Taking into account the prospects, convenience and functionality, the most reliable method of replacing lost teeth today is implantation, in particular, express implantation - installing an implant simultaneously with the removal of the problem tooth. It allows you not only to restore the aesthetics of the dentition, but also to eat normally, without limiting yourself to your favorite foods, moreover, it is the most durable method of prosthetics of all existing ones. However, sometimes a patient may experience complications after dental implantation. They appear extremely rarely, but there is still a risk of their development, especially when the patient does not accurately follow medical recommendations after dental implantation. What difficulties may arise with this type of prosthetics and how can they be prevented?
Myth 1: Missing one tooth is not a reason for implantation
Unfortunately, the absence of even one tooth can negatively affect the entire oral cavity. Over time, the patient may begin the process of thinning bone tissue , and neighboring teeth will change their position and noticeably shift , which will lead to the appearance of a malocclusion or its weakening. In the future, the quality of speech and diction will be impaired , muscle tone will decrease and problems of the gastrointestinal tract . Believe me, it is better to place an implant on time , visiting the clinic two or three times, than to treat the entire body for several years.
What is Zoom 3 whitening
Zoom 3 teeth whitening is based on the use of a special gel. It does not contain acids or other aggressive substances that negatively affect the enamel. The main component of the whitening gel is hydrogen peroxide. When exposed to light, it decomposes and releases active atomic oxygen. It quickly reacts with pigments, forming stable compounds. Thanks to the activity of oxygen, it is able to penetrate even into the deep layers of enamel, so Zoom 3 allows you to quickly lighten it by several tones.
The procedure lasts about an hour. After this, even the most persistent pigments are removed from the surface of the teeth. At the same time, there is no harm to the enamel and dentin. It is impossible to damage teeth during Zoom 3 whitening.
Zoom 3 is one of the most effective methods in aesthetic dentistry. With its help you can lighten your teeth up to 12 shades. Since the procedure is safe, it can be done regularly. We recommend whitening every year to help you maintain a snow-white smile.
Myth 4: Implants often fail
This statement is incorrect. Our specialists use only truly high-tech implants the risk of rejection is minimal , and the materials used in the work do not cause allergic reactions in almost 100% of cases.
The survival rate of implants installed at the Istok Health Clinic is 98.5% - 99%.
Before deciding to undergo implantation, we advise each patient to have an appointment with a qualified specialist to identify individual intolerance to certain components - this will help maintain your health and eliminate the risks of possible rejection.
Why does numbness in the upper or lower jaw persist after implant installation?
Often, after placing an implant, temporary complications arise in the form of loss of sensitivity, aching pain, bleeding and redness of the gums, swelling - all this is a normal reaction to surgery. Usually paresthesia goes away without a trace after 3-5 hours, all other symptoms - after 4-6 days.
There is no need to delay a visit to the doctor if numbness lasts more than five hours . It can occur either due to the effect of anesthesia or due to:
- poor preparation for surgery, incorrect selection of implants, the site of their integration;
- injuries of the mandibular trigeminal nerve.
Myth 6: Implantation is very painful
Another myth that worries many patients. The installation of an implant at the Istok Health Clinic takes place under anesthesia , during which the person does not experience any pain, and our specialists approach such “jewelry” work very delicately. If you are terrified of even having your teeth treated, then in our clinic there is the possibility of anti-stress treatment and dental implantation under sedation and in your sleep! The occurrence of edema the next day is a natural reaction of the body, which fades away over time without any consequences. To make the recovery process much faster, the patient is prescribed painkillers in tablets, which are important to take before a certain date.
What to do, how to treat
Treatment of paresthesia due to unsuccessful implantation can be prescribed by the implantologist who performed the operation, dentist, neurologist, or physiotherapist.
Before moving on to restorative therapy, a diagnosis must be carried out, during which the nature and extent of the damage is established. The treatment is carried out comprehensively, aimed at restoring the conductivity and sensitivity of nerve fibers .
If the patient consults a doctor immediately, drug therapy in combination with physiotherapeutic procedures is very effective. In other cases, surgery is required.
Myth 8: Implants require special care
In fact, caring for an implant is exactly the same as with regular teeth , using toothpaste, a brush and dental floss. To ensure thorough cleaning of the entire oral cavity, we recommend purchasing an irrigator for daily use and visiting the clinic for professional hygiene once every six months.
As you can see, many myths have been invented about implantation, but many of them are far from the truth. Come for a consultation with a doctor and find out reliable information from a specialist.
Recommendations after dental implantation
Statistics on dental implant failure indicate that the main reason for this outcome is the human factor*. Therefore, in order to avoid unnecessary complications, it is necessary to carefully choose the dentist where to place dental implants. It must be equipped with modern equipment, use high-quality implants that meet all standards, whose manufacturers must provide a guarantee in case of implant failure. Implantologists must undergo special training and have experience in performing such operations. Reviews from real patients of the clinics will be a good help in the difficult task of choosing a clinic that meets these criteria. And, of course, do not forget about the basics – regular and high-quality oral hygiene.
All consequences and complications after dental implantation can arise due to the fault of both the doctor and the patient, and sometimes an “X factor” independent of anyone plays a role. It is worth remembering that complications after implantation are still an exception to the rule. Therefore, you should boldly say to this unique technique: “YES!”
*Research data from the international company Nobel Biocare Russia
Benefits of the procedure
- Possibility of fast high-tech teeth whitening by 8-12 shades;
- Gentle effect on teeth compared to other similar procedures;
- Preservation of the original strength and chemical composition of tooth enamel;
- High stability of bleaching compared to other similar procedures;
- Preservation of the result for up to 5 years, subject to instructions;
- Maximum safety for teeth and patient health in general, confirmed by the results of various clinical studies.
Treatment options
If the nerve trunk, plexus or branches of the nerve are damaged or compressed, there are two ways to solve the problem.
The first is to leave everything as is, without performing surgery. Such a solution to the problem is acceptable in case of incomplete loss of sensitivity or a small area of focus, with the exception of cases with displacement of the denture. Compression of the nerve due to regenerative processes will stop progressing after a certain point, “frozen” in one place. Odontogenic sinusitis can be treated with medication using antibiotics.
The second method is to perform surgery. The operation is indicated for injuries during sinus lifting and bone grafting, displacement of dentures or bone mass, extensive or complete loss of sensation. During the operation, the cause of the numbness is eliminated and, if necessary, the damaged nerve is sutured. Restoration of sensitivity takes a long time, sometimes never returning to its original state.
Features of Zoom 3 whitening technology
The main distinguishing feature of Zoom 3 technology from other teeth whitening methods is safety and complete protection of oral tissues from possible damage. Harm and injury are completely excluded. Hydrogen peroxide is the main, but not the only component of the gel. It contains calcium phosphate. During the Zoom 3 procedure, it also penetrates the enamel, providing additional strengthening. Therefore, my teeth are less at risk of caries and destruction.
Hydrogen peroxide decomposes when exposed to ultraviolet light. The doctor adjusts the wavelength in such a way as to eliminate the risk of tissue overheating. Thanks to this, the ultraviolet lamp also does not harm teeth and soft tissues.
Problems in the upper jaw
Numbness after sinus lifting and bone grafting in the area of the upper teeth and gums is less common than in the lower jaw. This is due to the fact that the innervation of these structures is carried out by three groups of branches of the maxillary nerve, intertwined with each other and forming the dental nerve plexus. Such a structure is quite difficult to damage or completely disable.
The loss of sensitivity in the area of the upper lip and upper half of the cheek cannot in any way be associated with dental interventions due to the fact that completely different branches of the maxillary nerve go to them.
Damage to the alveolar branches or dental plexus
This complication can only develop in conjunction with penetration into the maxillary sinus during surgery, which should not occur if the operation is performed correctly.
Local, mild numbness develops. One or two teeth may be involved with incomplete loss of sensitivity.
Improper placement of the implant or complications in the postoperative period
Dislocation of the skeleton of a prosthetic tooth can occur due to injury, inflammatory processes, or neglect of the dentist’s recommendations. Diagnosis of this condition is not particularly difficult due to the obvious pathological state of the implant.
There may be loss of sensitivity due to chronic odontogenic sinusitis. The condition develops over a long period of time, occurs with severe symptoms of sinusitis, and numbness develops in extremely severe and advanced cases.
Implant opening – what is it?
Expansion of the implant is only necessary in case of two-stage implantation. This procedure is carried out after the implant has healed, but before the prosthetic stage. For understanding, we will briefly describe the implantation process according to the classical protocol.
Stage 1. Implant installation.
To gain access to bone tissue, the doctor makes an incision in the gum and then a hole in the bone at the site where the future implant will be installed. After implantation of an artificial root (implant) with a plug, the gums are sutured - this is necessary for successful osseointegration (engraftment) of the structure and to prevent infection. Next comes the engraftment process - approximately 3-6 months.
Stage 2. Orthopedic stage.
Installation of the gum former.
After the implant has taken root, the doctor performs the following manipulations.
- Using a scalpel, the implant is exposed;
- assesses the condition of the artificial root;
- removes the plug;
- installs the gum former.
The procedure is performed under local anesthesia.
Installation of abutment and crown.
Why is the gum exposed under the implant?
Implant exposure is a fairly common occurrence. More common with two-stage implantation. A characteristic sign is the exposure of the metal rim of the abutment under the prosthesis, resulting in the formation of a black stripe . Usually the defect makes itself felt some time after the operation.
Common causes of complications:
Exposed gums under the implant significantly spoil the aesthetic appearance of the dentition
- using an implant with a polished neck that remains above the bone surface after screwing in;
- too thin mucous membrane;
- overtension of the gingival flap;
- temporary crown pressure;
- poor quality oral care after implantation;
- mechanical trauma to the gums (toothbrush, hard food);
- improper formation of the gingival margin;
- subsidence of the bone as a result of long-term use of artificial teeth.
Peri-implantitis - symptoms and treatment
Peri-implantitis is an inflammation of the tissue surrounding the implant, which leads to progressive bone loss and implant loss.
The precursor to peri-implantitis is mucositis - inflammation of the gums without compromising the integrity of the bone tissue. It occurs in almost 80% of people with implanted teeth. If it is not diagnosed and treated promptly, the inflammatory process can spread along the body of the implant and lead to the development of peri-implantitis. Such cases occur in no more than 5-15% of cases [3], and according to other studies - in 11-28% [4][5][24].
The main cause of peri-implantitis is infectious agents, i.e. microorganisms that are found in the biofilm on the surface of the implant. Local and general factors contribute to their occurrence.
Common factors for the development of peri-implantitis:
1. History of periodontitis . Studies show that the risk of developing peri-implantitis is much higher in those who have had periodontitis (23%) than in people without it (7%) [9]. This is due to periodontal pathogenic bacteria that can be transferred from teeth to implants. Therefore, before implantation, it is necessary to undergo comprehensive treatment of periodontitis [11].
Also, the development of peri-implantitis after periodontitis can be caused by a high concentration of cytokines - special proteins that increase the activity of osteoclasts - bone cells that contribute to its destruction. This factor is hereditary [6][7].
2. General somatic diseases:
- Systemic blood diseases - leukemia, agranulocytosis, coagulopathy, anemia. They are an absolute contraindication for implantation.
- type 1 and 2 . The development of peri-implantitis in this case depends on the severity of the disease, which can be determined by the level of glycohemoglobin - the content of sugar in the blood over a long period. The risk of peri-implantitis increases if the level of this indicator is above 7%. However, against the background of maintenance therapy and compliance with all doctor’s recommendations, the incidence of peri-implantitis remains average, as in people without diabetes [29].
- Thyroid diseases - hypothyroidism (deficiency of thyroid hormones). It is also a contraindication for implantation [12].
- Autoimmune diseases - lupus erythematosus, scleroderma (connective tissue diseases).
3. Environmental factors: smoking , stress, alcohol . Smoking patients are 3.5 times more likely to develop peri-implantitis than non-smokers. On average, they lose up to 0.16 mm of bone around the implant per year [17]. Nicotine entering the blood causes vasospasm and impairs blood supply, which reduces the speed and completeness of fusion of bone tissue with the surface of the implant [20].
4. Genetic predisposition . According to the results of a study conducted in 2021, heterozygous mutations were identified in 82.8% of patients with peri-implantitis, and complete mutations in another 9.1% [8].
5. Taking bisphosphonates or drugs that affect bone metabolism . In the treatment of osteoporosis and cancer, patients are often prescribed drugs that inhibit bone self-destruction. They affect the process of new bone formation, including around the implant [11].
Local factors for the development of peri-implantitis:
1. Infectious agent that forms a biofilm. Immediately after installation of the implant, a layer of salivary glycoproteins forms on the surface, which is populated by microflora, which leads to the appearance of a bacterial film. The main causative agents of the disease are peptostreptococcus (p. micros), Plaut's bacillus, gram-negative anaerobes, Staphylococcus aureus and other microorganisms. All of them are present in the oral cavity and are also causative agents of periodontitis [19].
2. Autoimmune-autolytic reactions - self-destruction of bone tissue. Bone loss in this case occurs due to a change in the balance towards osteoresorption - resorption of bone tissue [13].
3. Insufficient oral hygiene leads to a rapid increase in the number of bacteria, which aggravate the inflammation process [2].
4. The roughness of the structure under the gum increases the adhesion of microorganisms to the surface of the implant. It has been proven that the smoother the surface, the fewer microorganisms remain on it [31].
5. Mismatch between pin and superstructure . The superstructure consists of an abutment (gum former) and a crown. It is fixed on top with a pin. If these structures do not correspond to each other, microorganisms accumulate at their junction. This leads to the entry of bacteria into the implant shaft and the contamination of its internal surface with microbes [1][10].
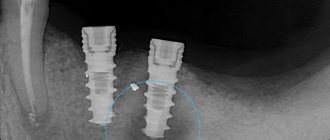
6. Biomechanical complications - weakening of fixation of abutments or screws, violation of cement fixation, remains of impression material. Cement is often used to secure the crown to the abutment. Sometimes it remains under the gum and leads to the development of peri-implantitis. This can be detected on an x-ray. After removal of the cement, in more than 2/3 of cases, the signs of peri-implantitis significantly decrease or disappear completely [23][25].
7. Level of connection between the pin and the abutment .
The higher this connection is located, the lower the risk of developing peri-implantitis [27].