
After the operation, the patient should follow certain procedures for several months to prevent the development of complications.
Reasons why teeth become small
As a rule, most of the reasons leading to the appearance of small front teeth in adults come from childhood, when pathological processes interfere with the formation of body systems. Microdentia can be a consequence of:
- severe infections suffered before the age of 2 years;
- exposure to radiation;
- inflammatory diseases in the mother during pregnancy;
- early removal of baby teeth;
- underdevelopment of the alveolar ridge and, as a consequence, lack of sufficient support for “growing” teeth of normal size.
Are baby teeth treated?
It is believed that if a child’s baby tooth hurts, you shouldn’t fuss with it. Since it will fall out soon, you just need to tear it out and forget it. Indeed, a toothache can be a signal for a doctor to remove a tooth. But only if the doctor sees that there is nothing left to treat: the carious process has completely destroyed the tooth from the inside. Then a decision can be made to remove it.
But if the tooth can be saved, the doctor will do everything necessary for this. As in adulthood, teeth are not simply pulled out in childhood. If only because they have their own purpose in the oral cavity. A child with fewer teeth may have trouble eating. Difficulties may arise with the development of the speech apparatus and the pronunciation of certain sounds, which will subsequently require speech therapy correction. Finally, the beauty of a smile in the future also depends on the quality of care for temporary teeth and timely medical care in childhood.
pixabay.co/
To put it simply, each baby tooth “reserves” a place for a molar one. As a child grows, his jaw becomes larger. And larger permanent teeth occupy the areas reserved for them. Temporary incisors are replaced by permanent ones, and so are temporary molars. If voids appear in the child’s mouth, this can change the dentition and cause bite problems in the future. Temporary teeth may shift to the vacated areas, and molars will erupt out of place. Therefore, children who lose teeth as a result of injury or extraction when treatment is impossible are recommended to be monitored by an orthodontist.
“You need to treat baby teeth,” the doctor clarifies. — For this purpose, painless techniques are used in dentistry. If drilling is necessary, the doctor will use anesthesia. Until the age of four, local anesthesia is not used - only general anesthesia. This eliminates anxiety and pain in the child, and allows him to remain in place while the doctor is working. After four years, local anesthesia can already be used. The treatment is painless, slight discomfort is possible only during the “freezing”.
Dangerous consequences of microdentia
At first glance, it seems that small teeth in an adult cause only aesthetic inconvenience, but this is not so. Dentists identify several quite serious problems that microdentia can lead to.
- Distal displacement of teeth,
that is, their gradual shift back relative to the optimal position in the jaw. - The appearance of gaps between the teeth
(the so-called diastemas and threes), which lead to disruption of the contact of the lateral surfaces of the teeth. Without support, the ligaments in the dental bed stretch and the tooth becomes unstable. - Diction disorders,
excessive amplification of hissing and whistling sounds in speech. - Periodontal disease
is a disease of the soft tissues of the jaw, caused by accumulations of bacteria in the interdental spaces and an enlarged periodontal pocket due to the high mobility of the tooth.
Once again about teething in children
To begin with, let me quote Mark Twain: “Adam and Eve had many advantages over us, but their greatest luck was that they avoided teething.” All other representatives of humanity cannot avoid this routine process.
As it turns out, the physiological basis of teething remains as poorly understood as the onset of labor pains in women at a certain stage of pregnancy.
What is beyond doubt is the fact of the formation of teeth by the 40th day of embryonic life, the genetic determination of the eruption of primary (baby) teeth, as well as the role of various environmental factors in this process. Numerous theories and hypotheses that partially explain teething continue to be the subject of further debate [1–3]. This is clearly seen from the review work of I. Kjær [2].
The main modern ideas about teething are reflected in our relatively recent publication in the journal “Treating Physician” [1]. In this regard, we will not dwell on such trivial things as the order of teeth eruption, the first signs of dental calcification, crown formation and the actual eruption of teeth [1, 2]. All this information is clearly and clearly presented in the newest (21st) edition of the Nelson Textbook of Pediatrics (2020) [3].
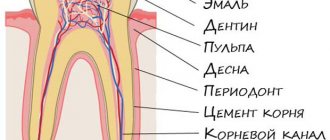
However, it is worth recalling the main four mechanisms that are of primary importance in the process of teething:
- tooth root growth;
- increased hydrostatic pressure in the periapical zone and/or in the dental pulp;
- reconstruction of dental bone tissue;
- the so-called “traction” of the periodontium [1].
New about teething
Every year more and more new data appears that expand our understanding of the phenomenon of teething in children. These data relate to the fields of immunology, genetics, endocrinology, perinatology and other areas of medical science.
SOB Franzolin et al. point to the role of mast cells in explaining the signs/symptoms of teething [4]. Based on fixing the number of mast cells in the pericoronal tissues at various phases of teething (intraosseous and submucosal) - in comparison with the calculated number of similar cells in the oral mucosa, Brazilian researchers come to the conclusion about the role of the following phenomena:
1) damage during chewing to the oral mucosa and dental follicles in the submucosa, which explains the susceptibility of the reduced enamel epithelium to the effects of connective tissue cells on the enamel; 2) the relationship between the exposure of antigenic enamel proteins and the release of sequestered antigens, which leads to the interaction of IgE with a large number of mast cells (regionally); 3) subsequent degranulation and local release of mediators such as histamine, leukotrienes, prostaglandins, proteases, cytokines and growth factors - in symptoms associated with teething [4].
H. Wu et al. indicate the presence of a complex of factors (maternal, prenatal and postnatal) associated with the eruption of primary teeth in children [5]. During the observation of 1296 mothers in the first trimester of pregnancy, these factors were studied by Chinese researchers in relation to the timing of primary teeth eruption in their offspring (in a national population). Infants were examined at 6, 9 and 12 months of age (dental examination). The average age of children at the time of the eruption of the first tooth was 6.82 ± 1.90 months in their observations.
Delayed teething in children was associated with older age of their mothers (β = 0.57, 95% CI = 0.13–1.02), female gender (β = 0.26, 95% CI = 0, 07–0.52), as well as low birth weight (β = 0.98, 95% CI = 0.20–1.76). In turn, macrosomia (β = –0.79, 95% CI = –1.30–0.28) was statistically significantly associated with earlier teething. Researchers from the People's Republic of China conclude that the age of the mother, the sex of the child, and body weight at birth are the most important determinants of the timing of the eruption of the first tooth [5].
Danish researchers S. Aziz et al. (2019) presented a description of a clinical case of the absence of primary teething in two siblings with a new mutation in the PTH1R (parathyroid hormone receptor 1) gene [6]. Previously, T. Yamaguchi et al. (2011) from Japan described a similar situation with mutation of the PTH1R gene among Japanese [7]. The role of genetic factors in teething is highlighted in the review by JM Richman [8]. A group of researchers from the USA and Japan A. Takahashi et al. presents the latest information on rare (syndromic) forms of primary teething disorders associated with a mutation in the PTH1R gene [9].
In relation to the teething process, Hunter's "root" theory and Yasvoin's "rocket" theory still deserve attention; they have the same right to exist as the Katz concept (pressure of a growing tooth on the lateral walls of the alveoli), Lukomsky’s concept (simultaneous development of the tooth/alveolar bone), as well as many others [1].
Helping children with teething and its safety
It should be noted that many years of debate among pediatricians regarding the possible influence of teething on the health of infants has come down to the recognition of the described influence. Evidence of this circumstance is the identification of teething syndrome in infants, that is, a condition that requires correction. It is even recognized by the International Classification of Diseases, 10th revision.
Since teething can be accompanied by pain, sleep disturbances, gastrointestinal disorders, hyperthermia, etc., the arsenal of remedies used for this condition varies from homeopathic and herbal remedies to non-steroidal anti-inflammatory drugs (NSAIDs): ibuprofen, paracetamol etc. [1, 3].
Among the drugs used in situations associated with teething in children, there are various dosage forms (powder, liquid, granular, gel) [10]. It is the latter - topical gels - that are currently particularly popular. Thus, N. Monaghan from Great Britain provides data according to which there are 14 varieties of teething products in the country; Of these, 2 contain sugar (sucrose), 6 contain alcohol, and another 6 contain lidocaine [11]. Nine of the analyzed products contained one or more undesirable ingredients [11].
L. Teoh and GM Moses from Australia question the safety of use, and even the need to abolish the use of topical gels containing lidocaine during teething in children [12]. They prepared a corresponding review, which examines cases of lidocaine-associated seizures, respiratory arrest, and even deaths as a result of the use of these topical gels [12]. The authors recall that in the USA, the FDA (Food and Drugs Administration of the United States, FDA) has banned the use of gels containing lidocaine for teething in children since 2014. This recommendation is currently followed by the American Academy of Pediatrics (AAP) and the Australian and New Zealand Society of Pediatric Dentistry (ANZSPD) [12].
Benzocaine and salicylates are no less dangerous ingredients in the products described above. Back in 2011, the FDA (USA) banned the use of benzocaine in products intended to correct teething symptoms in children [1]. The dangers of using benzocaine as part of oral medications are discussed in the publication of DS Aschenbrenner [13].
Information on the development of salicylate intoxication (methemoglobinemia, etc.) when using teething gels in children can be obtained from the recent work of T. Nguyen et al. (2018) from Australia, as well as from KE Hofer et al. from Switzerland [14–16].
Warning regarding potentially toxic and harmful topical gels for the child’s body is also expressed by S. Batra et al. from Pakistan [17].
Toxicological safety of teething gels
The second decade of the 21st century was marked by a significant tightening of requirements for the toxicological safety of drugs used in pediatrics. This is reported in the works of D. Tabersky et al., as well as R. Boetzel et al.
[18, 19]. An international database was created to assess the risk of using medical products with excessive levels of impurities of various elements [19].
K. Jurowski et al. - a group of researchers from Poland, Great Britain and Russia - presented a series of publications devoted to the toxicological analysis of herbal products (gels based on medicinal plant extracts) for the content of various elements [20–22]. Using plasma absorption spectrometry (FAS), the authors examined the content of copper (Cu), manganese (Mn) and zinc (Zn) in product samples; At the same time, the profile of the content of elements in the gels, the true content of elements in a single recommended amount of the gel (1 drop), and the daily exposure of these elements when using the gel in the maximum recommended amount were taken into account. It turned out that the content of Cu, Mn and Zn in the studied samples fully complied with the standards of the ICH Q3D directive (International Conference on Harmonisation's Q3D Guideline on Elemental Impurities) - the Q3D recommendations on elemental impurities of the directive International Conference on Harmonization [20].
The same team of authors, using the electrothermal atomic absorption spectrometry (ET AAS) method, studied the content of potentially toxic metals lead (Pb) and cadmium (Cd) in 5 samples of plant-based teething gels [21]. Although, as indicated, Pb and Cd were detected in all samples, their content fully complied with the standards of the ICH Q3D directive [21].
In addition, members of the described Polish-British-Russian team of researchers (K. Jurowski et al.) assessed the safety of the same topical teething gels for their nickel (Ni) and chromium (Cr) content - using the microwave-assisted method wet fermentation with concentrated nitric acid and electrothermal atomic absorption spectrometry [22]. The content of Ni and Cr fully complied with the requirements of ICH Q3D [22]. Thus, none of the studied plant-based gels posed a toxicological hazard (based on the analyzed element content) to children’s health [20–22].
Conclusion
N. A. Bogdanova and T. E. Zueva all types of gels used for teething are divided into four groups:
1) gels with an anesthetic effect based on anesthetic; 2) gels based on anti-inflammatory or antiseptic agents; 3) gels on a homeopathic basis; 4) gels based on extracts of medicinal plants [23].
The latter includes a topical gel of plant origin for teething in children, Dentinale® natura, which the authors prefer [23]. This position is quite understandable taking into account several circumstances: firstly, Dentinale® natura gel does not contain synthetic anesthetics and analgesics (lidocaine, salicylates, benzocaine); secondly, it contains no sugar and parabens; thirdly, it is harmless if swallowed; fourthly, it has a pleasant (attractive to a child) taste; fifthly, its components have anti-inflammatory, antiseptic and regenerating (wound healing) effects; sixth, when applied to the gums, this gel forms a protective film, reducing hypersensitivity, inflammation and irritation of the gums [1, 23].
According to information from the manufacturers, Dentinale® natura is a plant-based baby gel for teething gums and contains the following main ingredients:
- natural extract of Boswellia serrata resin;
- natural extract of chamomile flowers (Chamomilla recutita);
- natural extract of aloe leaf juice (Aloe barbadensis);
- natural extract of saffron (Crocus sativus);
- sweet orange peel oil (Citrus aurantium dulcis) [1, 23].
The medicinal properties of chamomile and aloe (agave) are well known in the Russian Federation and have been used in domestic medicine for many years [24]. Boswellia (frankincense tree, Indian incense) is less known to Russian doctors. At the same time, the resin extract of this plant is the main plant component of the Dentinale® natura gel. Boswellia is a tropical plant from the Burseraceae family, the medicinal properties of its resin are widely used in Ayurveda and folk medicine in many countries. In fact, Boswellia serrata extract is a natural substitute for NSAIDs [25]. A review by MZ Siddiqui details the properties of boswellia as an anti-inflammatory agent [26].
Not being a drug, Dentinale® natura gel has no contraindications for use (including age-related ones - during early teething) for use, as well as the previously described undesirable effects when using it. The safety and effectiveness of the drug are guaranteed both by its composition and the results of pre-registration studies.
"Noli nocere!" (“Do no harm!”) is the main commandment of a doctor and the oldest principle of medical ethics, attributed to Hippocrates. It is in pediatrics that it acquires special significance. The use of topical protective gels of plant origin for infant teething syndrome (K00.7) fully complies with them and avoids the use of potentially toxic/dangerous analgesics/anesthetics, as well as associated side effects and adverse events.
Literature
- Studenikin V.M. Teething in children: modern concepts // Attending Doctor. 2019; 1:7–11.
- Kjær I. Mechanism of human tooth eruption: review article including a new theory for future studies on the eruption process // Scientifica (Cairo). 2014; 2014: 341905.
- Nelson textbook of pediatrics. Kliegman RM, St Geme JW (eds.). 21st ed. Vol. I–II. Philadelphia. Elsevier. 2021. 4264.
- Franzolin SOB, Pardini MIMC, Francischone LA, Deffune E., Consolaro A. Explanation for the signs and symptoms of tooth eruption: mast cells // Dental Press J. Orthod. 2019; 24 (2): 20–31.
- Wu H., Chen T., Ma Q., Xu X., Xie K., Chen Y. Associations of maternal, perinatal and postnatal factors with the eruption timing of the first primary tooth // Sci. Rep. 2019; 9(1):2645.
- Aziz S., Hermann NV, Dunø M., Risom L., Daugaard-Jensen J., Kreiborg S. Primary failure of eruption of teeth in two siblings with a novel mutation in the PTH1R gene // Eur. Arch. Paediatr. Dent. 2019; 20 (3): 295–300.
- Yamaguchi T., Hosomichi K., Narita A., Shirota T., Tomoyasu Y., Maki K., Inoue I. Exome resequencing combined with linkage analysis identifies novel PTH1R variants in primary failure of tooth eruption in Japanese // J. Bone Miner. Res. 2011; 26(7):1655–1661.
- Richman JM Shedding new light on the mysteries of tooth eruption // Proc. Natl. Acad. Sci. US A. 2019; 116(2):353–355.
- Takahashi A., Nagata M., Gupta A., Matsushita Y., Yamaguchi T., Mizuhashi K., Maki K., Ruellas AC, Cevidantes LS, Kronenberg HM, Ono N., Ono W. Autocrine regulation of mesenchymal progenitor cell fates orchestrates tooth eruption // Proc. Natl. Acad. Sci. USA. 2019; 116(2):575–580.
- Painful teething: how to help // Local pediatrician. 2019; 5:12.
- Monaghan N. Teething products may be harmful to health // Br. Dent. J. 2019; 227(6):485–487.
- Teoh L., Moses GM Are teething gels safe or even necessary for our children? A review of the safety, efficacy and use of topical lidocaine teething gels // J. Paediatr. Child Health. 2020; Jan. 3. DOI: 10.1111/jpc.14769. .
- Aschenbrenner DS Warning for oral drugs containing benzocaine // Am. J. Nurs. 2018; 118(9):22–24.
- Nguyen T., Cranswick N., Rosenbaum J., Gelbart B., Tosif S. Chronic use of teething gel causing salicylate toxicity // J. Paediatr. Child Health. 2018; 54(5):576–578.
- Hofer KE, Kaegi S., Weiler S. The acute toxicity profile of a teething gel containing salicylamide in toddlers: an observational poisons center-based study // Clin. Toxicol. (Phila). 2018; 16:1–2.
- Hofer KE, Kaegi S., Weiler S. The acute toxicity profile of a teething gel containing alicylamide in toddlers: an observational poisons center-based study // Clin. Toxicol. (Phila). 2019; 57(3):220–221.
- Batra S., Ochani RK, Asad A. Teething gels: are they worse than we think? // J. Pak. Med. Assoc. 2019; 69(3):455–456.
- Tabersky D., Woelfle M., Ruess JA, Brem S., Brombacher S. Recent regulatory trends in pharmaceutical manufacturing and their impact on the industry // Chimia (Aarau). 2018; 72 (3): 146–150.
- Boetzel R., Ceszlak A., Day C., Drumm P., Gil Bejar J., Glennon J., Harris L., Heghes CI, Horga R., Jacobs PL, Keurentjes WJTM, King F., Lee CW, Lewen N., Marchant CA, Maris FA, Nye W., Powell S., Rockstroh H., Rutter L., Schweitzer M., Shannon E., Smallshaw L., Teasdale A., Thompson S., Wilkinson D. An elemental impurities excipient database: a viable tool for ICH Q3D drug product risk assessment // J. Pharm. Sci. 2018; 107(9):2335–2340.
- Jurowski K., Krosniak M., Folta M., Tatar B., Cole M., Piekoszewski W. The toxicological analysis of Cu, Mn and Zn as elemental impurities in pharmaceutical herbal products for teething available in pharmacies in Poland // J. Trace Elem. Med. Biol. 2019; 53: 109–112.
- Jurowski K., Krosniak M., Folta M., Tatar B., Cole M., Piekoszewski W. Toxicological analysis of Pb and Cd by ET AAS in local anaesthetics for teething (teething gels) based on herbs available in Polish pharmacies // J. Trace Elem. Med. Biol. 2019; 52: 18–21.
- Jurowski K., Krosniak M., Folta M., Tatar B., Cole M., Piekoszewski W. Safety assessment of the trace element impurities Ni and Cr in pharmaceutical herbal products for teething from Polish pharmacies // Biol. Trace Elem. Res. 2019; 191(2):517–521.
- Bogdanova N. A., Zueva T. E. How to help a child with teething? A new look at an old problem // Medical Council. 2019; 11:50–55.
- Nutrients, conditional nutrients and antinutrients in neurodietology of childhood (handbook) / Ed. Studenikina V. M. M.: Dynasty Publishing House, 2021. 184.
- Moussaieff A., Shohami E., Kashman Y., Fride E., Schmitz ML, Renner F., Fiebich BL, Munoz E., Ben-Neriah Y., Mecholaum R. Incensole acetate, a novel anti-inflammatory compound isolated from Boswellia resin, inhibits nuclear factor-kB activation // Mol. Pharmacol. 2007; 72(6):1657–1664.
- Siddiqui MZ Boswellia Serrata, a potential anti-inflammatory agent: an overview // Indian J. Pharm. Sci. 2011; 73(3):255–261.
V. M. Studenikin, Doctor of Medical Sciences, Professor, Academician of RAE and MAE
OOO NPSMC "Dream Clinic", Moscow
Contact Information
DOI: 10.26295/OS.2020.50.78.008
Once again about teething in children / V. M. Studenikin For citation: Attending physician No. 2/2020; Page numbers in issue: 50-53 Tags: baby teeth, pain, hyperthermia, topical gels
How to fix small teeth?
Small tooth: what to do if it causes inconvenience, reduces self-esteem and worsens quality of life? Depending on the severity of the picture, the dentist may suggest the following correction methods:
- In case of isolated microdentia, small teeth can be corrected by installing veneers or lumineers - thin plates that are attached to the front surface of the tooth. This method is also suitable for eliminating threes and diastemas and increasing the width of the visible part of the crown. If your teeth grow unevenly, you will most likely need orthodontic correction using braces before placing veneers.
Sealing
Currently, it is one of the most affordable ways to treat rare teeth. Its wide distribution is due to its low cost and ease of implementation.
The essence of the method is as follows: fillings of the same color as the natural chewing units are applied to the teeth. The procedure is considered a jewelry procedure, since the doctor must literally mold new bone structures. As a result, the teeth become wider and the gaps between them disappear. Only a specialist can visually distinguish fillings from natural dental units.
During the procedure, orthodontists use only high-quality materials. These are ceramics and porcelain.
After filling rare teeth, the functioning of the gastrointestinal tract is normalized and a correct bite begins to form.
Installation of crowns
These are non-removable structures that can be used to eliminate dental defects. The installation of crowns is also indicated in case of severe destruction of dental units. The essence of the method is to insert an artificial tooth into the gum using a pin made of metal.
Installing crowns requires some preparation. The patient's natural teeth are prepared and, if necessary, pulp removal is performed. Crowns take several days to make. During this period, the patient is provided with temporary structures. The finished crowns are completely identical to the patient’s teeth. They differ only in width, which makes it possible to hide large gaps between chewing units.
The following conditions are contraindications: loose teeth, allergic reaction to the components used, periodontal pathologies. In addition, crowns are not placed on anyone under 16 years of age.