Causes of obstruction of dental canals
The root canals of teeth can become obstructed for a variety of reasons. The most common include:
- features of the anatomical structure of the tooth - highly curved roots with small branches, flattened areas and transverse bridges;
- inflammatory processes in the neurovascular bundle - with dental injuries and chronic pulpitis with a subacute course, the root canals can become overgrown;
- age-related changes in tissues - over time, dentin deposits accumulate on the walls of the root canals, which lead to a narrowing of the lumen;
- dental procedures using phosphate cement - this material has a high density and cannot be destroyed by ultrasonic waves, instruments and solvents.
Before starting endodontic treatment, it is important to accurately determine whether the canals are patent.
Conservative treatment method
This method allows you to keep the nerve alive. This is a more preferable option, which is possible in case of a minor inflammatory process, or in the presence of a deep carious lesion, in which the lesion is close to the root, but has not yet had time to fully move to the pulp. In addition, complete and rapid nerve regeneration is possible mainly in young patients under 25-30 years of age due to the physiological characteristics of the structure and functioning of the pulp.
During the conservative treatment method, carious tissue is removed, after which a special medication is applied on top of the nerve. A temporary filling is fixed, which will reliably cover the area from bacteria and plaque. Such treatment can be repeated - the doctor assesses the condition of the dental nerve using X-rays and if the pulp regeneration is insufficient, the medicine can be prescribed for a few more days. After therapeutic treatment, the temporary filling is removed and replaced with a permanent one.
Surgical method of treatment
The surgical method is more common in the treatment of pulpitis, since the pulp most often cannot be cured and it is necessary to remove it so that the inflammatory process does not spread to the tissues around the tooth. This procedure is called depulpation or endodontic treatment.
Diagnostics
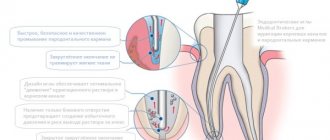
Treatment of impassable root canals begins with determining their length and anatomical features. The most informative diagnostic method is radiography. To obtain accurate data on the condition of the tissues, a photograph of the tooth root is taken with the instrument inserted into it. This allows you to see:
- length of root canals,
- the presence of curvatures and perforations,
- impassable areas.
The condition of the periodontium is also assessed. This allows you to determine further treatment tactics.
How canals are treated for pulpitis?
The cost of treating pulpitis directly depends on the number of tooth roots or canals - this affects the amount of work the dentist must do, as well as the amount of materials used.
The nerve removal itself is carried out as follows:
- administration of local anesthesia: treatment of pulpitis is a rather painful procedure, especially if there is still a living nerve, however, modern anesthetics can completely relieve the patient of pain for the entire duration of the operation,
- removal of all carious formations in the area of the tooth crown - this provides access to the tooth root,
- direct nerve removal : an extractor (a special surgical instrument) is used with which the doctor grabs the nerve and extracts it from the tooth root,
- expansion of the dental canals: required for better cleaning of the canals from the nerve, as well as so that the tooth root can be fully filled, without the presence of voids. The expansion is carried out using thin burs, which allow you to level the canal, make it smooth (initially it consists of many narrowings and expansions),
- cleaning of the canals: carried out with antiseptic agents, which allow you to remove foci of infection and pulp residues, as well as strengthen adhesion to filling materials,
- canal filling: a special filling material (gutta-percha) is placed along the entire length of the tooth root - initially it has a viscous state, which allows filling even lateral micro-channels. The top of the tooth is also filled with composites; if necessary, it may be necessary to install a large inlay or crown.
At all stages of treatment, doctors use a microscope - modern equipment that allows you to examine details even deep in the canals! In addition, it illuminates areas, which allows you to remove inflamed tissue in a gentle way, without damaging healthy tissue. Such a microscope, combined with the professionalism of our doctors, is a guarantee of high quality treatment.
What are the advantages of a microscope for root canal treatment?
- highly accurate diagnosis – lesions are visible at the earliest stages,
- gentle treatment – healthy tissue is preserved as much as possible without unnecessary drilling,
- high-quality processing - hard-to-reach areas, micro-gaps and roughness that require attention are clearly visible,
- treatment of complications: a microscope allows you to detect and remove broken instruments, restore perforated walls of dental canals,
- a chance for “hopeless” teeth - they can be saved, and not removed and replaced with a denture!
We treat carefully and responsibly! We use not only modern equipment (microscope, laser), but also nanomaterials for filling. We preserve living tissue and extend the life of the tooth for many years!
Enroll now
Features of treatment
Various techniques are used to treat impassable root canals:
- devital amputation of the pulp followed by mummification,
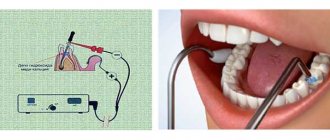
- depophoresis.
A special approach is required if the root canal:
- strongly curved
- completely closed,
- narrowed,
- is located next to the neighboring root.
To make the canal passable along its entire length, modern dentistry uses:
- durable extractors - nickel-titanium files, which allow you to go through the canal without preliminary tooth preparation;
- drills - special instruments with spiral blades designed for quick and safe removal of gutta-percha, pastes, cements and other filling materials;
- solvents - necessary for unsealing previously sealed canals; they cope well with soft and plastic materials.
The treatment tactics for impassable root canals in each clinical case are determined by the doctor. The procedure is performed under anesthesia. Depending on the complexity, treatment is carried out in one or several stages. To obtain the desired result, 2-3 visits to the dentist may be required.
This is how nature works that a seemingly small tooth turns out to be a very complex organ. Under the strong shell of hard tissue hides a very delicate substance - “tooth pulp” - tissue formed by a community of nervous tissue and blood vessels. It is needed to provide nutrition to the tooth tissues from the inside, as well as to form chewing reflexes. But very often, unfortunately, it happens that we, dentists, are forced to remove this very useful tissue. There are a great many reasons for such an operation (precisely an operation, since canal treatment is equal in complexity to microsurgery), but they can be reduced to three main points:
1. The presence of inflammation in the pulp. The entry of an infection into the pulp always leads to very violent inflammation - those same terrible toothaches that make you “want to climb on the ceiling” are precisely caused by the inflamed pulp. And due to its biological characteristics, the “dental nerve” is not able to recover - any inflammation always ends in gangrene. Similarly, the “nerve” can die with long-standing deep caries from exposure to bacterial toxins. And dead tissue must be urgently removed before it poisons the surrounding healthy tissue.
2. Pulp injury. A sharp, strong blow to the tooth or prolonged overload (for example, with the constant clicking of seeds) can lead not only to the destruction of hard tissue, but also to the death of the pulp, even without exposure to an infectious agent. In this case, the tooth may not even hurt, and only a change in color may indicate that the tooth is dead.
3. Preparation for prosthetics. Before covering a tooth with a crown, the orthopedic doctor is forced to remove approximately 2 mm of hard tissue from the tooth, and this is quite a large volume. If the tooth had a small crown or was tilted, then during processing the tooth cavity may open and the pulp may be exposed. In addition, supporting teeth are often overloaded. All this inevitably leads to the death of the “nerve”, and therefore, before prosthetics, it is recommended to subject all questionable teeth to “depulpization”, that is, removal of the pulp.
Thus, if there is a reason to remove the “nerve” from the tooth, then, unfortunately, there is no escape from this procedure (well, perhaps only in the third option, and then only at your own peril and risk - after all, for high-quality removal of pulp from It is recommended to remove the crown of a “crowned” tooth). After all, if endodontic treatment is not carried out, toxins from the dead pulp will slowly leak out of the tooth, poisoning the surrounding healthy tissue.
How does the depulpation process take place?
First, the doctor numbs the working area - nerve removal is always carried out under anesthesia. Afterwards, the tooth cavity is carefully opened. This is necessary so that the doctor can not only find all the root canals (these are tunnels in the roots of the tooth where nerves and blood vessels pass), but also process them efficiently. This is a very important stage - after all, a tooth can have from 1 to 4 (and in some cases even 5) canals, and each of them must be properly treated. The golden rule of endodontics says: “The quality of tooth treatment is assessed by the most poorly treated canal.”
After finding all the canals and determining their anatomy, the stage of mechanical and medicinal cleaning and treatment of the canals begins. It boils down to the fact that the doctor, using special thin instruments, removes all organic matter from the canal (so beloved by microbes) and gives it the shape of an even cone - this shape is convenient for subsequent washing and filling. After which the canal is thoroughly washed from dentin sawdust and pulp residues with special antiseptic solutions. Sometimes ultrasound or laser sterilization of the canal is also added to the medicinal treatment, and in very advanced cases (when there was a lot of infection in the canal), you can fill the canal with a special disinfecting paste and leave it for several days.
Finally, after the dentist has achieved maximum sterility of the root canals, the stage of filling them begins.
Here are a few criteria that must be strictly met when carrying out high-quality endodontic treatment:
1. Treatment and filling of canals must be carried out under anesthesia.
2. Endodontic treatment should be carried out under radiographic guidance.
3. The channels must be sealed hermetically.
4. Control x-ray after a year. The dentist can guarantee compliance with the treatment protocol, but the outcome of the treatment is determined by the patient’s body.
Repeated canal treatment.
Root canal treatment is one of the most difficult procedures in modern dentistry. Its outcome is influenced by many factors, from the physiological characteristics of the patient to the technical equipment of the dental office. Even the doctor’s mood and feeling of fatigue play an important role here. It is not surprising that a very large percentage (some researchers indicate as much as 80%) of previously treated canals require re-intervention. In most cases, the decision on the need for repeated endodontic treatment (the words “revision” are also used) is made based on the results of x-ray diagnostics.
So, what could serve as a reason for revision:
1. The root canal is not completely filled or not filled at all. It is also possible that the root canal was impregnated with resorcinol-formalin resin, which is not visible on x-rays and therefore cannot confidently assess the quality of treatment.
2. The canal is completely sealed, but the filling material is not dense enough. This most often happens when filling a canal with paste - the method is quite simple, but does not provide the necessary tightness, which in turn again leads to the spread of microorganisms and the emergence of foci of chronic inflammation.
3. The canals are sealed satisfactorily, but there is a focus of inflammation at the root. This happens when there is an infectious focus in the canal.
These reasons are the main reasons for repeated endodontic treatment. The worst thing in the situation of “poorly treated root canals” is that such a tooth may not cause any discomfort. A fair question arises: “So why re-treat them? They don’t hurt!”
The fact is that such teeth are like time bombs. There is a constant and continuous struggle between your immunity and bacteria. As long as the body copes, everything is fine. But as soon as it loosens its “grip” (for example, during a cold or after hypothermia), the bacteria quickly go on the offensive and then you will be left with flux and a sleepless night. And it’s very disappointing if this happens under a freshly installed metal-ceramic crown. Moreover, cardiologists have long proven that the presence of such “harmless” foci of inflammation greatly increases the risk of such a serious disease as bacterial endocarditis.
So, there is only one conclusion - if the root canals are poorly treated, they definitely need to be re-treated.
However, sometimes, even if there are indications for retreatment, dentists are forced to abandon canal revision, for example:
1. High risk of complications during treatment. Initially, the canal treatment procedure itself is very complex, and “correcting other people’s mistakes” is much more difficult. Naturally, as the difficulty of the procedure increases, the risk of complications also increases. Therefore, if the possible harm to the tooth from revision is higher than the predicted benefit from re-treatment, it is better to refuse. Best the enemy of the good
2. Long-term favorable course. If the problematic tooth was treated more than 5 years ago and the x-ray shows no signs of an inflammatory process, and the tooth itself has not caused concern during all this time, then we can assume that the body in this case has won a final victory over the bacteria. This means that no treatment is required.
3. Presence of concomitant pathologies. If a tooth, in addition to poorly treated canals and foci of inflammation, also has deep periodontal pockets, or its crown is severely destroyed, then the question of the advisability of treating such a tooth always arises, because even with well-treated canals, such a tooth may need to be removed.
Let's look at the root: how are the root canals of teeth filled?
The more a person is afraid of dentists, the more closely he eventually has to interact with them and the longer the dental treatment will be for him - a simple and banal truth, but, unfortunately, not all people take note of it. If caries treatment is not carried out in a timely manner, the infection gradually spreads “inward”, capturing more and more new territories and reaching the pulp chamber. Pulpitis develops - an extremely painful and unpleasant disease, which is popularly called “inflammation of the dental nerve.” This is where most people don’t just go to the dentist, but run – because the pain prevents them from sleeping, eating, or working normally. And if the patient has already begun to have inflammation of the tooth canals, treatment will require quite serious and lengthy treatment: cleaning the tooth canals from infected and dead tissue, their special antibacterial treatment, careful filling of both the canals themselves and the dental crown with the cavity.
Almost everyone knows about such a dental procedure as treatment and filling of dental canals, and many people have encountered it from personal experience. But most people usually don’t know the intricacies of the process, how exactly such treatment takes place, why it is needed and what it gives in the end. So what are the standards for filling canals, why and how exactly is this procedure carried out, and what can a poorly filled canal threaten a patient with? Dentist-therapist at the 32 Dent clinic Larisa Aleksandrovna Kravtsova will help you get reliable answers to all these questions.
Pain after root canal treatment
It happens that after root canal treatment, the molar should completely lose sensitivity. If pain in the tooth remains after removal of the nerve, then you need to continue therapy. Possible causes of the disease:
- The dental instrument used to clean canals is very thin. There are times when part of it breaks off and remains in the canal as a foreign object. An X-ray after filling is also needed to determine the boundaries of the filling. It is worth making sure that there is no unsealed space left in the canal. Incomplete filling will lead to inflammation and spread of infection in the tooth;
Preparation
Tooth canals are treated in the following cases:
- When treatment of pulpitis and periodontitis is necessary;
- Sometimes in preparation for prosthetics;
- If poor-quality treatment has already been carried out and the canal needs to be filled again.
Pulpitis is the most common cause of pulp problems and the need for root canal treatment. Preparation for the procedure is carried out very thoroughly - it is necessary to take an x-ray so that the doctor finds out the cause of the inflammation and examines the configuration of the canals. It is also advisable to do allergy tests to make sure that the patient is not allergic to the filling material or anesthetic. And only after that the procedure itself begins.
What materials are used to fill canals?
The main requirements for such filling materials are dense, hermetically sealed filling of the canals, chemical inertness (the material should not dissolve under the influence of body fluids), radiopacity (it should be clearly visible in the picture). Today, the following types of materials are used for filling dental canals:
- Solid fillers (fillers).
These include gutta-percha (a latex processing product), silver and titanium pins. Silver pins have recently been rarely used, since despite their good antibacterial properties they have a significant drawback - they do not provide complete tightness. - Polymer and natural pastes (sealers)
. A more preferable option is polymer sealers, which adhere better to the walls, do not stain dental tissue and do not dissolve when interacting with tissue fluids. - Glass ionomer cements.
Good adhesion and radiopacity, high biocompatibility and minimal shrinkage are the main positive qualities of such materials. They also have significant drawbacks: low strength, which is why such fillings are short-lived and not designed for serious functional loads. - Calcium hydroxide cements
. Non-toxic, biocompatible, radiopaque materials that exhibit minimal shrinkage, are easily removed if necessary and have bactericidal properties. However, they are considered not too strong and can break under heavy loads on the dental crown. - Polydimethylsiloxanes
. Modern reliable sealants with good therapeutic and operational parameters. Perhaps their only drawback is that this is a new product on the dental market and experience in using such materials has not yet been accumulated. There is no reliable information yet about the experience of patients after such treatment.
The nerve was removed, but the canal was not sealed
Such situation. On the X-ray of my teeth, they saw that in my six, in which the nerves were ripped out, only one canal was sealed. My employee’s nerve was removed and the canal was also not sealed - the filling was only placed on top. The fillings are not temporary, but permanent. It turned out to be completely random - during a check when another tooth (mine) was hurting. And the employee was sick after that, the hollow one.
Is there any reasonable explanation for the fact that the nerve is removed, but the canal is not filled and the filling is left only on top, or is this real negligence?
There are several options. Possibly negligence. But if one channel is sealed, then most likely there is another option. I haven't completed channels 5 and 6 yet. This turned out to be the case in the USA. The previous dentist in the USA turned a blind eye to this. We moved and took the new one to a specialist to do a refilling. Well. I did it in a cool place, with a cool specialist, a professor. I paid more than 3 tons of dollars for two teeth (5 and 6 on the lower left). And still, the channels have not been completed completely. He told me that you have very narrow and winding canals, plus 4 roots. The Russians used a different technology to fill the filling, but it surprisingly didn’t work too badly. Don't touch your teeth anymore. If inflammation occurs, you will have one way out - open the gum, bite off the tip of the root and fill it at the other end.